Early recognition of stiff-person syndrome is crucial to prevent misdiagnosis and unnecessary surgeries.
Dr. Lessoued Alaeddine, Department of Orthopedic Surgery, Kassab Hospital, Tunisia, Residence Diar Ben Mahmoud, Block A4, Apartment 21, El Agba, Manouba, Tunisia. E-mail: lessoued1992@gmail.com
Introduction: Stiff-person syndrome (SPS) is a rare autoimmune neurological disorder characterized by progressive muscle rigidity and spasms. While it predominantly affects adults, pediatric cases are exceptionally rare, often leading to delayed diagnosis due to non-specific early clinical manifestations.
Case Report: We report the case of an 11-year-old boy with progressive gait abnormalities and rigidity, initially misdiagnosed as an orthopedic disorder. The patient exhibited a forward-leaning posture, absent lumbar lordosis, and significant muscle tightness, leading to a primary surgical intervention. Despite initial improvement, symptom recurrence prompted further evaluation, ultimately raising suspicion of SPS. The absence of pyramidal or extrapyramidal signs complicated early diagnosis, highlighting the challenges in recognizing SPS in pediatric patients.
Discussion: SPS diagnosis relies on clinical criteria, serological markers, and electromyography. Autoantibodies against glutamic acid decarboxylase (anti-GAD) are commonly associated, although other markers may be present in atypical forms. Pediatric SPS is often misdiagnosed as dystonia, metabolic myopathy, or an orthopedic disorder. The underlying pathophysiology involves autoimmune-mediated dysfunction of GABAergic inhibitory neurons, resulting in loss of muscle control. Treatment strategies include immunomodulatory therapies such as intravenous immunoglobulins and rituximab, alongside symptomatic management with baclofen and benzodiazepines. Long-term rehabilitation is essential to prevent complications and improve functional outcomes.
Conclusion: This case underscores the diagnostic complexity of pediatric SPS and the importance of multidisciplinary management. Early recognition is critical to prevent unnecessary surgical interventions and optimize therapeutic strategies. Greater awareness and further research are necessary to refine diagnostic approaches and treatment protocols in pediatric SPS.
Keywords: Stiff-person syndrome, pediatrics, muscle rigidity, autoimmune neurology, anti-glutamic acid decarboxylase antibodies, immunotherapy.
Stiff-person syndrome (SPS) is a rare neurological disorder of autoimmune origin, characterized by progressive muscle rigidity and often associated with involuntary spasms [1]. Although it primarily affects adults, pediatric cases remain exceptional, which complicates their diagnosis in younger patients. SPS is frequently linked to the presence of autoantibodies targeting glutamic acid decarboxylase (anti-GAD), but other autoantibodies have also been identified in atypical forms of the disease [1]. The lack of specific clinical signs in the early stages of the disease, coupled with the rarity of pediatric cases, often leads to a complex and delayed diagnosis. This article presents a rare pediatric case of SPS in an 11-year-old boy and discusses the diagnostic and therapeutic management, as well as the challenges associated with this uncommon neurological disorder in children.
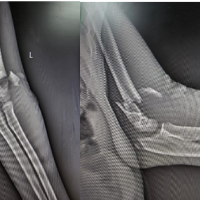
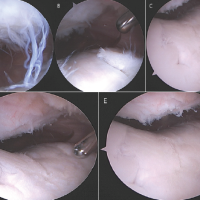
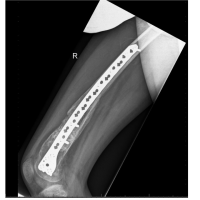
An 11-year-old boy, with no notable medical history and from a non-consanguineous marriage, was monitored from birth, which occurred without major complications. He presented with an abnormal gait and rigid posture since the age of 5 years, prompting his parents to seek specialized advice. He was initially evaluated for possible neuromuscular disorders rather than cerebral palsy, which typically manifests in the neonatal period. On clinical examination, the child had a forward-leaning posture, an absent lumbar lordosis, and a stiff gait. Muscular examination revealed tightness of the hamstrings and hip adductors, with a significant limitation in hip mobility, notably a flexion limited to 20° when the knees were extended. This stiffness was slightly improved with knee flexion, reaching up to 100°, suggesting a muscular retraction origin. Tightness of the tensor fasciae latae, sartorius, and hamstrings was also observed, along with a marked limitation of hip abduction, reduced to only 10°. Neurological tests showed no reflex abnormalities or pyramidal or extrapyramidal signs. Further investigations included normal radiographs (no scoliosis, no hip dislocation), a normal cerebral and spinal magnetic resonance imaging (MRI), and normal electromyography, which argued against cerebral palsy or primary neuromuscular disease. The initial diagnosis seemed to be an orthopedic disorder. Before surgical consideration, the patient underwent hospitalization in the Department of Physical Medicine, followed by several months of well-conducted rehabilitation targeting joint stiffness, without clinical improvement. Following rehabilitation, surgical management was considered, involving a proximal hamstring tenotomy and an external tenotomy of the tensor fascia lata. This intervention resulted in immediate improvement in joint ranges of motion. However, after 1 week of traction and 2 months of rehabilitation, a recurrence of symptoms occurred. Four months after the surgical procedure, muscle retraction resumed with the loss of lumbar lordosis, contracture of the lumbar paraspinal muscles, and a reappearance of the stiff gait. The recurrence of contractures despite appropriate surgical and rehabilitative management, combined with the absence of any structural or neurological lesion, raised suspicion of SPS. The diagnosis was further supported by a remarkable clinical improvement under targeted medical treatment, including rituximab and benzodiazepines.
