Multiple puncture technique with intralesional corticosteroids is a novel method of treatment for plantar fasciitis.
Dr. Sanjul Bansal, Department of Orthopedics, Atal Bihari Vajpayee Government Medical College, Vidisha, Madhya Pradesh, India. E-mail: –bansal.sanjul4@gmail.com
Introduction: Plantar fasciitis is a common condition characterized by pain at the heel, particularly in the morning with the first step out of bed and initial steps after a long break. Corticosteroids were the mainstay of treatment for plantar fasciitis, but now other modalities are being tried. One such modality is the multiple puncture technique. The present study aims to compare the efficacy of the multiple puncture technique and corticosteroid in the treatment of plantar fasciitis.
Materials and Methods: A total of 38 patients were included in the study. Diagnosis of plantar fasciitis was made clinically based on history and presence of medial calcaneal tenderness. In the corticosteroid group, a 5 mL sterile syringe was taken and 2 mL of 2% lignocaine solution was loaded, while in the multiple puncture technique, 4–5 pricks were made in the plantar fascia close to the area of degeneration.
Results: Mean Visual Analog Scale score and mean American Orthopedic Foot and Ankle Society score improved in both groups at 1 week, 1 month, and 3 months follow-up. The improvement was found to be statistically significant in all three follow-ups (P < 0.01).
Conclusion: Multiple puncture technique is a safe and effective modality of treatment for plantar fasciitis.
Keywords: Plantar fasciitis, corticosteroid, multiple puncture.
Plantar fasciitis is among the most common chronic foot disorders seen in an orthopedic outpatient department. Pain at the heel, initiating as early as the first step out of bed in the morning (morning first pain), is a classical feature of this disease [1]. Very often seen in Indian homemakers, laborers, teachers, and surgeons, it has been associated with standing for long durations. As with many other disorders, the exact cause of plantar fasciitis is unknown. However, histological studies have shown marked thickening and fibrosis of the plantar fascia at its origin on the medial calcaneal tuberosity [2]. Collagen necrosis, angiofibroblastic hyperplasia, chondroid metaplasia, and matrix calcification have also been visualized, but no evidence of inflammation. Hence, it is now considered a degenerative disorder, and it is safe to say that plantar fasciitis should rather be called plantar fasciopathy or fasciosis [3]. Nearly 1% of the general population suffers from plantar fasciitis, of which females are about 2.5 times more likely to suffer from plantar fasciitis [3]. The main risk factors for plantar fasciitis include prolonged weight bearing (as in Indian homemakers, teachers, surgeons), uneven walking surface, footwear with less cushioning/barefoot walking, and obesity. The diagnosis is generally made on clinical grounds. A characteristic history of morning first pain, pain most severe during the first few steps after rest, and decreasing later on, and the examination finding of tenderness at the medial calcaneal tuberosity are sufficient in most cases. Management is usually multimodal, including activity restriction, non-steroidal anti-inflammatory drugs, physiotherapy (stretching exercises, extracorporeal shock wave therapy, ultrasonic massage), and night splints. If not relieved, the patient needs some form of treatment without surgery. This is where local injections come into play [4]. Intralesional corticosteroids have been used for a long time. They have been found to be effective but only for a short duration and with no healing effect on the degenerative condition. Furthermore, the risk of plantar fascia rupture and contraindications of steroid use warrant a need for another safe and effective method of treatment. Various modalities have been tried, such as prolotherapy and platelet-rich plasma (PRP) with variable success [5]. The multiple puncture technique offers a novel method of treatment for the same. In the multiple puncture technique, 4–5 pricks are made in the plantar fascia close to the area of degeneration, i.e., medial calcaneal tuberosity, with the help of an 18G needle. This creates a fenestration or pie-crusting pattern which helps stretch the fascia. Localized microbleeding also releases growth factors, which help in the healing of the affected tissue. This study aimed to compare the efficacy of the multiple puncture technique with intralesional corticosteroids and to establish it as a novel method of treatment for plantar fasciitis. Plantar fasciitis can be unilateral or bilateral. For the sake of the present study, only patients with bilateral plantar fasciitis were considered to help reduce bias due to patient factors. Differences in compliance with instructions regarding footwear and physiotherapy might change the results in some patients. Hence, only patients with bilateral disease were included in the study and received intralesional corticosteroids in one foot and the multiple puncture technique in the other foot. Sides for the two modalities were chosen randomly.
