Girdlestone resection arthroplasty is a salvage procedure for the hip, involving the removal of the femoral head and neck to control infection and relieve pain, often resulting in a fibrous pseudarthrosis and instability. This article describes a novel technique of improving stability following Girdlestone resection arthroplasty.
Dr. Mohit Asthana, Department of Orthopaedics, Marengo Asia Hospitals, Gurugram, Haryana, India. E-mail: mohitdb92@gmail.com
Introduction: The Girdlestone procedure is one of the options for treating an infected hip arthroplasty. It is a surgical procedure that involves resection of the head and neck of the femur, resulting in pseudarthrosis of the hip joint. This is often kept as a last resort for patients with significant co-morbidities or when other treatments have been ineffective. This procedure should be considered a salvage procedure, primarily aimed at pain relief and infection control.
Case Report: We report a case of a 73-year-old male who sustained a fracture of the neck of the femur in 2019 and was operated on multiple times for the same. He presented to us with an unstable hip.
Conclusion: We used a novel technique of Girdlestone resection arthroplasty, which involved stabilization of the proximal femur with Prolene mesh.
Keywords: Total hip arthroplasty, Girdlestone, infected total hip arthroplasty, unstable hip.
Management of infected total hip arthroplasty (THA) has always been a challenging task for surgeons. There are several options widely reported in literature for the treatment of an infected hip arthroplasty: Antibiotics, antibiotics plus debridement, resection-arthroplasty (Girdlestone procedure), one-stage exchange, or two-stage exchange. Gathorne Robert Girdlestone described the technique of head and neck resection of the femur in 1928 for the treatment of tuberculosis of the hip joint [1]. The modern Girdlestone procedure is used primarily for the treatment of peri-prosthetic joint infection (PJI) in the setting of failed THA [2,3,4,5,6]. In such cases, this procedure may be used as part of a two-stage revision arthroplasty procedure in which a new prosthesis is later fitted to the patient [7]. It may also be used for definitive treatment in THA failure cases that are not suitable for revision [8]. This case reports a novel technique of stabilization of the proximal femur using Prolene mesh in Girdlestone resection arthroplasty in a patient with failed THA due to infection.
A 73-year-old male presented to us with pain in the right hip and difficulty in walking for the last 5 years. He had a history of a road traffic accident in 2019 and sustained a fracture of the neck of the femur on the right side. He was managed with closed reduction and internal fixation with cancellous cannulated screws at a hospital elsewhere. The patient had complaints of pain and was unable to bear weight on his right lower limb even after the surgery. In 2020, THA was done at yet another hospital. The patient then developed a surgical site infection. Debridement and prosthesis removal were done, but the infection still persisted, and he developed a pus-discharging sinus. Multiple debridements were done thereafter at different hospitals.
In early 2024, the patient was referred to a hospital where debridement was done again, along with an intramedullary antibiotic nail. The patient then presented to us in November 2024 with pain and instability of the right hip joint, along with shortening of the right lower limb.
On examination, a large scar healed by secondary intention was present over the posterolateral and posterior aspect of the right hip. There was no active discharge. The greater trochanter was felt proximally and laterally. Although there was no local rise of temperature, tenderness was present over the proximal aspect of the femur, which appeared to impinge on the lateral aspect of the proximal thigh. Flexion was restricted to 90° while both internal and external rotations were exaggerated. The right lower limb was shortened by around 4 inches. The telescopy test was positive. All these findings pointed toward a painful and unstable hip.
X-rays of the pelvis with both hips-anteroposterior view (Fig. 1) showed proximal and lateral migration of the proximal femur on the right side with an antibiotic nail in situ. A computed tomography (CT) scan was done to delineate the anatomy of the acetabulum and femur (Fig. 2).
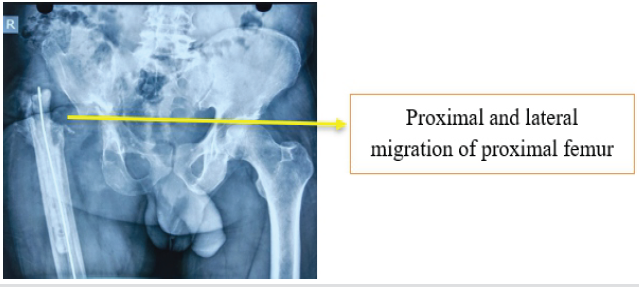
Figure 1: Pre-operative X-ray pelvis with both hips – anteroposterior view.
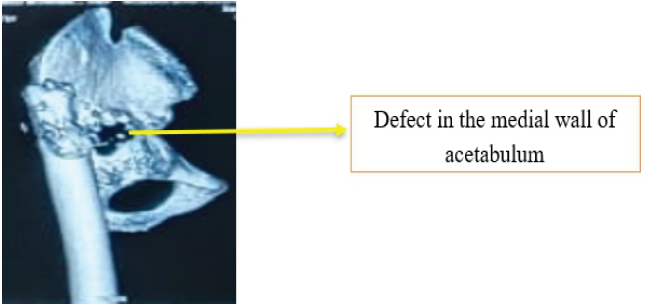
Figure 2: Computed tomography scan (right hip joint).