SPS is a rare neurodegenerative disorder. When it is diagnosed in children, it is often confused with other neurological or muscular disorders, such as dystonias, metabolic myopathies, or even orthopedic disorders. This case illustrates the diagnostic challenges associated with this disease in the pediatric population. In adults, SPS typically presents with well-defined symptoms, but in children, the clinical signs are often non-specific, leading to significant diagnostic delay [1]. The diagnosis of SPS relies on several clinical criteria. Progressive muscle rigidity is generally predominant along the body axis and is often associated with muscle spasms triggered by sensory stimuli, such as noise or light. This phenomenon is well documented in adults [2], but its observation in children remains rare. In our patient’s case, the rapid recurrence following surgery and the progressive evolution of muscle contractures were key indicators that guided the diagnosis toward SPS, despite the absence of obvious neurological signs during the initial examination [3]. The failure of prolonged rehabilitation and orthopedic surgery to provide lasting improvement, combined with the normal neurological and imaging findings, pointed toward a functional disorder of inhibitory motor pathways. Another essential criterion for diagnosing SPS in pediatric patients is the detection of anti-GAD autoantibodies in the serum or cerebrospinal fluid [4]. However, while the presence of these antibodies is a common marker [5], other autoantibodies may be involved in the pathogenesis of the disease, such as anti-amphiphysin and anti-gephyrin. Therefore, additional immunological tests are crucial to confirm the diagnosis, although these tests are not always available in all healthcare centers, which can be an obstacle to early diagnosis [6]. The underlying mechanism of SPS remains poorly understood, although several theories have been proposed. It is generally considered an autoimmune disease in which the immune system mistakenly attacks the central nervous system, particularly affecting GABAergic inhibitory neurons in the spinal cord and brain. This degradation leads to a loss of inhibitory control over muscles, resulting in the characteristic rigidity and spasms of the disease. In pediatrics, it is often difficult to differentiate the symptoms of SPS from those of other neurological disorders, which justifies a thorough follow-up and a detailed differential diagnosis [7]. In this patient, the main differential diagnoses initially considered were neuromuscular disorders (such as congenital myopathies, metabolic myopathies, and dystonia) and cerebral palsy. Cerebral palsy was excluded because the patient had a normal perinatal history, normal brain MRI, and no pyramidal signs. Neuromuscular disorders were considered unlikely due to the absence of muscle weakness, normal creatine kinase levels, and normal electromyography. The absence of scoliosis, hip dislocation, or bony deformities further argued against orthopedic or structural causes. Management of SPS in pediatrics presents several challenges. Treatment primarily involves immunomodulatory agents, such as intravenous immunoglobulins and rituximab, which have shown some efficacy in reducing inflammation and suppressing the abnormal immune response. These treatments are often combined with symptomatic medications, such as baclofen and benzodiazepines, which help control muscle rigidity and reduce spasms. Baclofen, a muscle relaxant, is particularly useful for relieving stiffness and improving mobility in patients with SPS [8]. Other therapies, such as plasmapheresis or azathioprine, may be considered in cases resistant to first-line treatments [9]. The ultimate confirmation in our case came from the favorable response to immunomodulatory treatment with rituximab and symptomatic improvement under benzodiazepines. Due to the rarity of the disease in children, there is a wide variety of clinical forms of pediatric SPS, ranging from localized forms to generalized forms. Some studies have also highlighted paraneoplastic forms associated with underlying cancers, but these are exceptionally rare. Moreover, milder forms with less pronounced symptoms and slower progression have been reported in the literature. Long-term follow-up of pediatric patients with SPS is crucial to adjust treatments and minimize the side effects of therapies [10]. In our patient’s case, a multidisciplinary approach was implemented, involving neurologists, orthopedists, and physiotherapists. Collaboration between these various specialties is essential to optimize care, prevent complications, and improve the patient’s quality of life. Regular physical rehabilitation is also indispensable to preserving joint mobility and avoiding additional muscle contractures [11].