This single-center study was conducted at MGM Medical College in 38 patients who were suffering from plantar fasciitis, which limits the statistical power and generalizability of the findings. Plantar fasciitis can be unilateral or bilateral. For the sake of the present study, only patients with bilateral plantar fasciitis were included in the study. Before the study, ethical permission was obtained from the Institutional Ethics Committee (IEC) Committee MGM Medical College, Indore (IEC/2020/23/date August 09, 2020).
Inclusion criteria
All patients aged 20–70 years of either sex having
- Bilateral Plantar fasciitis with the windlass test positive
- Ability to walk
- Subject understands the risks and benefits of the protocol and can give informed consent
- Availability for the duration of the entire study.
Exclusion criteria
- Previously operated for plantar fasciitis
- Deformation of the foot (congenital/acquired)
- Allergy to local anesthesia
- Pregnancy
- Fractures of the foot
- Osteomyelitis involving the calcaneum
- Patients with immunosuppression
- History of any other disease capable of inducing pain or sensitivity to foot such as diabetes mellitus, hypo- or hyperthyroidism, fibromyalgia, Vitamin B12 deficiency, Vitamin D deficiency, and seronegative arthritis. All such patients were advised physician check-up and treatment for the same.
Diagnosis was made clinically on the basis of history and presence of medial calcaneal tenderness. X-rays of the bilateral heel in lateral view were done to detect a calcaneal spur. Only pain (Visual Analog Scale [VAS]), function (the American Orthopedic Foot and Ankle Society [AOFAS]), and plantar fascia thickness were assessed; other parameters, such as quality of life or return to activity, were not included. Intralesional corticosteroid was injected in one of the feet, and the other received multiple puncture. In the corticosteroid group, a 5 mL sterile syringe was taken, and 2 mL of 2% lignocaine solution was loaded. In the same syringe, 2 mL of 40 mg/mL injection triamcinolone was loaded to make a total preparation of 4 mL. With the patient lying in the lateral decubitus position, the medial calcaneal tuberosity was palpated, and a 23G needle was inserted just distal to the tuberosity into the plantar fascia. As a gritty sensation was felt when entering the plantar fascia, the needle was withdrawn 1–2 mm and the solution was injected at this site. Any bleeding was stopped with sterile gauze, and the injection site was covered with a sterile dressing. In the multiple puncture group, only 2 mL of 2% lignocaine solution was loaded in a 5 mL syringe and injected at the insertion of the plantar fascia as described in the corticosteroids group. However, in this case, an 18G needle was used to inject the solution, and after injection, 4–5 pricks were made ~ 3–5 mm apart in the plantar fascia using the same needle without pulling it out of the skin. The post-injection protocol included restricted weight bearing for 24 h and analgesics (paracetamol and ibuprofen) for 3 days. Physiotherapy and footwear advice were given, but compliance and exact implementation were not strictly monitored, which may affect outcomes. The maximum follow-up was 3 months; long-term efficacy and recurrence rates were not assessed. Patients were assessed using the AOFAS score and VAS score pre-injection, at 1 week, 1 month, and 3-month follow-ups. Assessment of plantar fascia thickness was done pre-injection and at 1 month. Long-term complications such as fascia rupture or fat pad atrophy were not evaluated.
