For late TKA rotational instability from PLC insufficiency, a hybrid technique of anatomic reconstruction and insert upsizing can restore stability while preserving well-fixed components.
Dr. Vaibhav Bagaria, Department of Orthopaedics, Sir H N Reliance Foundation Hospital and Research Centre, Mumbai, Maharashtra, India. E-mail: bagariavaibhav@gmail.com
Introduction: Post-operative instability is a challenging complication following total knee arthroplasty (TKA), with most literature addressing coronal or sagittal laxity. Rotational instability, particularly involving the posterolateral corner (PLC), is rare and frequently overlooked. Conventional revision strategies often involve increasing constraint or complete component revision, which may not be appropriate in cases with well-aligned and well-fixed implants.
Case Report: A 60-year-old female presented 1-year post-primary TKA with symptomatic instability, manifesting as difficulty stair climbing and diminished confidence in the operated limb. Clinical evaluation revealed varus thrust, a positive dial test at 30°, and posterolateral laxity. Radiographic and computed tomography assessment confirmed well-positioned, stable components with no evidence of infection. Intraoperative findings demonstrated significant rotational instability of the rotating platform polyethylene insert without mechanical failure. A hybrid surgical solution was utilized: retention of the well-fixed components, upsizing of the polyethylene insert, and anatomic PLC reconstruction using a semitendinosus autograft. Postoperatively, the patient achieved marked improvement in functional stability and mobility, resuming independent activities. At 8-month follow-up, validated outcome scores demonstrated substantial enhancement, with no recurrent instability or complications.
Conclusion: This case report illustrates a novel hybrid stabilization technique for late PLC-derived rotational instability after TKA. Combining polyethylene insert upsizing with anatomic PLC reconstruction effectively restored knee stability while preserving well-fixed components, presenting a viable joint-preserving alternative to conventional revision arthroplasty in selected patients.
Keywords: Total knee arthroplasty, posterolateral corner, rotational instability, ligament reconstruction, rotating platform, hybrid revision, polyethylene insert upsizing.
Instability is a recognized complication following total knee arthroplasty (TKA) and accounts for a significant proportion of early revisions. While most reported cases involve coronal or sagittal plane instability, rotatory instability, particularly due to posterolateral corner (PLC) insufficiency, remains under-recognized and underreported [1,2]. Posterolateral rotatory instability (PLRI) after TKA may manifest as a subjective sense of “giving way,” difficulty navigating stairs, or progressive loss of confidence in the operated limb. It is typically diagnosed through clinical findings such as a positive dial test at 30, varus thrust gait, and varus laxity on stress testing, in the context of otherwise well-fixed and aligned implants [1,3]. Standard imaging helps exclude mechanical causes such as malalignment or component loosening, while infection workup must also be negative before a soft-tissue diagnosis can be confirmed [3]. The PLC comprises a complex network of stabilizers including the lateral collateral ligament (LCL), popliteus tendon, and popliteofibular ligament, which together resist varus and external rotational forces [2,4]. Injury or attenuation of these structures can result in functional instability, even in the presence of appropriate prosthetic alignment [5,6]. Conventional management options for such cases often involve upsizing the polyethylene insert or converting to a more constrained implant. However, these approaches may be insufficient or may introduce additional challenges, including increased stress at the bone–implant interface and risk of aseptic loosening [3,7]. Moreover, complete revision may not be justifiable when the components are well-fixed and well-aligned. In this report, we describe a novel hybrid approach to managing late post-TKA instability attributed to PLC insufficiency. Our technique combines polyethylene insert upsizing with anatomic PLC reconstruction using a semitendinosus autograft, while retaining the original femoral and tibial components. To the best of our knowledge, this is one of the first documented cases where a soft-tissue reconstruction was used to restore posterolateral stability in a TKA patient, avoiding full revision and yielding excellent clinical outcomes [1,8].
A 60-year-old female presented 1 year following primary TKA (performed elsewhere) with persistent symptomatic instability and functional impairment. Chief complaints included a subjective sensation of “giving way,” difficulty with ambulating long distances, and an inability to climb stairs, which had progressively diminished confidence in the operated limb. These symptoms persisted despite extensive rehabilitation (Fig. 1).