The patient was planned for elective surgery. Consent was taken, explaining that THA might not be possible as per the CT reports, which showed a very shallow and small acetabulum. In that case, debridement and removal of the antibiotic nail would be done. Surgically, the patient was placed in the lateral position. Using the posterior approach, a standard curved incision was made, and all the fibrous tissue was debrided. There were no signs of infection. However, a lot of fibrous tissue was encountered during deep dissection. The antibiotic spacer was removed from the canal. The acetabulum was identified with an image intensifier due to overgrowth of fibrous tissue. Fibrous tissue was cleared, and reaming was done with a No. 36 reamer. Acetabular bone stock was found to be scanty, due to which further reaming could not be done to accommodate the prosthesis shell or cage (Fig. 3). At this point, we decided not to go ahead with revision THA (Fig. 3).
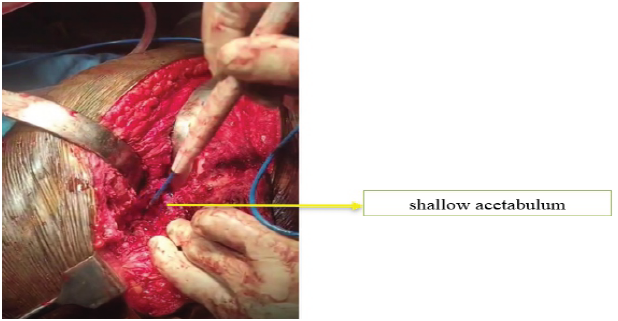
Figure 3: Intra-operative figure of shallow acetabulum – Right Hip.
Bursa over the protruded part of the proximal femur was debrided as it was thought to be the cause of tenderness over the skin laterally. Rough bone was trimmed and smoothened (Fig. 4).
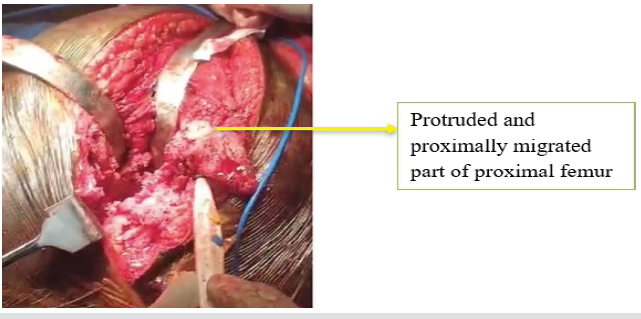
Figure 4: Intra-operative figure of the proximal femur.
A Prolene mesh was used to cover the proximal aspect of the femur, which was secured to muscles and capsule medially using Ethibond sutures (Fig. 5).
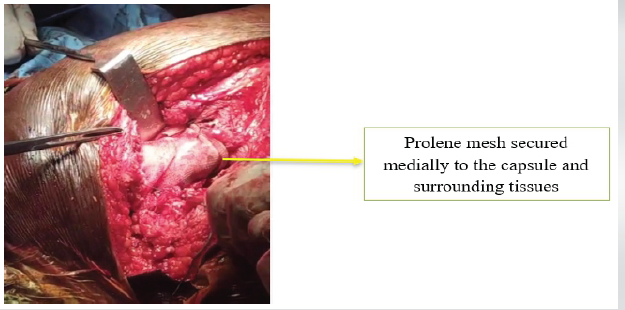
Figure 5: Intra-operative figure of the proximal femur with Prolene mesh.
Stability of the proximal femur was checked on the table, where decreased lateral and proximal migration was confirmed. Thorough lavage was given, and closure was done in layers. Antibiotics and deep vein thrombosis management were started prophylactically.
On post-operative radiograph, we drew a line from the tear drop to the proximal-most aspect of the femur and compared it with the pre-operative radiograph showing medialization and distalization of the proximal femur as compared to the pre-operative status (Figs. 6 and 7).
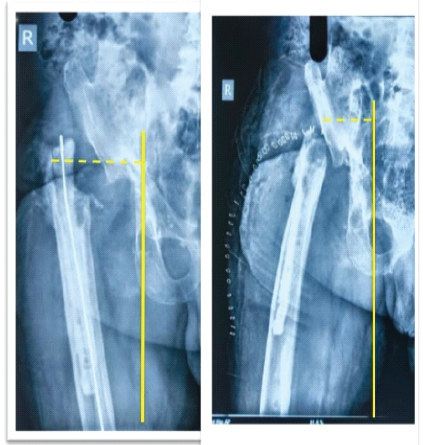
Figure 6, 7: Comparison of pre-operative and post-operative radiographs showing medialization of the proximal femur.
