Robotic-arm-assisted patellofemoral arthroplasty is a viable surgical option in grossly distorted knee anatomy, such as in post-traumatic patellofemoral ankylosis.
Dr. Thadi Mohan, Department of Orthopedics, Amrita Institute of Medical Sciences, Amrita Vishwa Vidyapeetham, Kochi, Kerala, India. E-mail: thadimohan@gmail.com
Introduction: This case report describes the procedure and 2-year outcome in a patient with bony patellofemoral ankylosis who underwent robotic arm-assisted patellofemoral arthroplasty (RA-PFA).
Case Report: A 21-year-old male with Post-traumatic Patellofemoral Ankylosis with quadriceps contracture underwent RA-PFA with Quadriceps-plasty. Preoperatively, the patient had a flexion deformity of 20° with no further active flexion or extension. Passive knee extension from 20° to 0° was possible. At 2-year follow-up, he was independently ambulant with good improvement in pain and functional clinical scores. He had an improved active flexion of 0°–80° and active extension of 80°–0° with no extension lag.
Conclusion: This case suggests RA-PFA may be an effective intervention to restore knee function in Post-traumatic Patellofemoral Ankylosis despite the grossly altered anatomy.
Keywords: Osseous ankylosis knee, patellofemoral implant, robotic arm-assisted patellofemoral arthroplasty, quadriceps-plasty.
Knee stiffness resulting from patellofemoral ankylosis is a rare complication of high-energy trauma and poses a difficult challenge to the surgeon, as there is no established treatment protocol to date [1]. Post-traumatic stiffness of the knee in extension causes severe disability to the patient by interfering with activities of daily living. While patellectomy has been proposed as an alternative treatment, its unfavorable impact on quadriceps strength, leading to laxity and increased extensor lag, raises concerns [2,3]. An osteotomy of the patellofemoral fusion will inevitably lead to refusion, due to the cancellous surfaces exposed. Previous attempts at patellar resurfacing using fascia, fat pad, or skin patches have yielded unreliable results as well [4,5,6,7]. Patellofemoral arthroplasty (PFA) has gained recognition as an effective intervention for isolated patellofemoral arthritis, although its role in addressing Post-traumatic Patellofemoral Ankylosis remains undocumented.
We performed a robotic-arm-assisted PFA (RA-PFA) in a case of Post-traumatic Bony Patellofemoral Ankylosis, utilizing a 3D computed tomography (CT) based image for pre-operative planning. The patient had achieved excellent function at his 2-year follow-up. This approach aims to enhance procedural precision, ensuring accurate component placement, achieve normal patellar tracking, and ultimately contribute to improved functional outcomes.
A 21-year-old male presented with a stiff knee following a road traffic accident 5 years ago. He had sustained an open comminuted supracondylar fracture of the right femur (Type 3B), and a closed comminuted fracture of proximal third tibia. He subsequently underwent several procedures over the next month: Immediate wound debridement and knee spanning external fixation, delayed open reduction and internal fixation of femur and tibia, bone grafting, antibiotic bead insertion, local flap, and split skin grafting. At 2 years, after confirming bony union, implants were removed from the femur.
On arrival at our clinic, the patient had a body mass index of 22 kg/m2, reported right anterior knee pain and stiffness, and was ambulatory with support. Physical examination revealed healed surgical and wound scars with severe quadriceps wasting. The patient’s right knee had a flexion deformity of 20°, and the patient exhibited no further active or passive flexion beyond 20°. The patient had no active extension, though his knee could be passively extended to 0° (Video 1: Pre-operative knee flexion deformity of 20° with no further active flexion and extension.).
The observation of a motionless patella suggested ankylosis of the patellofemoral joint.
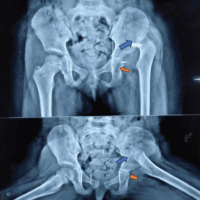
Long leg and lateral radiographs confirmed bony ankylosis of the patella (Fig. 1).

