Fungal osteomyelitis due to Histoplasma capsulatum can occur even in immunocompetent individuals; early diagnosis and combined surgical and antifungal therapy are key to successful management.
Dr. S Vishnu, Department of Orthopaedic Surgery, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: rollsroycevishnu95@gmail.com
Introduction: Histoplasma capsulatum is a thermally dimorphic fungus that is endemic to North and Central America and rarely encountered in Asia. Musculoskeletal involvement is uncommon, particularly in immunocompetent individuals. This report presents a rare case of localized histoplasmosis osteomyelitis involving two skeletal sites in an immunocompetent patient.
Case Report: A 53-year-old immunocompetent female presented with a 6-month history of chronic, multifocal osteomyelitis involving the right lateral malleolus and left ring finger. She had no systemic symptoms or history suggestive of immunosuppression. Radiographs revealed osteolytic lesions, and histopathological examination demonstrated granulomatous inflammation with fungal spores confirmed by periodic acid-Schiff and Gomori Methenamine Silvers staining, consistent with H. capsulatum. The patient underwent surgical debridement with autologous cancellous bone grafting and temporary external fixation. Post-operatively, she received intravenous Amphotericin B for 6 weeks, followed by a period of protected mobilization. At 1-year follow-up, the patient had complete recovery with no evidence of recurrence.
Conclusion: Localized histoplasmosis osteomyelitis in an immunocompetent host is extremely rare and may mimic bacterial osteomyelitis. A high index of suspicion, timely histopathological diagnosis, and appropriate antifungal therapy combined with surgical management are essential for optimal outcomes.
Keywords: Histoplasma capsulatum, histoplasmosis osteomyelitis, immunocompetent, amphotericin B, antifungal therapy, bone infection.
In North and Central America, the thermally dimorphic fungus Histoplasma capsulatum is endemic. In immunocompetent individuals, exposure to the bacterium simply causes an asymptomatic infection; in immunocompromised individuals, it can result in lethal disseminated fungemia [1].
Although the organism is widespread, histoplasmosis cases are uncommon in Asia. Extrapulmonary histoplasmosis is an acquired immunodeficiency syndrome (AIDS)-defining illness in HIV-positive individuals, but still only rarely involves the musculoskeletal system [2,3]. Only a few cases of H. capsulatum infection in the bone have been documented in the past few decades.
One patient, who showed no symptoms of a persistent illness or abnormal immune function, was diagnosed and treated for histoplasmosis osteomyelitis that had spread to two bones. We monitored the patient for a year, and she experienced no negative outcomes. We provide this case report to discuss about our knowledge in the diagnosis and treatment of Histoplasmosis osteomyelitis.
A 53-year-old female presented with multifocal signs of chronic osteomyelitis, 6 months duration, that is, Fig. 1: Over the right ankle lateral aspect and Fig. 2: Left hand ring finger with no systemic features of infection. It was associated with pain and progressive difficulty in walking.

Figure 1: Discharging ulcer over the left ankle (lateral).

Figure 2: Discharging wound over the left ring finger.
There was no history of fever/exposure to TB/chronic systemic diseases (Type 2 Diabetes Mellitus) or any significant history of chronic diseases in the past.
Physical examination revealed the patient to be cooperative, well oriented to time, place, and person, moderately built and nourished. There was no pallor, local or generalized lymphadenopathy and edema was absent. There were no systemic signs of immunocompromise. Other systemic examination was within normal physiological limits.
A swelling was noted over the left lateral malleolus 4 × 4 cm size with erythema over the surrounding skin, induration was present. It was firm in consistency and the skin was not pinchable. The swelling was not mobile, tenderness was present and ankle range of motion was near normal. There was no distal neurovascular deficit.
Another swelling noted over the left ring finger distal interphalangeal joint of 1 × 2 cm with surrounding erythema and induration. The swelling was not mobile but a discharging sinus was present (seropurulent). The range of motion at the distal interphalangeal joint was 10–30° flexion.
The patient was evaluated radiologically and routine blood investigations were sent. Laboratory testing indicated a blood white cell count of 8.6 × 109/L, with neutrophils accounting for 58.3% and lymphocytes for 31.6%. The hematocrit was 36.0%. The Erythrocyte sedimentation rate was 62 and C-reactive protein was 24. She was negative for anti-human immunodeficiency virus, anti-syphilis, and anti-hepatitis C virus antibodies, anti-hepatitis A virus immunoglobulin, and hepatitis B surface antigen. The concentration of serum alkaline phosphatase was 226 U/L, slightly higher than the cutoff for abnormal values: >140 U/L), and total bilirubin was 0.19 mg/dL, which was lower than the cutoff value of 0.30 mg/dL. The concentrations of plasma electrolytes, creatinine, urea nitrogen, and albumin were within normal ranges.

Figure 3: Anteroposterior and lateral views of the left ankle when the patient presented to the outpatient department showing an osteolytic lesion of the lateral malleolus.

