The key learning point of this report is the recognition of a rare vascular complication after a Girdlestone procedure and the critical importance of timely diagnosis, rapid intervention, and coordinated team communication in achieving favorable patient outcomes.
Mr. Daanish Sheikh, Department of Orthopaedics, UT Health San Antonio, San Antonio, Texas. E-mail: sheikhd1@livemail.uthscsa.edu
Introduction: Girdlestone excision arthroplasty is a surgical procedure for managing severe hip joint pathology, involving the removal of the femoral head and neck. Despite its utility, the Girdlestone procedure carries significant risks, including vascular complications. This report highlights a previously unreported complication: Post-operative hemorrhage from the superior gluteal artery (SGA).
Case Report: A 65-year-old female underwent this procedure after recurrent infections and instability following hip hemiarthroplasty. The patient who underwent a Girdlestone procedure experienced life-threatening hemorrhage likely due to excessive external rotation and femoral shortening during post-operative transfer. A computed tomography scan revealed active SGA extravasation, necessitating emergent embolization by interventional radiology.
Conclusion: There are currently no reported cases of this event occurring in the literature. This case underscores the need for vigilance in post-operative monitoring for vascular complications, particularly in high-risk patients. This report emphasizes the importance of recognizing and promptly addressing vascular injuries, as well as prioritizing care-team communications, to improve patient outcomes.
Keywords: Orthopedics, Girdlestone, prosthetic joint infection, hip fracture, arthroplasty, superior gluteal artery.
Girdlestone excision arthroplasty is a surgical procedure performed primarily for the management of severe hip joint pathology. This technique involves the removal of the femoral head and neck, resulting in a flail hip. The procedure is indicated for severe infections of the hip joint, especially when management does not respond to conservative treatment or revision surgeries. Sharma et al. [1] elaborated on its utility in managing recurrent dislocations and severe osteoarthritis, particularly in patients who are poor candidates for more complex reconstructive procedures. Furthermore, Condell et al. [2] highlight Girdlestone’s role in situations where patients have significant bone loss or poor bone stock that precludes successful reconstruction.
Girdlestone excision arthroplasty is associated with several potential complications including leg length discrepancy, prolonged use of mobility aids, persistent pain, and the potential for recurrent infections. Vascular complications, although rare, can be severe, as illustrated by Pasquinelly and Andrews, [3] who reported a case of profunda femoris pseudoaneurysm leading to fatal hemorrhage 2-week post-surgery. Calligaro et al. [4] emphasized the potential for acute arterial complications, such as thrombosis or embolism, associated with hip surgeries, underscoring the need for vigilant post-operative monitoring.
Here, we report the case of a patient who experienced life-threatening hemorrhage from the superior gluteal artery (SGA) following incision and drainage (I&D) of a hip with recurrent infections that had previously been treated with Girdlestone resection arthroplasty. This case highlights a previously unreported serious and preventable complication following the Girdlestone procedure in the setting of sharp greater trochanteric remodeling.
June 22, 2023
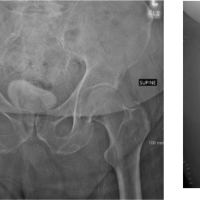
A 65-year-old female with a history of non-alcoholic steatohepatitis (NASH), stroke, pancytopenia, hypertension, aortic stenosis, uncontrolled type 2 diabetes, and obesity was brought to the emergency department (ED) after a fall onto her right hip. She was independent but used a walker at baseline. She sustained a right femoral neck fracture (Fig. 1). The orthopedics team recommended a right hip hemiarthroplasty due to the patient’s underlying medical conditions.
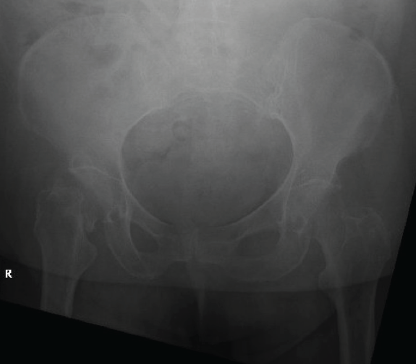
Figure 1: Anterior-posterior X-ray of right femoral neck fracture.