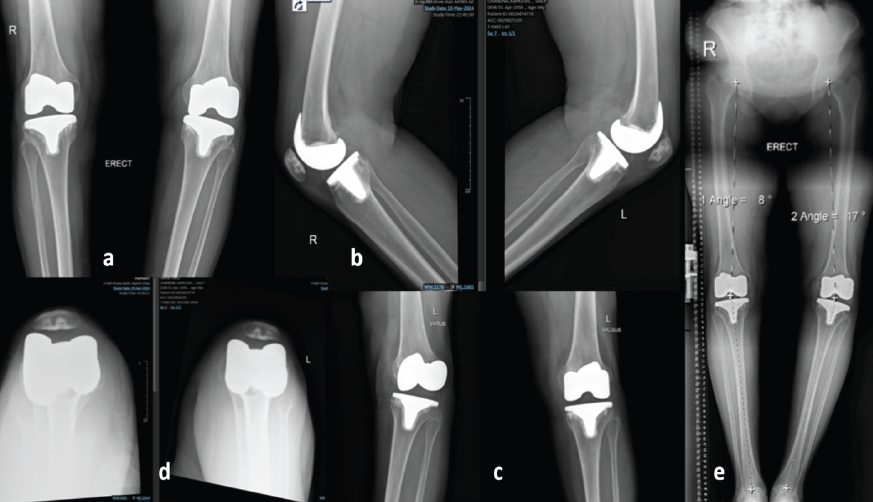
Figure 1: Pre-operative imaging demonstrating features suggestive of posterolateral corner insufficiency following total knee arthroplasty. (a) Anteroposterior radiograph of the knee showing well-fixed femoral and tibial components with preserved medial and lateral joint spaces. (b) Lateral radiograph demonstrating maintained sagittal alignment without evidence of component loosening or subsidence. (c) Varus stress radiograph showing preserved medial compartment stability, valgus stress radiograph demonstrating subtle lateral compartment opening, suggestive of lateral soft-tissue laxity. (d) Skyline view showing patella tracking. (e) Full-length standing scanogram illustrating overall lower limb alignment with residual varus alignment.
On clinical examination, she exhibited a pronounced varus thrust during gait analysis and showed positive dial test at 30° of knee flexion, suggestive of PLRI. Varus laxity was evident on stress testing, and no hyperextension or anteroposterior instability was observed. The rest of her neurovascular examination was unremarkable. Standing long-leg alignment radiographs confirmed well-fixed femoral and tibial components without evidence of loosening. Computed tomography revealed that the angle between posterior condyle line and surgical transepicondylar axis was 4° and thus excluded component rotational malalignment. On X-ray and scanogram analysis, there was a varus of 17° on the affected left side and posterior slope was 3°. Laboratory investigations (C-reactive protein and erythrocyte sedimentation rate) and joint aspiration ruled out infection. Based on the clinical and radiographic findings, a diagnosis of late posterolateral instability secondary to PLC insufficiency was established. Given the well-fixed, well-aligned components, and the absence of infection, a joint-preserving hybrid surgical strategy was planned. The aim was to restore functional stability without revising the components. Under spinal anesthesia, the joint was exposed through a standard medial parapatellar approach. Intraoperative assessment revealed well-fixed and properly positioned components. However, the rotating platform (RP) tibial insert exhibited significant rotational instability, particularly pronounced during application of varus stress and external rotation in mid-flexion. The tibial cut was noted to be in slight varus alignment, a finding suggestive of possibly intraoperative compensation for medial tightness during the index arthroplasty (Fig. 2). Furthermore, the lateral soft-tissue structures, specifically the PLC, demonstrated attenuation with associated functional incompetence, directly contributing to the observed persistent rotatory laxity (Fig. 3 and 4).
