Osteopoikilosis is a finding that does not affect bone healing in the context of a fracture.
Dr. Jorge Ogalde Bravo, Universidad Católica de la Santísima Concepción, Alonso de Ribera 2850, Concepción - 4030000, Chile. E-mail: jogaldeb@gmail.com
Introduction: Osteopoikilosis (OPK) is a benign osteosclerotic dysplasia that is almost always asymptomatic. Its radiographic pattern can mimic osteoblastic metastases. Its coexistence with fractures is rare, and there is no demonstrated increased risk of fracture or issues with bone healing. Our objective was to present a case of an ankle fracture with an incidental finding of OPK and highlight its clinical implications.
Clinical Report: A 21-year-old male presented with pain and swelling after twisting his left ankle. X-rays and computed tomography (CT) scan revealed a comminuted medial malleolus fracture and avulsion of the lateral process of the talus, in addition to multiple well-defined sclerotic foci in the distal tibia, fibula, and talus, consistent with OPK. Laboratory tests were normal, except for vitamin D at 17 ng/mL. No associated endocrinological or rheumatological findings were noted. Open reduction and internal fixation of the medial malleolus was performed using 2.5 mm headless cannulated screws. The outcome was favorable with no pain, full bone healing, 0° dorsiflexion, and 60° plantar flexion at 17-month follow-up.
Discussion: OPK shows symmetric epimetaphyseal images, with no periosteal reaction or soft tissue involvement; recognizing this pattern prevents unnecessary invasive studies and anxiety due to differential diagnosis with metastases. In fractures, management should follow standard orthopedic principles, as OPK does not affect biomechanics or healing.
Conclusion: OPK is a “do not touch” lesion; diagnosis is based on radiographs or CT scans, differentiating it from malignant processes. In concurrent fractures, standard treatment yields successful results.
Keywords: Osteopoikilosis, ankle fracture, medial malleolus, computed tomography, differential diagnosis.
Osteopoikilosis (OPK), also known as “disseminated condensing osteopathy,” is a rare bone disorder first described in 1915 [1,2]. It is a sclerotic dysplasia of autosomal dominant genetic origin, associated with a mutation in the LEMD3 gene, which regulates protein signaling [1,2,3]. Three types of presentations are described: speckled, striated, and mixed [2]. Its estimated prevalence is 1/50,000 people/year, and the diagnosis is usually incidental, as most patients are asymptomatic [1,4,5]. It affects both sexes equally across all ages but is reported more often in adult males [5,6]. This condition is typically asymptomatic and may be discovered at any age [2,3,6]. It presents as multiple, symmetrical, well-defined areas of bone condensation in the epiphysis and metaphysis – primarily in the carpal and tarsal bones, pelvis, and long bones [2]. A key feature is that these lesions do not show radionuclide uptake, which helps differentiate them from blastic bone metastases [7]. Although some associations with rheumatological, endocrinological diseases, or genetic syndromes have been reported, coexistence with fractures is rarely described in the literature [3,5,8]. Differentiating the benign lesions of OPK from other conditions like bone metastases is critical to avoid unnecessary invasive tests like biopsies and to prevent the emotional distress of a cancer workup [6,7]. Here, we present a case of ankle fracture with an incidental diagnosis of OPK, managed surgically with satisfactory functional outcomes.
A 21-year-old male with no significant medical history experienced a twisting injury to the left ankle, resulting in pain, bruising, and swelling, without skin breakage or neurovascular compromise. He presented to the emergency department, where anteroposterior, lateral, and mortise ankle X-rays and a computed tomography (CT) scan revealed a comminuted and displaced medial malleolus fracture and avulsion fracture of the lateral process of the talus. In addition, multiple small (2–16 mm), punctate, well-defined, round and oval-shaped sclerotic lesions were found symmetrically in the distal left tibia, fibula, and talus (Fig. 1a and b), sparing the joint space and without affecting bone architecture or soft tissues.

Figure 1: (a): Pre-op anteroposterior (AP) and lateral X-rays of the left ankle showing multiple small (2–10 mm), well-defined, oval-shaped sclerotic lesions symmetrically distributed in the distal tibia, fibula, and talus, with no cortical disruption or periosteal reaction. A comminuted medial malleolus fracture is also visible. (b): Post-op AP and lateral X-rays showing the same sclerotic lesions and a fixed medial malleolus fracture with two cannulated screws.
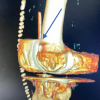
The ankle was immobilized in a neutral dorsiflexion position using a backslab, and the patient was admitted for further evaluation and surgical planning. During hospitalization, an extensive evaluation showed no associated conditions, skin lesions, or signs of endocrine dysfunction. Laboratory tests, including electrolytes, hematology, and urinalysis, were all within normal ranges. Thyroid and parathyroid hormones were normal. Vitamin D was decreased to 17 ng/mL. X-rays of other limbs showed similar well-defined sclerotic lesions in the distal radius and carpal bones (Fig. 2). CT scan of the ankle showed well-defined hyperintense foci in the cancellous bone of the distal tibia, consistent with OPK (Fig. 3).
