There is a significant association between Vitamin D levels and lateral epicondylitis of the elbow; hence, Vitamin D deficiency should be looked for and treated in all cases of lateral epicondylitis of the elbow.
Dr. Udit Kumar Biswal, Department of Orthopaedics, Institute of Medical Sciences and Sum Hospital, Bhubaneswar, Odisha, India. E-mail: uditkumarbiswal@gmail.com
Introduction: Lateral epicondylitis (LE) or tennis elbow is a degenerative condition that causes pain and tenderness at the lateral aspect of the elbow, usually secondary to repetitive strain of wrist extensors. Although there is a well-defined association between musculoskeletal disorders and environmental, genetic, and lifestyle risk factors, the etiological role of Vitamin D in musculoskeletal diseases is still an area of active research. The objective of this study was to evaluate the correlation between serum Vitamin D levels and the incidence of LE among a population in Eastern India.
Materials and Methods: A total of 150 subjects, 75 with diagnosed LE and 75 age- and sex-matched controls, were studied cross-sectionally. Serum Vitamin D concentrations were determined and calculated for the possible association with LE prevalence and severity.
Results: A total of 75 cases and 75 controls were analyzed. Both groups were comparable in age and gender. Mean serum Vitamin D levels were significantly lower in cases than controls (15.3 ± 7.2 vs. 28.5 ± 10.1 ng/mL, P < 0.001), with Vitamin D deficiency more common among cases (70% vs. 22%). Serum Vitamin D level was strongly negatively correlated with LE (Pearson’s r = −0.62, P < 0.001). Vitamin D deficiency increased the odds for LE by over threefold (odds ratio 3.2; 95% confidence interval: 1.8–5.6). This association remained significant across subgroups, with the highest prevalence observed in those performing repetitive upper-limb activities.
Conclusion: The study showed a strong negative correlation between the low serum Vitamin D status and the occurrence of LE, implicating a possible role for Vitamin D in the pathogenesis of this disease. This emphasizes the clinical significance of Vitamin D status monitoring in at-risk subjects for LE development and its role in both preventive and therapeutic treatment.
Keywords: Lateral epicondylitis, Vitamin D, serum Vitamin D levels, elbow pain, musculoskeletal disorders, tennis elbow.
Lateral epicondylitis (LE) or tennis elbow is a syndrome of overuse of the forearm extensor muscles, characterized by lateral epicondylar pain and tenderness, resulting from repetitive stress and overuse of the muscles of the extensor–supinator compartment of the forearm, most commonly involving the extensor carpi radialis brevis [1]. Although initially thought to be an inflammatory process, more recent research has emphasized its degenerative etiology, and tendinopathy is actually the true pathology [3]. This condition is found among athletes, especially tennis players, with repetitive stroke actions, and also individuals with occupations that require repetitive extension movements of the forearm and wrist, such as carpenters, painters, software professionals, writers, and even housewives. The occurrence of LE is most prevalent in adults between the ages of 30 and 50 years and is equally present in both males and females [3]. From a pathophysiological point of view, LE is a tendinopathy in which degeneration of collagen, neovascularization, and inflammatory cell invasion of the affected tendons occur [1,4]. The treatment ranges from conservative measures such as rest, icing, use of braces and analgesics to local corticosteroid injections and even surgery in resistant cases [5]. Recent studies have focused interest on various biochemical and metabolic pathways leading to the development of LE, and one such molecule of interest is Vitamin D. Vitamin D is a fat-soluble vitamin that plays a vital role in calcium regulation, bone metabolism, and the regulation of the immune system [6]. Apart from its classical role in bone metabolism, a lot of evidence suggests that Vitamin D has a direct role in soft-tissue health, including the functioning and repair of tendons [7]. The deficiency of Vitamin D is implicated in numerous musculoskeletal disorders such as osteoporosis, osteomalacia, and muscle weakness and fatigue [8]. However, the etio-pathogenesis of LE is still poorly understood, particularly in non-Western communities such as India’s, where Vitamin D deficiency is quite common due to minimal exposure to sunlight, poor nutrition, and pigmentation. The present study aims to investigate the association between serum Vitamin D level and incidence of LE in a population of Eastern India and to provide evidence on whether Vitamin D deficiency can be a causative agent of LE. This can help in the formulation of future diagnostic and therapeutic guidelines for this condition.