Figure 4: X-ray of the left hand in anteroposterior view – soft tissue shadow noted over the distal phalanx of the ring finger.
On radiological evaluation Figs. 3 and 4: An osteolytic lesion was noted over the lateral malleolus, not well demarcated edges, no sclerosis and joint space was maintained. The lateral cortical bone was intact.
Surgery
The lateral cortical bone was intact, and that the subcortex was filled with brown fleshy tissue 3 × 2 × 2 cm in size. The lesion tissues and narrow margin -scraped using a curette, and the tissue cavity – treated sequentially with carbolic acid, alcohol, and hydrogen peroxide as chemical cauterization.
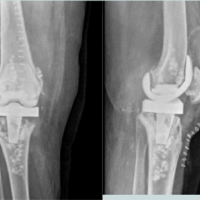
Bone graft (autologous cancellous) was harvested from the iliac crest and filled inside the defect. Fig. 5: Temporary stabilization was done with an external fixator (delta frame).

Figure 5: Delta frame applied after debridement.
Histology
Fig. 6: Round and oval spores; granulomatous inflammatory cells in the lesion tissue sections, Fig. 7 and 8: Positive periodic acid-Schiff staining and periodic acid methenamine-silver staining negative smear for acid-fast staining, indicating H. capsulatum.
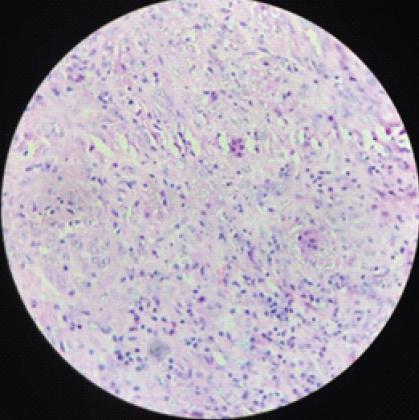
Figure 6: H&E section ×40:- Fibrocollagenous tissue showing mixed inflammatory cells and plenty of histiocytes with organism in their cytoplasm and new foreign body giant cells.