Figure 1: (a) Pre-operative long leg and lateral radiographs depicting deformed distal femur with ankylosed patellofemoral joint, (b) Pre-operative magnetic resonance imaging image of the right knee, showing only minimal cartilage thinning in the medial compartment.
The patient exhibited joint space narrowing in the medial compartment of the knee on radiographs; however, on magnetic resonance imaging (MRI), there was only minimal cartilage thinning (Fig. 1). Notably, a skyline patella view radiograph could not be obtained due to the existing deformity. We ruled out the possibility of infections since the total count and inflammatory markers were within the normal range, and the MRI showed no signs of infection. Given the distorted anatomy, RA-PFA using the MAKO Robot (Stryker, USA), complemented by a quadriceps-plasty procedure, was planned. 3D-CT scan was performed to facilitate precise pre-operative planning. A MAKO product specialist segmented the scans using the MAKO planning software. Since the patella was ankylosed, the patella and femur were taken en bloc for segmentation, unlike regular cases (Fig. 2).
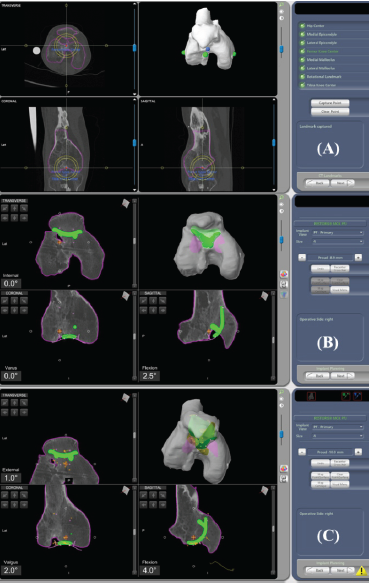
Figure 2: (a) Segmentation of femur and patella en bloc, (b) Pre-operative plan of the trochlear component size and position, (c) Implant position virtually adjusted.
Implant size and positioning were planned pre-operatively on the 3-D CT scan (Fig. 2). On the transverse plane, the largest trochlear implant was used without overhang, and in the sagittal plane, the implant tip was anterior to Blumensaat’s line. On the coronal view, the component was centered on the notch. Varus/valgus, flexion/extension, and external/internal rotation were adjusted as necessary within the recommended safe zone [8].
Surgical technique
The procedure was performed under spinal anesthesia with the patient in supine position using pneumatic tourniquet applied to the right thigh. Prophylactic doses of a second-generation cephalosporin and I.V. tranexamic acid were administered. A midline longitudinal incision over the previous scars and a medial parapatellar arthrotomy were done. Quadriceps-plasty was initially done to relieve contractures, releasing suprapatellar, lateral, and medial gutter adhesions and the lateral retinacular tissues. The quadriceps muscle fibers adherent to fracture site were meticulously released [9]. Two unicortical femoral pins were inserted onto the medial surface of the medial femoral condyle (MFC) and array fitted to face the robotic camera. A checkpoint was then inserted on the MFC. The limb was then rotated to locate the hip center, and the femur checkpoint was verified using the blunt probe. Bone registration involves touching forty points on the femur with a sharp probe, spaced 5 mm apart in all three planes to establish real-time communication between the robot and the patient’s right lower limb (Video 2: Bone registration involving collecting 40 points 5 mm apart).
The ankylosed patella was manually resected and subluxed, leaving a 15 mm remnant measured with a ruler to prevent excessive thinness that could lead to fracture during component fixation.
The subsequent step involved cartilage mapping, a critical procedure especially in cases with distorted anatomy, where identifying the true trochlear surface poses a significant challenge. The robot identified the trochlear groove, and 12 points were collected within it to complete the articular surface mapping (Video 3: Trochlear mapping).
Implant position was virtually adjusted for a seamless transition from the component to the mapped trochlear surface after registration (Fig. 2). Subsequently, the preparation of the femoral trochlea was undertaken using the robotic arm’s burr, cutting through the remaining portion of the resected patella to access the true trochlea (Video 4: Trochlear preparation using robotic arm’s bur.).