Study design
This was a cross-sectional observational study which was conducted at a medical college and its multi-speciality hospital in Eastern India over a period of 1 year (January 2023–December 2023 The study was approved by the Institutional Ethics Committee vide approval number IEC/IMS.SH/SOA/2023/032 dated January 12, 2023. All participants were explained in detail about the study and provided written informed consent before their participation.
Sample size calculation
The sample size calculation was done using a two-proportion comparison formula. Based on an anticipated difference in Vitamin D deficiency prevalence between cases and controls drawn from previous literature, an expected effect size corresponding to an odds ratio (OR) of about 2.0, with a confidence level of 95% and a power of 80%, the minimum sample required was estimated to be 150 participants, with 75 subjects in each group. This sample size was determined to be sufficient to obtain a clinically important association between serum Vitamin D levels and LE, also allowing subgroup analyses.
Study population
A total of 150 participants were enrolled in the study and were divided into two groups:
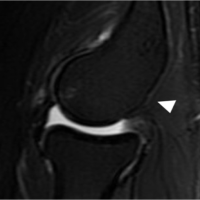
- Group 1 (Cases): 75 patients with clinically diagnosed LE (lateral epicondyle tenderness, pain on resisted wrist extension (Cozen’s test positive), and/or pain on resisted grip). The diagnosis in all patients had been confirmed with ultrasound evaluation, with the usual findings being tendon thickening, hypoechogenicity, partial thickness tears, neovascularity, or peritendinous inflammatory changes.
- Group 2 (Controls): 75 age, sex and body mass index (BMI)-matched individuals who presented to outpatient departments of other clinical specialties with no musculoskeletal problems or history of elbow pain.
Individuals between the ages of 18 and 60 years with clinically and radiologically (by ultrasound findings as enlisted previously) diagnosed LE were included by a consecutive non-probability purposive sampling of patients attending the orthopedic department. Those with a history of systemic diseases (e.g., diabetes and rheumatoid arthritis), recent trauma to the elbow, or those on Vitamin D replacement therapy or medications that interfere with calcium metabolism were excluded from the study.
Data collection
Demographic and clinical details of the subjects, such as age, gender, occupation, duration of symptoms, and history of any comorbidity, were collected. Serum Vitamin D was measured in both groups using electrochemiluminescence immunoassay with the following standard cutoff values: Serum Vitamin D value <20 ng/mL as deficiency, 20–30 ng/mL as insufficiency, and >30 ng/mL as sufficient.
Statistical analysis
For statistical analysis, we used the Statistical Package for the Social Sciences software (version 25.0) and Chat GPT AI model. The continuous variables have been reported as mean ± standard deviation, and categorical variables reported as frequencies with percentages. The correlation between the degree of serum Vitamin D and the incidence of LE was assessed with Pearson’s correlation coefficient. An independent t-test was utilized to compare Vitamin D levels among the cases and controls, and to determine the association between categorical variables, we used Chi-square tests. Statistical significance was established with a P < 0.05.
Demographic characteristics
Seventy-five cases and 75 controls were enrolled in the study. The mean age was 42.3 ± 7.5 years in the case group and 43.1 ± 8.3 years in the control group (P = 0.652). The gender ratio was 1:1 in both groups. Professions of case group participants included manual workers (homemakers, carpenters, painters) and office staff, with a high proportion of repetitive use of forearms and wrists. In the control group, participants were typically sedentary professionals or those with little repetitive upper limb activity.
Serum Vitamin D levels
Mean serum Vitamin D concentration in the case group was 15.3 ± 7.2 ng/mL, and in the control group, 28.5 ± 10.1 ng/mL (P < 0.001). A high percentage (70%) of subjects in the case group were deficient in Vitamin D (<20 ng/mL), whereas in the control group, it was just 22%. Insufficiency (20–30 ng/mL) was observed in 20% of the case group and 32% of the control group, and 10% of the case group and 46% of the control group had adequate Vitamin D levels (>30 ng/mL) (Fig. 1 and Table 1).

Figure 1: Serum Vitamin D levels in cases versus controls – box plot.

