Two main factors contribute to non-union: 1. Inadequate immobilization/stabilization, and 2. Compromise of biology at the fracture site. Achieving union at a non-union site requires adequately addressing both these issues.
Dr. Manjesh Reddy S V , Department of Orthopaedic Surgery, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi - 110001, India. E-mail: svmanjeshreddy@gmail.com
Introduction: Long-standing non-unions of the humeral shaft with established pseudoarthrosis are rare and pose substantial challenges in management. This case report describes the successful treatment of such a patient.
Case Report: A 60-year-old male patient presented with a 40-year history of a humeral shaft fracture that had progressed to non-union with pseudoarthrosis. The patient underwent open reduction and internal fixation using a proximal humeral interlocking osteosynthesis system, augmented with an intramedullary fibular strut graft for added stability and an autogenous cancellous bone graft from the iliac crest to enhance healing. Post-operative radiological imaging confirmed successful bone healing, and the patient achieved a good range of motion in the affected arm.
Conclusion: This case demonstrates that long-standing humeral shaft non-unions can achieve successful clinical outcomes when managed with mechanical stabilization and biological augmentation.
Keywords: Non-union, pseudoarthrosis, humerus, shaft fractures, bone graft.
Humeral shaft fractures constitute approximately 2% of all fractures, with falls being the most common cause [1]. While most humeral shaft fractures are treated conservatively with cast immobilization, a subset of them develop non-union [1,2,3,4,5]. Non-union occurs in approximately 10% of conservatively treated humeral shaft fractures and around 15% of surgically treated cases [2,3,4,5,6]. Factors such as the severity of impact, fracture pattern, bone quality, and patient-related factors can influence healing [3,4]. Patients may experience difficulty performing daily activities due to instability and discomfort [2,5]. Long-standing non-unions, especially those with established pseudoarthrosis, present unique surgical challenges [1,2,3,4,5]. This report describes the successful management of a rare case of a 40-year-old humeral shaft non-union with pseudoarthrosis, emphasizing the surgical technique employed to achieve a good clinical outcome.
A 60-year-old male presented to our outpatient department with a noticeable deformity in his left arm, which was substantially limiting his daily activities. He had a history of smoking and hypertension. The patient reported a history of a closed fracture of the left humeral shaft 40 years prior, treated conservatively with cast immobilization. Clinical examination demonstrated significant deformity and functional impairment of the left arm. His shoulder range of motion was significantly limited with 30° of flexion, 15° of extension, 30° of abduction, 15° of adduction, 20° of internal rotation, and 15° of external rotation. Elbow flexion was also restricted, ranging from 15° to 70°. The constant shoulder score was 21. X-ray examination confirmed an oligotrophic non-union with pseudoarthrosis at the junction of the proximal and mid-third of the left humeral shaft (Fig. 1). His pre-operative evaluations, including white blood cell count (7500 cells/mm3), C-reactive protein (0.7 mg/dL), and erythrocyte sedimentation rate (15 mm/h), were within normal limits.
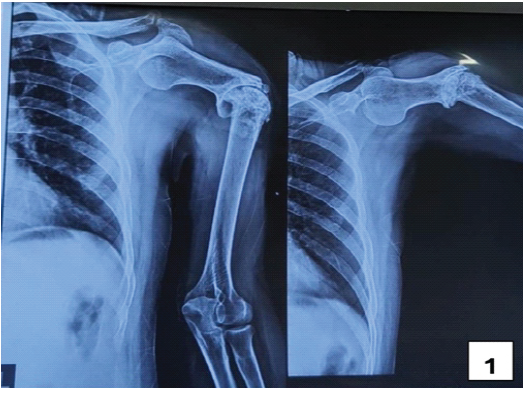
Figure 1: Pre-operative X-ray showing oligotrophic nonunion with pseudoarthrosis at the junction of the proximal and mid-third of the left humeral shaft.