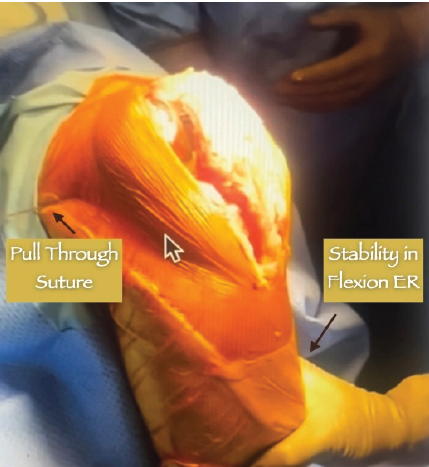
Figure 2: Intraoperative picture showing the appropriate tensioning and stability following the reconstruction.
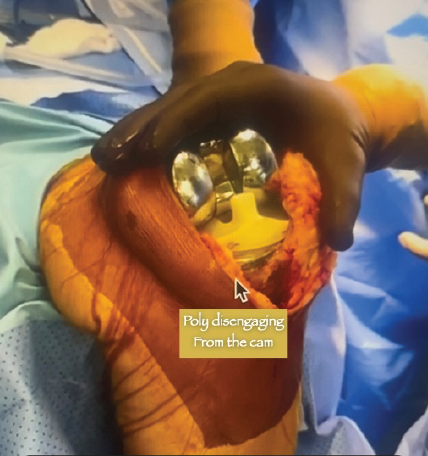
Figure 3: Intraoperative imaging shows poly spinning out after performing dial test.
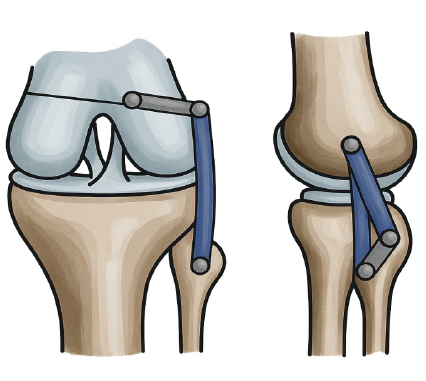
Figure 4: Illustration showing the technique of posterolateral corner reconstruction.
A two-pronged hybrid surgical approach was implemented:
- Polyethylene insert upsizing: The existing insert was removed and replaced with a larger one (by 2 mm) to improve coronal plane tension and minimize laxity in extension and mid-flexion. Trial insert evaluation showed improved mediolateral balance.
- Anatomic PLC reconstruction: A semitendinosus autograft was harvested through the same incision. Using an anatomical double-bundle reconstruction technique adapted from multi-ligament knee reconstruction principles, tunnels were drilled into the fibular head (to recreate the popliteofibular ligament) and into the lateral femoral condyle (for LCL and popliteus insertion). The graft was passed and tensioned with the knee in 30° of flexion and neutral rotation, then secured with interference screws and cortical fixation buttons as required.
Post-graft fixation, intraoperative assessment confirmed restoration of posterolateral stability, with negative dial test and symmetric varus stress response. Patellar tracking remained central with no signs of maltracking or instability. The joint was closed in layers, and a hinged knee brace was applied. Postoperatively, the patient was managed with a hinged knee brace locked in extension for the initial 2 weeks. Early range of motion exercises was initiated from day 3, progressing cautiously under supervision to protect the reconstructed PLC. Weight-bearing was restricted to toe-touch ambulation for the first 4 weeks, followed by a gradual increase to full weight-bearing by week 8, aligned with improvement in quadriceps control and proprioceptive feedback. The physiotherapy protocol emphasized neuromuscular retraining, proprioceptive drills, and lateral chain strengthening, targeting the gluteal and biceps femoris musculature to restore posterolateral dynamic stability. Isometric quadriceps and hamstring co-contraction drills were introduced early, with closed-chain exercises phased in after 6 weeks (Fig. 2 and 5).
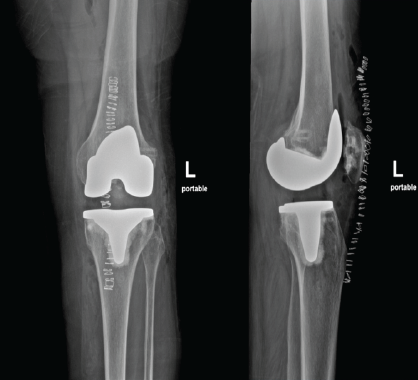
Figure 5: Immediate post-operative X-ray showing preserved joint and a well-balanced flexion extension gap.