Plantar fasciitis, which is better called “plantar fasciopathy” is a degenerative disease of the insertion of plantar fascia at the medial calcaneal tuberosity. Since it was earlier considered an inflammatory disease, the most commonly used local injection was corticosteroids. However, now histopathological and electron microscopic studies have shown that it is actually a degenerative disease. This has led to a change in the understanding of the disease process and its management. Studies have shown that prolotherapy and PRP are also effective in managing plantar fasciitis. Other methods being tried include dry needling and botulinum toxin. The study compared only corticosteroids and the multiple puncture technique, whereas other emerging regenerative therapies (PRP, prolotherapy, dry needling) were not included for a more comprehensive comparison. Multiple puncture technique is a new method of local injection in which 4–5 fenestrations are made 3–5 mm apart in the plantar fascia using an 18G needle. These fenestrations allow the fascia to stretch like a pie-crusting pattern and allow the plantar fascia to get stretched during activities such as walking. Hence, there is a decrease in the pain perceived while doing these activities. This also leads to localized micro-bleeding with release of various growth factors such as transforming growth factor-beta and platelet-derived growth factor locally. These growth factors further help in the healing of the degenerated plantar fascia. Kukreja et al. in their study of corticosteroids and PRP injection found both modalities to be effective at 3 months of follow-up, with the effect of corticosteroids weaning off rapidly after 3 months. However, they found that PRP was effective even after 3 months, all the way up to 12 months [6]. Whittaker And Say et al. in their study of corticosteroids and PRP followed up 50 patients at 6 weeks and 6 months [7,8]. They also found PRP to be more effective than corticosteroids in chronic plantar fasciitis.
Say F et al. in their study of 388 patients, have found that in terms of improvement in pain, dextrose prolotherapy is superior to placebo but inferior to corticosteroids in the short term. In the long-term, however, prolotherapy was found to be even better than corticosteroids in reducing pain and improving function [8]. Lai WF et al. in their study of 66 patients, found both corticosteroids and dry needling to be effective in reducing pain at the plantar fascia in the short term [9]. However, in the long-term, dry needling was found to be more effective than corticosteroids. Many more such studies have shown that regenerative modalities are at least equally effective as corticosteroids, if not more, in the treatment of plantar fasciitis [10]. Particularly in the long-term, these modalities have been found to be more effective in comparison with corticosteroids. Hence, more research is required into these modalities. In our study, we found multiple puncture techniques to be as effective as corticosteroids at 3 months of follow-up. The decrease in mean VAS scores and the improvement in mean AOFAS scores were significant in both the groups. The decrease in plantar fascia thickness was also significant. Our study shows that the multiple puncture technique can be used in the treatment of plantar fasciitis with very good outcomes. It is a new modality of treatment and warrants further studies to establish its efficacy in the long-term.
A total of 38 patients were included in the study, of which 10 (26.32%) were male and 28 (73.68%) were female. The mean age was 35.7 years with a standard deviation of 5.66.6 (15.78%) patients were up to the age between 41 and 50 years. 32 patients (84.21%) had bony spur on X-rays. Mean body mass index was 23.2 with a standard deviation of 2.07. Mean VAS score and AOFAS score at all three follow-ups were analyzed and to assess the differences in the mean of the two groups. A Student’s t-test was performed. Plantar fascia thickness measured pre-injection and at 1-month follow-up was also analyzed. Mean VAS score and mean AOFAS score improved in both the groups at 1 week, 1 month, and 3 months’ follow-up. The improvement was found to be statistically significant in all three follow-ups (P < 0.001). Plantar fascia thickness also decreased in both the groups, and the decrease was statistically significant (P < 0.001) (Table 1).