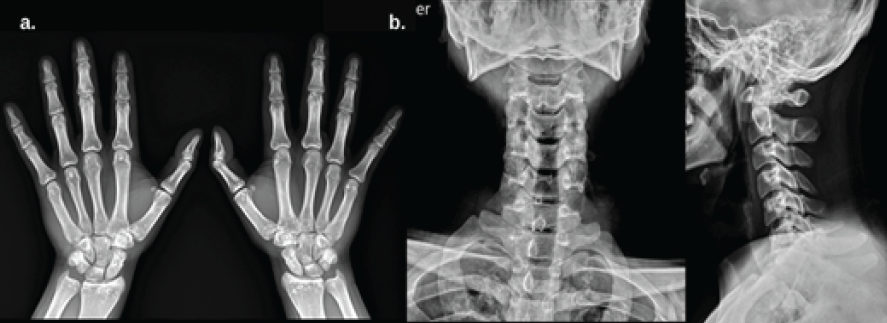
Figure 2: (a) Anteroposterior (AP) X-ray of both hands showing well-defined sclerotic lesions in the distal radius and carpal bones, with no cortical involvement or periosteal reaction. (b) AP and lateral cervical spine X-rays showing symmetrically distributed sclerotic foci in vertebral bodies, without disc involvement or structural collapse.
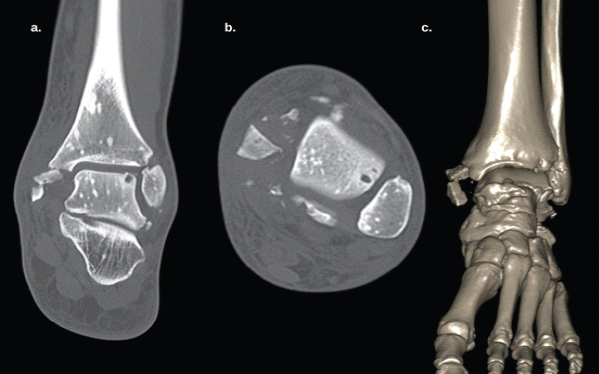
Figure 3: (a) Coronal computed tomography (CT) scan of the left ankle showing multiple well-defined, symmetrically distributed, spherical/oval radiopaque lesions in the distal tibia, fibula, and talus, without bony architectural disruption. A comminuted medial malleolus fracture is also visible. (b) Axial CT showing similar findings in the fibula and talus. (C) 3D CT reconstruction.
The case was reviewed with the hospital’s bone tumor team. Based on clinical examination, normal laboratories, and imaging findings, a diagnosis of OPK was confirmed, and no further studies were deemed necessary.
Surgery involved an open reduction of the medial malleolus through a medial ankle approach. The sagittal fracture line was stabilized temporarily with a Kirschner wire, and definitive fixation was achieved with two 2.5 mm headless cannulated compression screws (38 mm and 35 mm in length) (Fig. 1b). One-month post-op, the patient began physiotherapy, walking without complications, and ascending/descending stairs without issues. He reported only occasional pain, Visual Analog Scale 2/10 when walking on uneven surfaces. He returned to work as a fisherman 5 weeks after surgery. After completing physical therapy, follow-up was periodic. At his last check-up, 17-month post-op, he had no pain or complaints and exhibited normal function (neutral dorsiflexion and 60° plantar flexion).
Although OPK is typically asymptomatic, isolated cases exist where patients present with fractures after trauma. However, literature reviews do not show an increased fracture risk in OPK patients. Chou TF et al. reviewed multiple fracture cases in OPK and found no increased risk of pathological fracture, and healing was the same as in patients without OPK. Clinical experience supports that bone healing in OPK is normal and without complications [7]. Diagnosis is usually based on typical radiographic findings – multiple, well-defined, round/oval, symmetrical sclerotic lesions in the epiphysis and metaphysis of long bones, pelvis, wrist, and tarsal bones [6]. These images can mimic osteoblastic metastases, particularly in symptomatic or undiagnosed patients. Recognizing OPK is essential to avoid invasive diagnostic procedures like biopsies or single photon emission CT [6,9,10]. Differential diagnoses include mastocytosis, synovial chondromatosis, tuberous sclerosis, osteosclerotic myeloma, and melorheostosis [4,11]. Awareness and a high index of suspicion are a key when radiologic findings are compatible. Although X-rays are the first step, bone scans can help rule out metastases – OPK shows normal bone scans, whereas metastases do not. In this case, the diagnosis was confirmed by CT and normal laboratories (including sex- and size-adjusted values). Vitamin D was slightly low (17 ng/mL), a common finding in the Chilean population, and was corrected with oral supplementation, with no impact on surgical management [11,12]. Literature on fractures in OPK patients is limited. Some suggest that fracture comminution in young patients may relate to reduced bone mass, but there is no evidence to suggest that OPK alters bone strength or healing. Therefore, fractures should be treated using standard orthopedic principles [9]. In this case, the ankle fracture was treated successfully with internal fixation using headless cannulated screws, ensuring adequate stability and full healing with normal function. This aligns with the few published reports showing that OPK does not interfere with bone healing or mechanical stability. OPK is a classic “do not touch” lesion. Correct diagnosis is essential to avoid unnecessary biopsies or additional imaging, which are typically not needed [5,9,13].