June 23, 2023
The patient underwent right hip hemiarthroplasty (Fig. 2). A standard anterolateral approach was utilized. The femoral stem was cemented, a standard neck +3 bipolar head was used, and good intraoperative stability and length were confirmed. Due to a platelet count of 42 and hemoglobin of 8, she was given platelets and packed red blood cells (PRBCs) intraoperatively. She tolerated this surgery well. She was weight bearing as tolerated (WBAT) postoperatively.
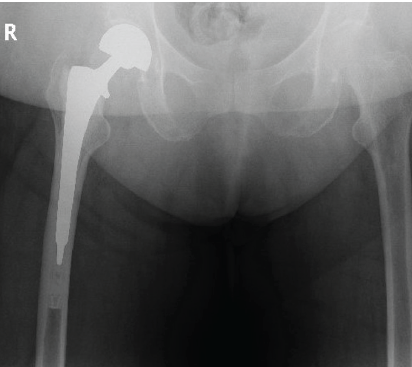
Figure 2: Anterior-posterior X-ray depicting right hip hemiarthroplasty.
June 29, 2023
The patient had difficulty mobilizing with physical therapy (PT) and was discharged to a skilled nursing facility (SNF).
July 07, 2023
The patient had a fall from standing at her SNF while ambulating independently. She developed pain and decreased independence.
July 10, 2023
The patient returned to the ED due to an altered mental status, presenting with purulent drainage from a right hip wound. A shortened, painful, and internally rotated extremity was noted. Blood cultures grew Klebsiella. Imaging confirmed a posteriorly dislocated hemiarthroplasty (Fig. 3). The orthopedic team recommended open reduction with single-stage I&D and head-ball exchange due to the acute nature of the prosthetic joint infection (PJI) and chronic nature of the dislocation.
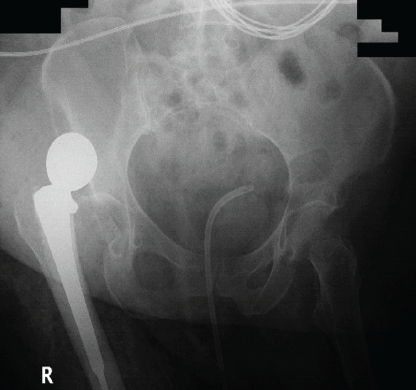
Figure 3: Anterior-posterior X-ray of initial posteriorly dislocated hemiarthroplasty.
July 13, 2023
The patient underwent I&D of the right hip with a head-ball exchange. The old incision was used, and purulent fluid was found to track down to the hip joint. The tip of her greater trochanter was found to be avulsed from the femur. The hip was reduced and was stable to full range of motion. Vancomycin and tobramycin powder with procoagulant were placed in the wound before closure. An incisional Prevena Wound-VAC dressing was placed for soft tissue healing. She was made non-weight bearing to her right lower extremity, strict posterior hip precautions were placed, and infectious disease (ID) was consulted for antibiotic recommendations.
July 19, 2023
The patient was discharged to a SNF.
August 07, 2023
The patient presented to the ED and was admitted to the intensive care unit (ICU) for a bleeding and dehiscent right hip wound, severe hypotension (91/35), and altered mental status. She was started on pressors and emergently transfused. The patient was found to have sanguinopurulent drainage and a recurrent posteriorly dislocated right hip. A right hip Girdlestone resection arthroplasty was recommended, considering the recurrent instability, infection, and poor clinical condition.
August 17, 2023
Following initial hesitance due to the risk of intraoperative mortality, the patient consented to a Girdlestone procedure (Fig. 4).