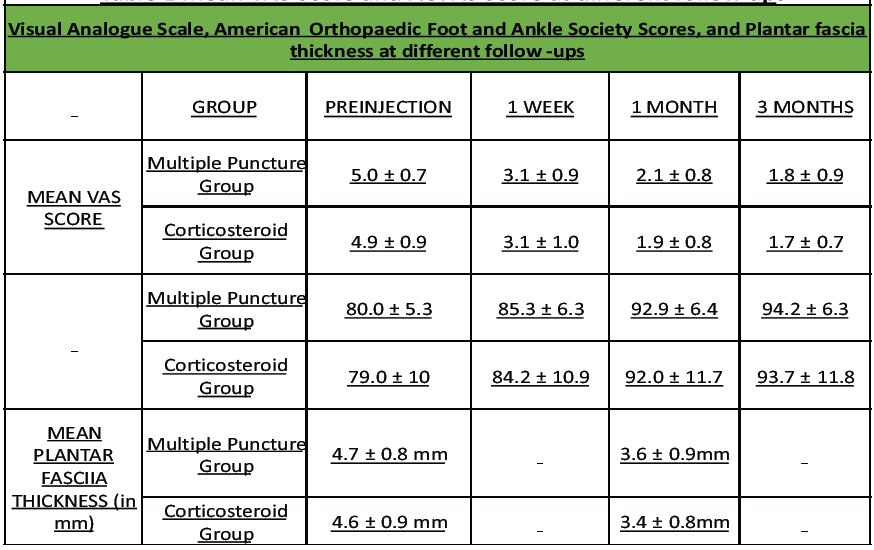
Table 1: Mean VAS Score and AOFAS Score at different follow ups
However, comparison between the groups revealed mean difference in VAS score to be 0.1 preinjection, 0 at 1 week and 0.2 at 1 month, and 0.1 at 3 months. The mean difference in AOFAS score was 1.0 preinjection, 1.1 at 1 week follow-up, 0.9 at 1 month follow up and 0.5 at 3 months’ follow-up. The mean difference in plantar fascia thickness was 0.1 preinjection and 0.2 at 1-month follow-up. All of these were found to be statistically insignificant (P > 0.05). The statistical analysis shows that the multiple puncture technique is not less effective compared to corticosteroids in decreasing pain and improving function in plantar fasciitis. No severe adverse effects were seen in any group. The most common complaint in post-injection period was increased pain for 2–3 days, which was relieved with analgesics.
Multiple puncture technique is a safe and effective modality of treatment for plantar fasciitis. However, there is a need for larger studies with long-term follow-ups to verify its efficacy and advantages over corticosteroids.
The multiple puncture technique is equally effective as corticosteroid injections. It offers a non-steroidal alternative for managing plantar fasciitis. It may be preferable for patients seeking minimally invasive, drug-free options.
References
- 1. Lemont H, Ammirati KM, Usen N. Plantar fasciitis: A degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc 2003;93:234-7. [Google Scholar] [PubMed]
- 2. Menon NA, Jain J. Plantar fasciitis: A review. Indian J Pain 2018;32:24-9. [Google Scholar] [PubMed]
- 3. Nahin RL. Prevalence and pharmaceutical treatment of plantar fasciitis in United States adults. J Pain 2018;19:885-96. [Google Scholar] [PubMed]
- 4. Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med 2004;350:2159-66. [Google Scholar] [PubMed]
- 5. Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician 2011;84:676-82. [Google Scholar] [PubMed]
- 6. Kukreja T, Agarwal T, Singh A, Bhugra H. Comparative study for the treatment of plantar fasciitis by corticosteroids versus platelet rich plasma. Med J D Y Patil Univ 2017;10:252-6. [Google Scholar] [PubMed]
- 7. Whittaker GA, Munteanu SE, Menz HB, Bonanno DR, Gerrard JM, Landorf KB. Corticosteroid injection for plantar heel pain: A systematic review and meta-analysis. BMC Musculoskelet Disord 2019;20:378. [Google Scholar] [PubMed]
- 8. Say F, Gürler D, İnkaya E, Bülbül M. Comparison of platelet-rich plasma and steroid injection in the treatment of plantar fasciitis. Acta Orthop Traumatol Turc 2014;48:667-72. [Google Scholar] [PubMed]
- 9. Lai WF, Yoon CH, Chiang MT, Hong YH, Chen HC, Song W, et al. The effectiveness of dextrose prolotherapy in plantar fasciitis: A systemic review and meta-analysis. Medicine (Baltimore) 2021;100:e28216. [Google Scholar] [PubMed]
- 10. Kim E, Lee JH. Autologous platelet-rich plasma versus dextrose prolotherapy for the treatment of chronic recalcitrant plantar fasciitis. PM R 2014;6:152-8. [Google Scholar] [PubMed]