Utilizing a 6 mm burr attached to robotic arm, all green markings on the screen were meticulously removed. Three peg holes were drilled on the prepared articular surface using the robotic arm (Video 5: Drilling of three peg holes using robotic arm’s burr).
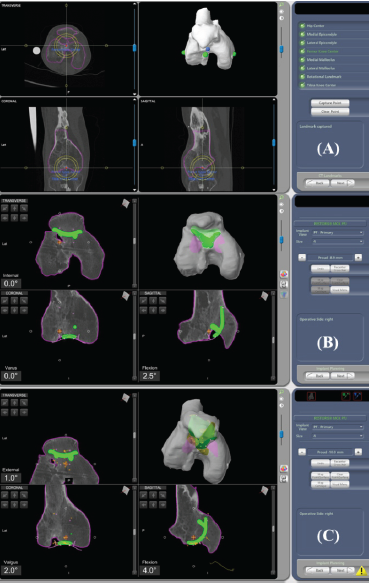
Figure 2: (a) Segmentation of femur and patella en bloc, (b) Pre-operative plan of the trochlear component size and position, (c) Implant position virtually adjusted.
The patella was resurfaced in the conventional manner. (Video 6: Drilling of peg holes for patella using patella drill guide).
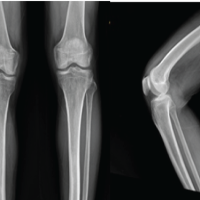
Patella tracking was checked manually and found acceptable. We achieved a passive flexion of 90° of the index knee during trialing of components (Fig. 3).
The Trochlear implant (size 4)was made of Cobalt Chromium Alloy & Patellar Dome (29mm) was Polyethylene (Fig. 3). The final implantation was performed with careful cement pressurization, and the joint was maintained in a stable position until the cement was set. After ensuring hemostasis, a meticulous layered wound closure was done.
Postoperatively, the patient was enrolled in a rehabilitation program consisting of continuous passive motion twice daily, patellar mobilization, quadriceps, and hamstring strengthening exercises. Intraoperative cultures from synovial fluid and synovial tissue had no growth.
At 2-year follow-up, the patient demonstrated improved gait and active knee flexion up to 80°; he had Grade 4 active knee extension with no lag (Fig. 3).

Figure 3: Measuring patella thickness before resection.
Kujala Score improved from pre-op 39/100 to 78/100 post-operative. Visual Analog Scale improved from pre-op 7/10–1/10 post-operative, indicating decreased pain. Oxford Knee Score improved from 22/48 to 41/48. Post-operative radiographs showed good implant positioning (Fig. 4). Patella Baja was not corrected, given the pre-existing quadriceps contracture. (Video 7: Patient climbing stairs independently at 2-year follow-up).

Figure 4: Post-operative active knee demonstrating flexion up to 90° and extension up to 20°, Post-operative (a) anteroposterior, (b) lateral, and (c) skyline view radiographs of the index knee.
The bony, ankylosed knee presents with a unique set of difficulties. The difficulties are in identifying normal anatomical landmarks, preparing bone surfaces, and achieving precise prosthesis placement [10,11]. Conventional cartilage mapping, as in regular robotic PFA cases, is not possible intraoperatively either.
We found 3-D CT-based pre-operative planning extremely useful in identifying the true trochlear surface in an ankylosed patella. It involved segmentation of the femur and patella en bloc due to the ankylosis. After bone registration, we resected and subluxed the patella and collected points using the probe around the trochlear groove to precisely locate the true articular surface. While preparing the trochlear surface, the robotic arm burred the patellar remnant and guided in drilling of peg holes on the exposed articular surface. This approach facilitated accurate implant positioning, ensuring optimal alignment within the recommended safe zone, thereby highlighting the dynamic capabilities of robotics in managing complex cases.