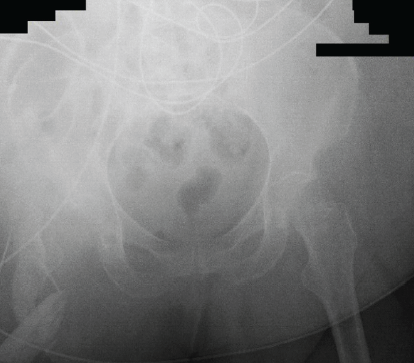
Figure 4: Post-operative Anterior-posterior X-ray of the pelvis following Girdlestone excision arthroplasty.
The old incision was reopened with a significant hematoma but no gross purulence. An I&D was performed, and all orthopedic implants, including a difficult cemented femoral component, were removed. Flexible osteotomes were utilized with multiple proximal osteotomies performed. No intraoperative fracture occurred. The hip was reduced under fluoroscopy and was stable with full range of motion. Vancomycin and tobramycin powder with procoagulant were placed in the wound and closed in standard fashion. An incisional Wound-VAC dressing was placed for soft tissue healing. The patient was made WBAT with a full range of motion.
August 21, 2023
The patient was discharged to an SNF.
August 25, 2023–October 04, 2023
The patient returned to the ED two times during this period with continued non-odorous serosanguinous drainage from her right hip wound. Wound care was consulted, and she was transitioned to formal Wound-VAC for secondary intention healing. The wound decreased from 1.5 × 1.0 × 10 cm to 1.0 × 1.0 × 2.0 cm and she was transitioned to packing.
February 03, 2024
The patient returned to the ED with increased pain and purulent drainage (Fig. 5). She remained pancytopenic with platelets of 59, hemoglobin of 8.7, and elevated coagulation laboratories. The orthopedic team recommended a formal right hip I&D.
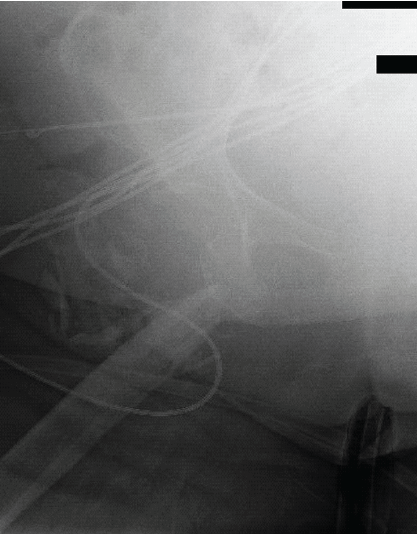
Figure 5: Anterior-posterior X-ray of the right hip upon readmission before second incision and drainage. Note the sharp spike of the greater trochanter.
February 04, 2024 9:00 am
The patient was taken for right hip I&D and given 1 gram of tranexamic acid before incision. A wide excision of her draining sinus tract was performed. Dissection down to the level of the joint and remaining proximal femur bone was performed, with a void of fascial tissue in this area. Her draining sinus tract went down to the level of the joint and bone. Purulent fluid was noted, and cultures were taken. The wound was irrigated with saline. She had venous oozing, but no pulsatile bleeding. The wound was sprayed with thrombin and cautery was used for hemostasis. A KCI Wound-VAC was placed in the wound. The suction was set to 125 mmHg continuous. No significant output was appreciated in the operating room (OR).
Notably, when the patient was transferred to the Post Anesthesia Care Unit, her right leg was externally rotated >90° by OR staff who were unaware of her Girdlestone. No increase in Wound-VAC output occurred at that time.
February 04, 2024 11:30 am
The patient had approximately 150 mL of sanguinous fluid in her Wound-VAC canister. Suction was turned to 75 mmHg intermittent with better control of hemostasis appreciated over the next 15-min. Nurse instructions were to call the orthopedic team if the canister exceeded 300 mL by 5 pm.
February 04, 2024 4:30 pm
The patient had exuded 300 mL into the Wound-VAC canister. Her post-operative hemoglobin was 7.4. Considering her coagulation laboratories and low platelets, one unit of PRBCs and platelets were each transfused. It was hypothesized that the bleeding was due to her NASH, hyperinflammatory tissue, and pancytopenia. Returning to the OR would likely worsen the venous bleeding.