OPK is a benign osteosclerotic condition that does not increase the risk of pathological fractures. Documented clinical cases (in various bone locations: Wrist, elbow, humerus, tibia, femur, etc.) show that fractures in patients with OPK follow a normal healing course after appropriate treatment for each injury. It is essential to recognize the characteristic radiological pattern of OPK in order to distinguish it from malignant processes (such as bone metastases), but once the diagnosis is established, OPK does not require any specific additional treatment. In summary, although OPK may occasionally coincide with traumatic fractures, the available evidence suggests that there is no causal relationship: OPK does not cause increased bone fragility nor does it affect fracture mechanics or healing.
OPK is a benign incidental radiological finding that can mimic bone metastases but does not compromise bone strength or healing. This case is relevant because it demonstrates that even in the context of a complex ankle fracture, standard orthopedic management is safe and effective, avoiding unnecessary interventions.
References
- 1. Mohsenpour B, Ahmadi A. Osteopoikilosis: A case report. J Med Case Rep 2023;17:292. [Google Scholar] [PubMed]
- 2. Rosa‐Juana TP, Ana AL, Julia MD, Sara CP. Osteopoikilosis-the incidental finding of a rare bone dysplasia: A case report. Clin Case Rep 2024;12:e9191. [Google Scholar] [PubMed]
- 3. Liu B, Ma L, Zhang B, Wu G. Distal radius fracture combined with osteopoikilosis in young adults: The first case report. Asian J Surg 2025;48:1768-9. [Google Scholar] [PubMed]
- 4. Mukai T, Morita Y. Osteopoikilosis. Rheumatology (Oxford) 2022;61:879-80. [Google Scholar] [PubMed]
- 5. Alghamdi BA. A rare case of hereditary bone dysplasia: Osteopoikilosis in a mother and her son. Cureus 2024;16:e61477. [Google Scholar] [PubMed]
- 6. Nascimento AF, Araújo FC. Osteopoikilosis – the importance of recognizing a rare but benign bone disorder. ARP Rheumatol 2022;1:177-8. [Google Scholar] [PubMed]
- 7. Chou TF, Hsiao CH. Osteopoikilosis: Benign bone islands in periarticular bones. Med J Aust 2022;217:397. [Google Scholar] [PubMed]
- 8. Al-Bourini O, Lotz J, Wienbeck S. Radiological imaging in osteopoikilosis. Advances in the Fiel od X-Rays and Imaging Techniques 2018;190:499-502. [Google Scholar] [PubMed]
- 9. Ye C, Lai Q, Zhang S, Gao T, Zeng J, Dai M. Osteopoikilosis found incidentally in a 17-year-old adolescent with femoral shaft fracture: A case report. Medicine (Baltimore) 2017;96:e8650. [Google Scholar] [PubMed]
- 10. Syrycka J, Kubicka E, Polowczyk B, Bolanowska-Tyszko A, Podgajny Z, Bolanowski M. Low back pain and osteosclerotic bone lesions suggestive of metastases: A mask of osteopoikilosis. Pol Arch Intern Med 2020;130:249-51. [Google Scholar] [PubMed]
- 11. Schweitzer D, Amenábar PP, Botello E, López M, Saavedra Y, Klaber I. Prevalence of Vitamin D Insufficiency and Deficiency in Older Adults with Hip Fracture in Chile. Chilean Medical Journal 2016;144:175-80. [Google Scholar] [PubMed]
- 12. Amezcua-Guerra LM, Mansilla-Lory J, Fernández-Tapia S, Pijoan C, Leboreiro I, Martínez-Lavín M, et al. Osteopoikilosis in an ancient skeleton: More than a medical curiosity. Clin Rheumatol 2005;24:502-6. [Google Scholar] [PubMed]
- 13. Madeira N, Ganhão S, Ferreira RM, Duarte AC, Freitas R, Miranda LC. Osteopoikilosis: Case series from portuguese rheumatology centers. Acta Reumatol Port 2019;44:78-83. [Google Scholar] [PubMed]