Table 1: Vitamin D levels across groups
Association between Vitamin D level and incidence of LE
There was a high negative correlation between serum Vitamin D level and incidence of LE (Pearson’s r = −0.62, P < 0.001), i.e., lower Vitamin D levels were more likely to develop LE. OR for Vitamin D deficiency as a risk factor for LE was 3.2 (95% confidence interval: 1.8–5.6), showing that patients with Vitamin D deficiency were more than 3 times more likely to have LE compared to their counterparts with sufficient levels of Vitamin D (Fig. 2 and Table 2).

Figure 2: Correlation between serum Vitamin D levels and LE – scatter plot.

Table 2: Correlation of LE and Vitamin D deficiency
Subgroup analysis
When stratified by age, gender, and occupation, the correlation between LE and low-serum Vitamin D remained significant in all groups. Interestingly, employees with occupational repetitive arm use (painters and carpenters) had a greater prevalence of both Vitamin D deficiency and LE than those employed in sedentary occupations (P = 0.02) (Fig. 3).

Figure 3: Occupational risk and Vitamin D deficiency in lateral epicondylitis – bar graph.
In this cross-sectional study, we found a strong inverse association between serum 25-hydroxyvitamin D levels and LE: Cases had significantly lower mean Vitamin D and a markedly higher prevalence of deficiency than matched controls, and Vitamin D deficiency was associated with a >3-fold increased odds of LE. These results directly satisfy the study objective of evaluating the role of Vitamin D as a potential risk factor for LE. Vitamin D’s role in musculoskeletal health has long been established, particularly in bone illnesses such as osteoporosis and osteomalacia. Its role, however, on tendon health and illnesses such as LE is only newly researched [6,9,10]. Vitamin D receptors are present in several tissues, including tendons, and Vitamin D has been reported to influence collagen production and tendon repair. From studies, Vitamin D is reported to enhance tenocyte proliferation, cells that form tendons, and induce collagen synthesis, crucial for tendon flexibility and resistance [6,7]. The anti-inflammatory action of Vitamin D might inhibit the inflammation cascade in tendinopathies and reduce degeneration in LE [11]. Vitamin D deficiency is widespread in India, and studies have confirmed that more than 80% of the population has suboptimal levels of Vitamin D [12,13]. This can be attributed to limited sun exposure, especially in urban areas, and foods that are consistently low in Vitamin D [14]. Our findings are in concordance with recently emerging clinical literature that has associated hypovitaminosis D with tendinopathies, especially, LE. Two recent case–control studies are noteworthy. Yaka et al. [9] found significantly lower levels of Vitamin D in patients with LE compared with controls, while El-Leithy et al. [10] also found higher rates of deficiency and worse symptom scores among patients with LE. These significant results from different countries strengthen the external validity of our finding. However the available literature is neither uniform nor consistent in findings. Systematic reviews find heterogeneity of effect sizes and results that are not consistent enough to initiate supplementation trials. Possible causes for such variation among studies include differences in study design (cross-sectional vs. prospective), sample size, case definitions and imaging confirmation, seasonal or geographic variations in Vitamin D levels, methods used for assay, and uncontrolled confounding factors (occupational pattern, BMI, diabetes, etc.). These factors underscore the fact that further randomized controlled trials targeting Vitamin D deficiency patients with LE are required to determine whether correction of deficiency alleviates the symptoms, functional outcome, or radiologic evidence of tendon healing. Our study has several limitations that need to be mentioned. First, the cross-sectional design makes it difficult to establish cause–effect relationship. Low Vitamin D could be a cause of LE, or even a consequence (e.g., reduced outdoor activity because of elbow pain leading to inadequate sunlight exposure). Second, this is a single-center study, and although the cases and control groups are age and sex matched, some residual confounding from factors such as occupational exposure, BMI, comorbidity, smoking, dietary intake, and sunlight exposure remains possible. Third, Vitamin D levels are known to exhibit seasonal variation in our population. Although our recruitment occurred over 12 months, we have not performed any season-stratified analyses. Finally, although our sample size was enough to detect the observed differences, larger multicentre population cohorts would be an ideal prerequisite to obtain more precise effect estimates and allow better subgroup analyses. In summary, our study adds to the recently emerging evidence of the association between low serum Vitamin D and the occurrence of LE and provides a basis for future prospective and interventional studies. If causal links are established, then Vitamin D assessment and correction may become a simple, inexpensive component of LE prevention and management strategies.