The non-union site was accessed through an anterolateral approach to the humerus. The proximal plane was developed between the deltoid and pectoralis major, whereas the distal plane was identified between the medial and lateral fibers of the brachialis, after retracting the biceps medially. Exposure of the non-union site revealed a well-formed pseudoarthrosis with an adjacent pseudo-synovial capsule (Fig. 3 and 4). The pseudo-synovial capsule was carefully excised. Bone ends were freshened by removing approximately 1.5 cm of bone on either side until a bleeding edge was visible. The medullary canal was opened on both sides to facilitate bone grafting.

Figure 3: Intraoperative image of non-union site showing pseudoarthrosis.

Figure 4:Intraoperative image of non-union with pseudoarthrosis site distracted.
A 5 cm segment of the fibula was harvested from the middle third of the contralateral leg and split longitudinally into four pieces. The entire length of each fibular strut was then inserted into the medullary canal of the humerus. The non-union site was then reduced and stabilized with an 8-hole proximal humeral interlocking plate in compression mode. Cancellous bone graft, obtained from the ipsilateral iliac crest, was placed at the non-union site. An intraoperative tissue sample was obtained and sent for culture. The wound was closed in layers, and an antiseptic dressing was applied.
Postoperatively, the limb was immobilized with a universal shoulder immobilizer. There were no post-operative neurovascular deficits. The first post-operative dressing was performed on day 3, with suture removal on day 14. A staged rehabilitation program was initiated, beginning with passive pendulum exercises from the 3rd post-operative week onward. Assisted range of motion exercises were introduced from the 5th week, progressing to active range of motion exercises from the 9th week. At 6 months postoperatively, his shoulder range of motion included 110° of flexion, 30° of extension, 130° of abduction, 25° of adduction, 60° of internal rotation, and 35° of external rotation (Figs. 5, 6, 7, 8, 9, 10]. Elbow flexion was restored to 0–135°. Constant Shoulder Score improved to 80, indicating a good functional outcome. X-ray at 6 months showed a callus bridge across the non-union site (Fig. 2).

Figure 2: Post-operative 6-month follow-up X-ray.

Figures 5 to 10
Postoperative improvement in shoulder range of motion at 6 months with 110° of flexion (Fig. 5), 30° of extension ((Fig. 6), 130° of abduction ((Fig. 7), 25° of adduction ((Fig. 8), 60° of internal rotation ((Fig. 9), and 35° of external rotation ((Fig. 10).
Non-union, defined as the failure of a fracture to heal within an expected timeframe, arises from a complex interplay of biological and mechanical factors [3]. High-risk fracture patterns, especially in polytrauma, can compromise bone healing. Biological factors, including diabetes, smoking, severe neuropathy, and non-steroidal anti-inflammatory drug use, further impede the healing process [3,6]. Mechanically, inadequate stability, improper implant selection, excessive rigidity, or inadequate fixation can also lead to non-union [7]. In our patient, his substantial smoking history and inadequate immobilization were possible risk factors contributing to the non-union. Surgical management of non-union demands a tailored approach, considering the patient’s overall health, fracture characteristics, previous treatments, and the presence of complicating factors [1,2,3,4,5,6]. Various techniques exist, including internal fixation with plating, intramedullary nailing, allografts, and Ilizarov external fixation [2,5]. Each technique carries its own set of advantages, disadvantages, and success rates [1,5,6,7]. Based on a thorough assessment of patient-specific factors, the chronicity of the non-union, presence of pseudoarthrosis, and the nature of the injury, we determined that internal fixation with plating and bone grafting would be the most appropriate approach for this case [2]. The surgical approach was hampered by several factors. The soft tissue surrounding the non-union site exhibited significant alterations, making dissection both difficult and meticulous to avoid neurovascular structures. Removal of the pseudocapsule also proved challenging. Furthermore, the bone quality itself was poor, adding to the complexity of the procedure. Despite these intraoperative challenges posed, the surgery was completed without any intraoperative or post-operative complications. We selected the fibular strut graft due to its inherent structural strength, enhanced screw purchase, and its ability to promote bone healing. Its large contact area with the endosteal surface of the humerus further promotes bone healing [1,8,9]. To complement the graft and ensure stable fixation, we opted for an 8-hole proximal humeral interlocking plate. To address the challenging 40-year-old non-union, we utilized the autologous cancellous bone graft from the iliac crest, chosen for its superior osteogenic properties [1,10]. Postoperatively, the patient began a tailored rehabilitation initially focused on pain reduction, followed by a gradual increase in range of motion and strengthening exercises. A long-term follow-up would be needed to fully assess the functional outcome. We anticipate that the combination of stable fixation, osteogenic properties of the bone graft, and a dedicated rehabilitation program would ultimately result in a full functional recovery and improved quality of life for the patient.