By the 3-month post-operative visit, the patient reported markedly improved subjective knee confidence and achieved unassisted ambulation. At the 6-month mark, she had successfully resumed stair climbing and independent performance of daily activities without difficulty. Validated functional outcome scores demonstrated substantial improvement: the Knee Injury and Osteoarthritis Outcome Score increased from 42 preoperatively to 82, and the Western Ontario and McMaster Universities Osteoarthritis Index decreased significantly from 48 to 18. The dial test remained negative at all assessments. At the latest follow-up of 8 months, the patient had returned to a physically active lifestyle without functional limitations. Radiographic evaluation confirmed maintained implant position and alignment. Clinically, there was no evidence of instability, graft failure, or excessive polyethylene wear. Dynamic assessment confirmed central alignment of the RP insert without rotational subluxation (Fig. 6).
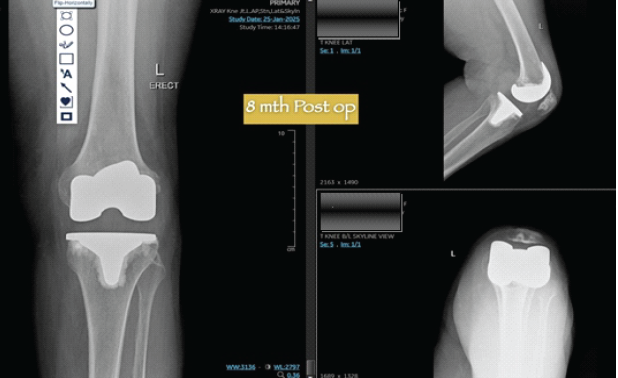
Figure 6: Eight-month follow-up X-rays showing no secondary laxity or alteration in the alignment.
Soft-tissue balancing is essential not only for achieving mechanical alignment but also for ensuring the functional success and longevity of a total knee replacement. Instability remains one of the leading causes of early revision following TKA, with posterior and coronal plane laxity being most frequently addressed in the literature. Rotational instability, particularly PLRI), is less frequently reported and often underdiagnosed [1,2,3]. In this case, the patient presented with clinical features suggestive of PLRI despite radiographically well-fixed components. Advances in digital and robotic-assisted surgery, along with real-time intraoperative assessment tools, have made soft-tissue balancing more accurate and reproducible further improving surgical outcomes. A key intraoperative finding was rotatory instability of the RP insert, exacerbated by varus stress and external tibial rotation. The platform demonstrated excessive spin in mid-flexion, in the absence of infection or mechanical loosening. This suggested functional posterolateral insufficiency as the principal driver of instability [2,6,4]. RP designs are sensitive to soft-tissue balance. While they offer improved kinematics and wear characteristics, they require symmetric ligamentous support to prevent rotational drift. Inadequate balancing particularly on the lateral side can lead to bearing instability or subluxation. In this case, it is likely that the tibial cut was made in residual varus during the index procedure to accommodate medial tightness, leaving the lateral structures under-tensioned. Over time, progressive stretching and attenuation of the PLC may have resulted in clinical instability [5,3,7]. Traditional management strategies for such presentations often involve full component revision with increased constraint (e.g., constrained condylar knee or rotating hinge designs). While effective, these carry associated risks of higher mechanical stress at fixation interfaces, reduced implant longevity, and increased complication rates. Component revision may also be biologically and economically unjustifiable when the prosthesis is well-fixed and appropriately aligned [2,3]. In contrast, the present case demonstrates a hybrid approach involving polyethylene insert upsizing and anatomic PLC reconstruction, with partial retention of existing components. This strategy directly addresses soft-tissue deficiency while preserving implant integrity. Although intuitive, such approaches remain underutilized possibly due to limited familiarity among arthroplasty surgeons with soft-tissue reconstructive techniques, and a lack of published outcomes in this setting [1,2,4]. The outcome in this case was favorable, with restoration of rotatory stability, resolution of subjective symptoms, and return to function. However, this technique is not universally applicable. It requires stable and well-aligned components, appropriate patient selection, and surgical expertise in ligament reconstruction [1,9,10]. Long-term graft performance in the prosthetic knee environment remains a consideration, and further study is warranted.