February 04, 2024 9:31 pm
The patient became hypotensive (81/43), and a rapid response was called. She appeared pale and had a total of 700 mL of blood in her Wound-VAC canister, with 400 mL over the last hour. Her post-transfusion hemoglobin decreased to 7.0. The critical care team was consulted, and she was transferred to the ICU. Two units of PRBCs, two units of fresh frozen plasma (FFP), and one unit of platelets were transfused. The orthopedic team was not contacted at this time. No advanced imaging was ordered.
February 05, 2024 7:35 am
The orthopedic team was contacted by the night nurse that the patient had 3000 mL of frank blood into her Wound-VAC overnight. She received a total of three units of PRBCs, two units FFP, one unit Platelets, two amps calcium gluconate, and 500 mL albumin. She remained hypotensive with a MAP of 59 but was stable, alert, and oriented. Her Wound-VAC was saturated and no longer functioning. A STAT-CT of her pelvis and right lower extremity was ordered. Thrombin spray was injected into her Wound-VAC and she was given 1 gram of tranexamic acid intravenously.
February 05, 2024 9:21 am
The patient had active extravasation from the SGA on CT scan. Interventional radiology (IR) was contacted, and emergent embolization was planned (Fig. 6).
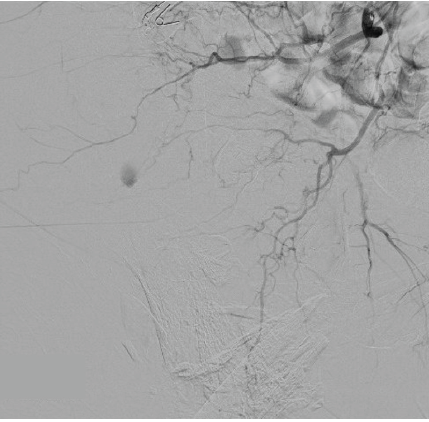
Figure 6: Anterograde hip angiogram via fluoroscopy depicting superior gluteal artery extravasation before emergent embolization.
February 05, 2024 10:30 am
The patient was taken to the IR suite and the arterial branch supplying the area of extravasation was embolized with Gelfoam to cessation. The right common iliac artery, internal iliac artery, posterior division, and seven additional high-order vessels including the superior gluteal artery region were embolized. Hemostasis was confirmed under fluoroscopy.
February 05, 2024 1:30 pm
The patient had her Wound-VAC replaced at bedside post-IR-embolization. The patient exuded <100 mL of serosanguinous drainage over 3 h and was hemodynamically stable.
February 06, 2024
The patient’s Wound-VAC contained <500 mL of serous output over 24 h; she was off pressors and was hemodynamically stable. The Wound-VAC was transitioned to an irrigating setup. ID recommended 6 weeks of meropenem based on the intraoperative culture Klebsiella sensitivities.
February 12, 2024
The patient was downgraded to the medicine floor. Her Wound-VAC was transitioned to non-irrigating therapy with 3 times weekly changes.
February 15, 2024 – present
The patient was discharged to a SNF with wound care. She continues to perform Wound-VAC changes and her wound is granulating. She is WBAT to her right lower extremity but has difficulty with mobility due to loss of strength and mild pain. She is working with PT for improvement.
Girdlestone resection arthroplasty has 90-day complication rates of 34% and an 11% mortality rate [5]. Vascular injury following total hip arthroplasty is <1%, but no data exists on vascular complications for Girdlestone arthroplasty [6]. The only case regarding post-Girdlestone vascular injury described a fatal pseudoaneurysm of the profunda femoris artery likely secondary to bony contact with the vessel and femur, although iatrogenic injury from retractor placement cannot be ruled out [3]. That case described a subtrochanteric osteotomy with more shortening than in our case where the patient had a traditional Girdlestone. The SGA sits approximately 5 cm from the tip of the greater trochanter, warranting caution in the anterolateral hip approach. As we did not experience any pulsatile or uncontrolled bleeding intra-operatively, it is unlikely that this structure was injured iatrogenically. Instead, the greater trochanter spiked remodeling, the large dead-space region following debridement, the decreased trochanter-SGA distance due to femoral shortening, and the excessive lower-extremity external rotation during transfer likely allowed for the greater trochanter spike to perforate the SGA.