This case demonstrates the successful treatment of a long-standing humeral shaft non-union with established pseudoarthrosis, achieving complete healing and good functional outcomes with plate fixation and bone grafting. The effectiveness of combining a fibular strut graft for stability with a cancellous bone graft for biological enhancement is also highlighted.
This case report highlights the body’s remarkable adaptive capacity, even in long-standing non-unions with pseudoarthrosis. It underscores the importance of adequately addressing both mechanical and biological factors through rigid fixation, meticulous tissue handling, and bone grafting to achieve favorable functional outcomes.
References
- 1. Naclerio EH, McKee MD. Approach to humeral shaft nonunion: Evaluation and surgical techniques. J Am Acad Orthop Surg 2022;30:50-9. [Google Scholar] [PubMed]
- 2. Tapscott DC, Paxton ES. Decision-making and management of proximal humerus nonunions. Orthop Clin North Am 2021;52:369-79. [Google Scholar] [PubMed]
- 3. Nicholson JA, Makaram N, Simpson A, Keating JF. Fracture nonunion in long bones: A literature review of risk factors and surgical management. Injury 2021;52 Suppl 2:S3-11. [Google Scholar] [PubMed]
- 4. Oliver WM, Searle HK, Ng ZH, Molyneux SG, White TO, Clement ND, et al. Factors associated with humeral shaft nonunion. J Shoulder Elbow Surg 2021;30:2283-95. [Google Scholar] [PubMed]
- 5. Orapiriyakul W, Apivatthakakul V, Theppariyapol B, Apivatthakakul T. Humerus shaft fractures, approaches and management. J Clin Orthop Trauma 2023;43:102230. [Google Scholar] [PubMed]
- 6. Dedhia N, Ranson RA, Rettig SA, Konda SR, Egol KA. Nonunion of conservatively treated humeral shaft fractures is not associated with anatomic location and fracture pattern. Arch Orthop Trauma Surg 2023;143:1849-53. [Google Scholar] [PubMed]
- 7. Sanchez G, Vargas M, Gordon AM, Golub I, Ashraf A, Diamond K, et al. Risk factors for nonunion following open reduction and internal fixation for proximal humerus fractures. Eur J Orthop Surg Traumatol 2023;33:883-8 [Google Scholar] [PubMed]
- 8. Padegimas EM, Nicholson TA, Chang G, Hebert-Davies J, Namdari S. Outcomes of open reduction and internal fixation of proximal humerus fracture dislocations. J Shoulder Elbow Surg 2021;30:2331-5. [Google Scholar] [PubMed]
- 9. Wright TW, Miller GJ, Vander Griend RA, Wheeler D, Dell PC. Reconstruction of the humerus with an intramedullary fibular graft. A clinical and biomechanical study. J Bone Joint Surg Br 1993;75:804-7. [Google Scholar] [PubMed]
- 10. Bégué T, Mouchantaf M, Aurégan JC. Aseptic humeral shaft nonunion. Orthop Traumatol Surg Res 2023;109:103462. [Google Scholar] [PubMed]