This is an important study that not only identified an independent association between low serum Vitamin D levels and LE but also met its primary objective of assessing Vitamin D as a risk factor for the condition. The serum Vitamin D level was significantly lower in patients with LE than in matched controls, while Vitamin D deficiency increased the odds of developing the disorder more than threefold. These findings suggest that insufficient Vitamin D may cause tendon degeneration or faulty tendon repair, thus providing a plausible explanation for the observed relationship. Given the high prevalence of Vitamin D deficiency in the study population, routine assessment and correction of Vitamin D status may prove to be a simple modifiable factor in the prevention and management of LE. More prospective and interventional studies will be needed to establish causality and assess the therapeutic benefit of supplementation with Vitamin D.
Low-serum Vitamin D levels predispose to the development of LE of the elbow. Routine assessment and correction of Vitamin D levels are a simple modifiable factor in the prevention and treatment of LE.
References
- 1. Whaley AL, Baker CL. Lateral epicondylitis. Clin Sports Med 2004;23:677-91, x. [Google Scholar] [PubMed]
- 2. Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N. Lateral epicondylitis: A review of pathology and management. Bone Joint J 2013;95-B:1158-64. [Google Scholar] [PubMed]
- 3. Akbar H, Akbar S, Saddique MN, Sarfraz MS. Prevalence of lateral epicondylitis among housewives in Lahore: A cross-sectional study. BMC Musculoskelet Disord 2024;25:815. [Google Scholar] [PubMed]
- 4. Levin D, Nazarian LN, Miller TT, O’Kane PL, Feld RI, Parker L, et al. Lateral epicondylitis of the elbow: US findings. Radiology 2005;237:230-4. [Google Scholar] [PubMed]
- 5. Hong QN, Durand MJ, Loisel P. Treatment of lateral epicondylitis: Where is the evidence? Joint Bone Spine 2004;71:369-73. [Google Scholar] [PubMed]
- 6. Mendes MM, Botelho PB, Ribeiro H. Vitamin D and musculoskeletal health: Outstanding aspects to be considered in the light of current evidence. Endocr Connect 2022;11:e210596. [Google Scholar] [PubMed]
- 7. Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A, et al. Vitamin D deficiency 2.0: An update on the current status worldwide. Eur J Clin Nutr 2020;74:1498-513. [Google Scholar] [PubMed]
- 8. Giustina A, Bilezikian JP, Adler RA, Banfi G, Bikle DD, Bikley NC, et al. Consensus statement on vitamin D status assessment and supplementation: Whys, whens, and hows. Endocrine Rev 2024;45:625-54. [Google Scholar] [PubMed]
- 9. Yaka H, Başbuğ V, Tekin AA, Özer M. Evaluation of the relationship between lateral epicondylitis and vitamin D. Jt Dis Relat Surg 2022;33:414-8. [Google Scholar] [PubMed]
- 10. El-Leithy SA, Adly NN, Galal S. Role of vitamin D in lateral epicondylitis among Egyptians. Egypt Rheumatol Rehabil 2023;50:61. [Google Scholar] [PubMed]
- 11. Lenoir H, Mares O, Carlier Y. Management of lateral epicondylitis. Orthop Traumatol Surg Res 2019;105(Suppl 8):S241-6. [Google Scholar] [PubMed]
- 12. Aparna P, Muthathal S, Nongkynrih B, Gupta SK. Vitamin D deficiency in India. J Family Med Prim Care 2018;7:324-30. [Google Scholar] [PubMed]
- 13. Ghosh A, Monisha S, Sunny AS, Diwakar L, Issac TG. Prevalence and patterns of vitamin D deficiency and its role in cognitive functioning in a cohort from South India. Sci Rep 2024;14:11215. [Google Scholar] [PubMed]
- 14. Ritu G, Gupta A. Vitamin D deficiency in India: Prevalence, causalities and interventions. Nutrients 2014;6:729-75. [Google Scholar] [PubMed]