Wound-VAC therapy has allowed progress in the field of complex wound management. This therapy is generally considered safe, but hemorrhage is a rare complication [7,8,9,10]. Physiologic or therapeutic anticoagulation, vascular trauma, and infected/inflammatory tissue all place patients at increased risk for bleeding [10]. Our patient had all three of these risk factors. Careful monitoring and clear instructions to the multidisciplinary care team regarding Wound-VAC output, transfusion parameters, and clinical presentation are essential. Had better communication occurred between the care-team members, this clinical scenario may have been caught earlier.
Vascular complications of Girdlestone resection arthroplasty, though rare, can be severe, as demonstrated by this report of SGA hemorrhage. Surgeons should be aware of these potentially life-threatening complications and must remain vigilant both intraoperatively, for the potentially sharp proximal femur, and postoperatively, for hemodynamic stability.
Superior gluteal artery extravasation following a Girdlestone procedure has not been previously reported in the literature. This case highlights the need for vigilance in post-operative monitoring for vascular complications to prevent poor outcomes. This report emphasizes the importance of recognizing and addressing vascular injuries, as well as prioritizing care team communications, to improve patient outcomes.
Although rare, vascular complications after Girdlestone resection arthroplasty can be severe. Surgeons should remain vigilant for sharp proximal femoral spikes intraoperatively and for post-operative hemodynamic instability.
References
- 1. Sharma H, Dreghorn CR, Gardner ER. Girdlestone resection arthroplasty of the hip: Current perspectives. Curr Orthop 2005;19:385-92. [Google Scholar] [PubMed]
- 2. Condell R, Low L, Kearns SR, Murphy CG. Girdlestone resection arthroplasty of the hip (GRA): A case series-outdated procedure or acceptable outcome? Eur J Orthop Surg Traumatol 2024;34:1711-5. [Google Scholar] [PubMed]
- 3. Pasquinelly A, Andrews K. Profunda femoris Pseudoaneurysm and fatal hemorrhage 2 weeks after modified girdlestone resection arthroplasty: A case report. JBJS Case Connect 2024;14:e23.00302. [Google Scholar] [PubMed]
- 4. Calligaro KD, Dougherty MJ, Ryan S, Booth RE. Acute arterial complications associated with total hip and knee arthroplasty. J Vasc Surg 2003;38:1170-7. [Google Scholar] [PubMed]
- 5. Malcolm TL, Gad BV, Elsharkawy KA, Higuera CA. Complication, survival, and reoperation rates following girdlestone resection arthroplasty. J Arthroplasty 2015;30:1183-6. [Google Scholar] [PubMed]
- 6. Barquet A, Gelink A, Giannoudis PV. Proximal femoral fractures and vascular injuries in adults: Incidence, aetiology and outcomes. Injury 2015;46:2297-313. [Google Scholar] [PubMed]
- 7. Orgill DP, Bayer LR. Update on negative-pressure wound therapy. Plast Reconstr Surg 2011;127 Suppl 1:105S-15. [Google Scholar] [PubMed]
- 8. Vikatmaa P, Juutilainen V, Kuukasjärvi P, Malmivaara A. Negative pressure wound therapy: A systematic review on effectiveness and safety. Eur J Vasc Endovasc Surg 2008;36:438-48. [Google Scholar] [PubMed]
- 9. Apelqvist J, Willy C, Fagerdahl AM, Fraccalvieri M, Malmsjö M, Piaggesi A, et al. EWMA document: Negative pressure wound therapy. J Wound Care 2017;26 Sup 3:S1-154. [Google Scholar] [PubMed]
- 10. Fleischmann W, Becker U, Bischoff M, Hoekstra H. Vacuum sealing: Indication, technique, and results. Eur J Orthop Surg Traumatol 1995;5:37-40. [Google Scholar] [PubMed]