In the current case, we could mobilize the knee after releasing fracture-adherent muscles and quadriceps-plasty. Quadriceps snip or V-Y-plasty may have further weakened the quadriceps muscles. Another concern is the fracture risk when placing the threaded array pin in a relatively fragile femur. We minimized this risk by passing small 4 mm diameter pins through the metaphyseal portion, enabling quicker healing. Furthermore, we believe the risk of latent infections flaring up in patients with such a complex history can be minimized by careful patient selection and pre-operative planning using blood investigations and MRI to screen for signs for infection. In addition, intraoperative aseptic precautions, tissue cultures, and avoiding placing femoral array pins through the skin, but rather after opening the knee, can minimize further chances of post-operative infection.
RA-PFA may be preferred to a total knee arthroplasty in our young patient as a less radical, reconstructive procedure conserving cartilage menisci, cruciate ligaments, and bone stock, enabling faster rehabilitation. Long-term outcomes of RA-PFA for Post-traumatic Patellofemoral ankylosis, including implant survivorship, are yet to be evaluated.
RA-PFA (with quadriceps-plasty) is a viable intervention in post-traumatic patellofemoral ankylosis, provided the tibiofemoral compartment is spared. The short-term surgical outcomes are promising.
• Planning for conventional PFA in a grossly altered knee anatomy, as in this case of post-traumatic patellofemoral ankylosis, is challenging.
• We adapted the pre-operative planning to the altered anatomy, using the 3D-CT imaging of an existing robotic system, to gain precise planes of bone cuts and implant positions.
• Two-year outcomes are promising, with the patient able to mobilize independently, with no radiographic signs & no sign of implant loosening.
References
- 1. Sharma M, Sharma S, Upadhyaya AR. Classification-based management of stiff/ankylosed knees. Indian J Orthop 2021;55:1158-74. [Google Scholar] [PubMed]
- 2. Baker CL, Hughston JC. Miyakawa patellectomy. J Bone Joint Surg Am 1988;70:1489-94. [Google Scholar] [PubMed]
- 3. Günal I, Karatosun V. Patellectomy: An overview with reconstructive procedures. Clin Orthop Relat Res 2001;389:74-8. [Google Scholar] [PubMed]
- 4. Cave EF, Rowe CR. The patella: Its importance in derangement of the knee. J Bone Joint Surg Am 1950;32:542-3. [Google Scholar] [PubMed]
- 5. Judet R, Judet J, Lord G, Roy-Camille R, Boutelier P. Patelloplasty with preserved skin. Presse Med 1962;70:983-6. [Google Scholar] [PubMed]
- 6. Koga Y, Kono S, Mabuchi K. A long term follow up of resection interposition arthroplasty of the knee using chromicized fascia lata. Int Orthop 1988;12:9-15. [Google Scholar] [PubMed]
- 7. Oztuna V, Karatosun V, Unver B, Ayan I, Kuyurtar F. An alternative patellar resurfacing technique in knee replacement: Patellofemoral fascial interposition arthroplasty. Knee Surg Sports Traumatol Arthrosc 2007;15:1210-4. [Google Scholar] [PubMed]
- 8. Selvaratnam V, Toms AD, Mandalia VI. Robotic assisted patellofemoral joint replacement: Surgical technique, tips and tricks. Indian J Orthop 2022;56:2110-8. [Google Scholar] [PubMed]
- 9. Judet R, Judet J, Lagrange J. Treatment of pseudarthrosis by simple bone compression. Memoires. Acad Chir (France) 1956;82:402-5; discussion, 405-7. [Google Scholar] [PubMed]
- 10. Ferrari MB, Zago MK, de Castro JV, Gomes JL. Patellofemoral ankylosis: Case report and technical note. Arch Orthop Trauma Surg 2020;140:1977-83. [Google Scholar] [PubMed]
- 11. Belkin NS, Zelenski N, Mehta S, Kelly JD. Post-traumatic patellofemoral joint ankylosis. Univ Pennsylvania Orthop J 2015;25:38-40. [Google Scholar] [PubMed]
We would like to thank Dr. Manu Pradeep, MM Medical Research, Cherthala, India for assisting with manuscript writing.