Figure 7: Special stain for confirmation – periodic acid-Schiff (PAS) stain, ×40 PAS positive – fungal organism.
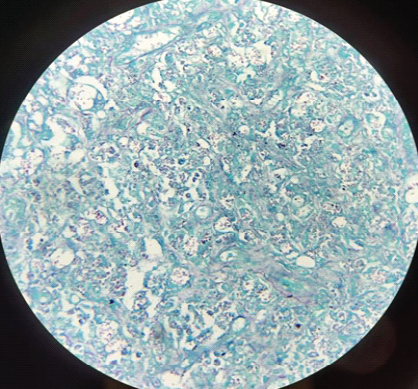
Figure 8: Special stain for confirmation, Gomori Methenamine Silvers (GMS) stain, ×40 GMS + for fungal organism.
Treatment
Thorough debridement of the infected tissue was done with a curette, till fresh bleeding was noted. Autologous bone graft was given and temporary stabilization with an external fixator was given. The patient was started on Amphotericin B for 6 weeks. Patient was advised non-weight-bearing walking (walker-assisted) for 3 weeks. (Fig. 9).
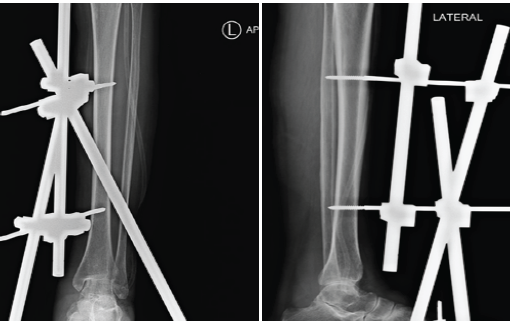
Figure 9: Six-weeks post-operative X-ray of the left ankle.
Bacterial pathogens, primarily Staphylococcus, remain the most common cause of subacute osteomyelitis in immunocompetent individuals, but mycotic infection does occur infrequently [4].
Histoplasmosis is brought on by H. capsulatum infection, which typically happens in the lungs. The soil serves as H. capsulatum’s environmental reservoir [5]. People obtain Infection with H. capsulatum generally occurs through breathing conidial forms of the organism that are present in the environment, including soil that has been exposed to chickens, birds, or bat excrement, and can infect humans when its spores are aerosolized [5,6,7]. The severity of the primary infection depends on several factors, including the size of the inoculum, the immune status of the host, and the virulence of the infecting strain [8]. In our case, the infection’s source was obscure. She claimed she had no recent travel history, lived in the countryside, and worked daily in the fields. She might have picked up the H. capsulatum infection in the fields. Immunocompetent subjects who become infected with H. capsulatum typically experience asymptomatic or moderate flu-like infections with fever, headache, malaise, coughing, and chest pain that spontaneously go away after a few days. For several years, infected people can harbor H. capsulatum. Disseminated histoplasmosis, which can affect the lungs, central nervous system, liver, spleen, and rheumatologic, ocular, and hematologic systems, can occur in a patient who has become immunosuppressed. Patients with histoplasmosis in the muscle and bone tissues, however, are incredibly uncommon [9]. There are very few cases of bone histoplasmosis reported, of which it’s mostly disseminated in immunocompromised hosts. Reported cases of lower limb bone histoplasmosis and localized lesions in immunocompetent host is rarest [10].
To repair a solid distal tibiofibular syndesmosis and ankle joint, the patient’s surgical cavity was filled with homologous cancellous bone rather than bone cement or antibacterial beads. Indeed, physical examination and radiographic scans have shown that the function and structure of the surgically repaired muscles and bone structures have fully recovered. The patient was able to engage in both routine and demanding activities. The medications for the treatment of histoplasmosis were listed as being itraconazole and amphotericin B [11].
Amphotericin B is a widely used medication for treating people with life-threatening illnesses [12], although it can occasionally have serious side effects with close monitoring of renal functions. Patients who are immunocompromised (AIDS) should receive amphotericin B as induction therapy for disseminated histoplasmosis and either amphotericin B or an oral azole antifungal medication (itraconazole) as maintenance therapy [13].
Itraconazole (200 mg once or twice daily for 6–12 months) is the drug of choice for mild and isolated disease [6,14,15,16,17] and can be used for both the induction and maintenance phases of treatment for disseminated histoplasmosis. Itraconazole’s labeling states that there is not adequate support for its usage in children. A safe option is voriconazole, a conazole with clear labeling and instructions for usage in teenagers [4]. The follow-up results showed that the prognosis was quite positive.
As a summary, we describe a rare instance of localized histoplasmosis osteomyelitis that lacked immunocompromise. Using routine radiological exams, this condition was difficult to diagnose. For the control of infection and functional recovery, we discovered that surgical excision of the lesion, local treatment with autologous bone transplantation, and systemic treatment with antibiotics were all beneficial. In patients who cannot take itraconazole, fluconazole (400 mg–800 mg daily) is an alternative [14,17].
Histoplasmosis capsulatum is a rare cause of localized osteomyelitis the diagnosis of the histoplasmosis was initially not suspected and she was receiving emperical antiobiotics for the same until culture showed growth of H. capsulatum fungus.
Histoplasmosis osteomyelitis can occur even in immunocompetent individuals and may mimic bacterial infection; a high index of suspicion, prompt diagnosis with combined surgical debridement and antifungal therapy ensures optimal outcomes.
References
- 1. Chang P, Rodas C. Skin lesions in histoplasmosis. Clin Dermatol 2012;30:592-8. [Google Scholar] [PubMed]
- 2. Yee AC, Huang S, Singh R, Rizzi D, Shama N, Khoury N, et al. Disseminated histoplasmosis in an HIV/AIDS transgender male-to-female with atypical and persistent GI manifestations. JGH Open 2023;8:e13011. [Google Scholar] [PubMed]
- 3. Agarwal V, Chauhan S, Gupta RK. Pyomyositis. Neuroimaging Clin N Am 2011;21:975-83, x. [Google Scholar] [PubMed]
- 4. Mittal J, Ponce MG, Gendlina I, Nosanchuk JD. Histoplasma capsulatum: Mechanisms for pathogenesis. Curr Top Microbiol Immunol 2019;422:157-91. [Google Scholar] [PubMed]
- 5. Fischer GB, Mocelin H, Severo CB, Oliveira FD, Xavier MO, Severo LC. Histoplasmosis in children. Paediatr Respir Rev 2009;10:172-7. [Google Scholar] [PubMed]
- 6. Larsen SØ, Bodilsen J, Mørn B. Disseminated Histoplasma captulatum infection in a patient with HIV. Ugeskr Laeger 2024;186:V03240205. [Google Scholar] [PubMed]
- 7. Huang L, Wu Y, Miao X. Localized Histoplasma capsulatum osteomyelitis of the fibula in an immunocompetent teenage boy: A case report. BMC Infect Dis 2013;13:132. [Google Scholar] [PubMed]
- 8. Harnalikar M, Kharkar V, Khopkar U. Disseminated cutaneous histoplasmosis in an immunocompetent adult. Indian J Dermatol 2012;57:206-9. [Google Scholar] [PubMed]
- 9. Wheat LJ, Cloud G, Johnson PC, Connolly P, Goldman M, Le Monte A, et al. Clearance of fungal burden during treatment of disseminated histoplasmosis with liposomal amphotericin B versus itraconazole. Antimicrob Agents Chemother 2001;45:2354-7. [Google Scholar] [PubMed]
- 10. Noor A, Preuss CV. Amphotericin B. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/nbk482327 [Last accessed on 12 Aug 2025].. [Google Scholar] [PubMed]
- 11. McKinsey DS. Treatment and prevention of histoplasmosis in adults living with HIV. J Fungi (Basel) 2021;7:429. [Google Scholar] [PubMed]
- 12. Kurn H, Wadhwa R. Itraconazole. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/nbk557874 [Last accessed on 15 Nov 2025]. [Google Scholar] [PubMed]
- 13. Ramos JT, Romero CA, Belda S, Candel FJ, Carazo Gallego B, Fernández-Polo A, et al. Clinical practice update of antifungal prophylaxis in immunocompromised children. Rev Esp Quimioter 2019;32:410-25. [Google Scholar] [PubMed]