The case presented highlights the diagnostic complexity of SPS in pediatrics and emphasizes the need for a multidisciplinary approach in managing this rare disease. The clinical progression, marked by rapid recurrence after surgical intervention, was a key indicator that led to suspicion of SPS. This case underscores the importance of a rigorous neurological evaluation and immunological testing in cases of unexplained muscle stiffness and gait abnormalities, even in children. Early recognition of neurological signs prevents the need for repeated surgical interventions and allows for rapid referral to specialized care. Ongoing research into pediatric forms of SPS is crucial to better understand its evolution, pathogenesis, and the most effective therapeutic strategies.
In pediatric patients presenting with unexplained stiffness and gait abnormalities, particularly those unresponsive to conventional orthopedic treatment, early neurological evaluation and immunological testing are essential to avoid misdiagnosis and ensure timely management of rare conditions like SPS.
References
- 1. Dalakas MC. Stiff person syndrome: advances in pathogenesis and therapeutic interventions. Curr Treat Options Neurol. 2009 Mar;11(2):102–10. [Google Scholar] [PubMed]
- 2. Baizabal-Carvallo JF, Jankovic J. Stiff-person syndrome: insights into a complex autoimmune disorder. J Neurol Neurosurg Psychiatry. 2015 Aug;86(8):840–8. [Google Scholar] [PubMed]
- 3. Meinck HM, Thompson PD. Stiff man syndrome and related conditions. Mov Disord. 2002 Sept;17(5):853–66. [Google Scholar] [PubMed]
- 4. Dalakas MC. Advances in the pathogenesis and treatment of patients with stiff person syndrome. Curr Neurol Neurosci Rep. 2008 Jan;8(1):48–55. [Google Scholar] [PubMed]
- 5. Bose S, Jacob S. Stiff-person syndrome. Pract Neurol. 2025 Jan 16;25(1):6–17. [Google Scholar] [PubMed]
- 6. Clardy SL, Lennon VA, Dalmau J, Pittock SJ, Jones HR, Renaud DL, et al. Childhood onset of stiff-man syndrome. JAMA Neurol. 2013 Dec;70(12):1531–6. [Google Scholar] [PubMed]
- 7. McKeon A, Robinson MT, McEvoy KM, Matsumoto JY, Lennon VA, Ahlskog JE, et al. Stiff-man syndrome and variants: clinical course, treatments, and outcomes. Arch Neurol. 2012 Feb;69(2):230–8. [Google Scholar] [PubMed]
- 8. Geffen S, Chiang N. Successful Treatment of Stiff Person Syndrome with Intrathecal Baclofen. J Rehabil Med Clin Commun. 2019;2:1000016. [Google Scholar] [PubMed]
- 9. Mercure-Corriveau N, Roy S, Hu C, Crowe EP, Zhu X, Obando D, et al. Therapeutic plasma exchange in the management of stiff person syndrome spectrum disorders: a case series and review of the literature. Ther Adv Neurol Disord. 2023 July 24;16:17562864231180736. [Google Scholar] [PubMed]
- 10. Yeshokumar AK, Sun LR, Newsome SD. Defining the Expanding Clinical Spectrum of Pediatric-Onset Stiff Person Syndrome. Pediatr Neurol. 2021 Jan;114:11–5. [Google Scholar] [PubMed]
- 11. Vaiyapuri A, Kashyap P, Kashyap N, Muthusamy H, Unnikrishnan R, Alqahtani M. Is Stiff Person Syndrome Benefited by Physical Therapy Intervention? Summary of Case Reports. Biomed Res Int. 2019;2019:5613680. [Google Scholar] [PubMed]