The patient was mobilized the next day on full weight bearing with walker support and with a shoe raise to compensate for limb shortening (Fig. 8).

Figure 8: Post-operative day 1 figure of patient mobilization with the help of a walker.
The Girdlestone procedure is indicated when getting control of infection is difficult and the condition of soft tissue and bone is not good enough to implant a new prosthesis, and various medical co-morbidities, where an extensive surgical procedure is contraindicated [2].
The result of this procedure is usually a painless hip joint, but pain may still persist in some patients. The walking ability of the patient is limited after the procedure.
In this case, we decided to perform Girdlestone resection arthroplasty since the acetabular bone stock was deficient and it was very shallow to accommodate a shell or cage. Performing THA in a case where the Girdlestone procedure was already done in the past is technically challenging.
PJI can also be managed with the implantation of an antibiotic cement spacer. Cement spacers are associated with various complications such as dislocation, fracture, further loss of bone stock, and development of resistant strains of bacteria. Thus, the Girdlestone procedure is the preferred method for treatment in cases of deficient bone stock as well as in cases where infection is very difficult to completely eradicate.
The walking pattern and energy expenditure were analyzed in patients undergoing resection arthroplasty by Waters et al. [9]. They reported that the majority of patients required walker support or crutches, and their walking speed was also slowed down.
As per the study done by Sharma and Kakar, all the patients required assistance for mobilization, unlike the report in some publications that 50% of the patients were able to walk without any assistance [10].
In this case report, the patient had already undergone multiple surgeries, which had a significant impact on his physical and mental health. His main concern was pain in the right hip, which was due to the tenting of soft tissues around the hip due to instability. We brought down the proximal femur to its anatomic location by stabilizing it with a Prolene mesh. Pain was significantly reduced in the post-operative period, and the patient could mobilize with walker support. Limb shortening was compensated with a shoe raise.
The Girdlestone resection arthroplasty is a salvage procedure; the aim of the technique is to reduce the instability of the proximal femur by efficiently stabilizing it with a Prolene mesh. It is a simple, straightforward, and cost-effective method to secure the proximal femur with the joint capsule and surrounding soft tissues. Thus, issues such as pain, instability, and complications due to instability, such as skin complications and impingement, can all be addressed by this novel technique. While Girdlestone may hamper the joint stability and cause limb length shortening, it can only be used in patients with severe pain who cannot undergo hip arthroplasty.
Reinforcement of the proximal femur with Prolene mesh during Girdlestone resection arthroplasty is a simple and cost-effective technique that provides added stability and soft-tissue support, facilitating early mobilization and improved functional outcome.
References
- 1. Girdlestone GR. Acute pyogenic arthritis of the hip: An operation giving free access and effective drainage. Lancet 1943;241:419-21. [Google Scholar] [PubMed]
- 2. Vincenten CM, Gosens T, Van Susante JC, Somford MP. The Girdlestone situation: A historical essay. J Bone Jt Infect 2019;4:203-8. [Google Scholar] [PubMed]
- 3. Sawadogo M, Kafando H, Ouedraogo S, Korsaga AS, Ouedraogo S, Tinto S, et al. Is head and neck resection of the femur (Girdlestone’s Procedure) still relevant? Indications and results about 24 cases. Open Orthop J 2018;12:69-74. [Google Scholar] [PubMed]
- 4. McElwaine JP, Colville J. Excision arthroplasty for infected total hip replacements. J Bone Joint Surg Br 1984;66:168-71. [Google Scholar] [PubMed]
- 5. Petty W, Goldsmith S. Resection arthroplasty following infected total hip arthroplasty. J Bone Joint Surg Am 1980;62:889-96. [Google Scholar] [PubMed]
- 6. Ahlgren SA, Gudmundsson G, Bartholdsson E. Function after removal of a septic total hip prosthesis. A survey of 27 girdlestone hips. Acta Orthop Scand 1980;51:541-5. [Google Scholar] [PubMed]
- 7. Vincenten CM, Den Oudsten BL, Bos PK, Bolder SB, Gosens T. Quality of life and health status after Girdlestone resection arthroplasty in patients with an infected total hip prosthesis. J Bone Jt Infect 2019;4:10-5. [Google Scholar] [PubMed]
- 8. Castellanos J, Flores X, Llusà M, Chiriboga C, Navarro A. The Girdlestone pseudarthrosis in the treatment of infected hip replacements. Int Orthop 1998;22:178-81. [Google Scholar] [PubMed]
- 9. Waters RL, Perry J, Conaty P, Lunsford B, O’Meara P. The energy cost of walking with arthritis of the hip and knee. Clin Orthop Relat Res 1987;214:278-84. [Google Scholar] [PubMed]
- 10. Sharma H, Kakar R. Outcome of Girdlestone’s resection arthroplasty following complications of proximal femoral fractures. Acta Orthop Belg 2006;72:555-9. [Google Scholar] [PubMed]