Late PLRI following TKA presents a complex surgical challenge. This case report illustrates a novel, joint-preserving hybrid approach for managing this condition in the presence of well-fixed and well-aligned components. By combining polyethylene insert upsizing with anatomic PLC reconstruction, we successfully restored rotational stability, resolved subjective instability, and enabled a return to function without revising the original implants. This technique represents a viable and less invasive alternative to conventional component revision in carefully selected patients, though long-term outcomes and broader application require further study.
In cases of late total knee arthroplasty (TKA) instability due to isolated posterolateral corner (PLC) insufficiency with well-fixed components, a joint-preserving hybrid surgical approach should be considered. This involves anatomic PLC reconstruction combined with polyethylene insert upsizing, rather than automatic full component revision. It effectively restores rotational stability while preserving bone stock and the original implant. This approach is a valuable, less invasive alternative for carefully selected patients, expanding surgical options beyond constrained revision.
References
- 1. Sharma S, Kulkarni S, Rankin E, et al. Posterolateral corner reconstruction alone using a fibular-based technique for unstable total knee arthroplasty. J Orthop Case Rep 2015;2015:262187. [Google Scholar] [PubMed]
- 2. Villarreal-Espinosa JB, Haynes M, Cotter EJ, Saad Berreta R, Cancienne JM, Verma NN, et al. Posterolateral corner ligament reconstruction in knee arthroscopy: Complications and complication management. J Clin Orthop Trauma 2025;64:102948. [Google Scholar] [PubMed]
- 3. Haider O, Scheidl T, Sterneder CM, Boettner F. Lateral instability 13 years after kinematically aligned total knee arthroplasty. Arthroplast Today 2025;33:101674. [Google Scholar] [PubMed]
- 4. Khanduja V, Somayaji HS, Harnett P, Utukuri M, Dowd GS. Combined reconstruction of chronic posterior cruciate ligament and posterolateral corner deficiency. A two- to nine-year follow-up study. J Bone Joint Surg Br 2006;88:1169-72. [Google Scholar] [PubMed]
- 5. Lamba A, Boos AM, Krych AJ, Stuart MJ, Hevesi M, Levy BA. Satisfactory outcomes and improved range of motion with arthroscopic lysis of adhesions and manipulation for arthrofibrosis after multiligamentous knee reconstruction. Arthrosc Sports Med Rehabil 2023;5:100784. [Google Scholar] [PubMed]
- 6. Chechik O, Mayer C, Drexler M, Sternheim A, Snir N, Dekel S. Posterolateral capsular release for correction of valgus deformity. J Knee Surg 2012;25:355-60. [Google Scholar] [PubMed]
- 7. Golovakha ML, Bondarenko SB, Orljanskі W. Results of minimally invasive knee posterolateral corner reconstruction. Orthop Traumatol Prosthet 2021;4:13-21. [Google Scholar] [PubMed]
- 8. Rosario PM, Ra RE. A case report on the management of peri-prosthetic fracture in a post-tka patient with rheumatoid arthritis: Surgical strategy and treatment outcome arthritis. J Orthop Case Rep 2025;15:180-4. [Google Scholar] [PubMed]
- 9. Oner K, Kose O. Is peroneus longus tendon the ideal graft for ACL reconstruction? Sports Traumatol Arthrosc 2025;2:1-3. [Google Scholar] [PubMed]
- 10. Fraval A, Karim MA, Bagaria V, Lyu S, Manzary M, Chen CF, et al. What factors determine the necessity of tibial and/or femoral stem use in primary total knee arthroplasty? J Arthroplasty 2025;40:S79-81. [Google Scholar] [PubMed]








