Subcutaneous emphysema of the upper limb following blunt trauma and scapular fracture is rare but often benign. Differentiating it from serious infections like necrotizing fasciitis is crucial to avoid overtreatment, and early imaging can aid in accurate diagnosis and safe conservative management.
Dr. Manveer Singh, Department of Orthopaedics, All India Institute of Medical Sciences, Marudhar Industrial Area, 2nd phase, M.I.A. 1st phase, Basni, Jodhpur - 342005, Rajasthan, India. E-mail: manveerdhillon3@gmail.com
Introduction: Subcutaneous emphysema (SE) of the upper extremity is a rare condition, typically associated with penetrating trauma, infections, or chest injuries. Its occurrence following blunt trauma with an isolated scapular fracture is exceedingly uncommon and may mimic more serious conditions such as necrotizing fasciitis. We present a rare case of upper-limb SE associated with an open scapular fracture and propose a diagnostic approach to distinguish benign SE from limb-threatening infections.
Case Report: A 65-year-old male presented with pain and swelling in the right upper limb following a fall from a two-wheeler. Clinical examination revealed a laceration over the posterior axillary fold and extensive crepitus extending to the elbow. Radiographs and computed tomography imaging confirmed SE without intrathoracic involvement and revealed an extra-articular scapular body fracture. The patient underwent wound debridement and was treated with antibiotics. The scapular fracture was managed conservatively. The patient had an uneventful recovery, and follow-up showed complete resolution of symptoms.
Conclusion: Post-traumatic SE of the upper limb can present similarly to necrotizing soft tissue infections but is often benign. Careful clinical assessment, appropriate imaging, and close monitoring are essential. Awareness of this rare presentation in the context of scapular fractures helps prevent overtreatment and unnecessary surgical intervention.
Keywords: Subcutaneous emphysema, scapular fracture, benign emphysema, upper-limb trauma.
Subcutaneous emphysema is defined by the presence of air within the subcutaneous soft tissue planes and is most commonly encountered in association with thoracic trauma, pneumothorax, or gas-forming infections such as necrotizing fasciitis [1]. However, rare cases have been reported where subcutaneous emphysema occurs following minor trauma or superficial lacerations without thoracic or systemic involvement [2-4]. Scapular fractures account for less than 1% of all fractures and usually occur following high-energy trauma [5]. Most are extra-articular and are treated conservatively. Subcutaneous emphysema is not a recognized complication of scapular fractures; however, when associated with open wounds in the axillary or shoulder region, air may track along fascial planes into the upper limb. We present a rare case of post-traumatic subcutaneous emphysema of the upper extremity associated with an open scapular body fracture following blunt trauma. We also review the existing literature and discuss key diagnostic considerations to differentiate benign emphysema from limb-threatening infections.
A 65-year-old male presented to the emergency department after sustaining a fall from a two-wheeler, landing on his right side. He complained of pain and swelling in the right upper limb, along with a crackling sensation under the skin. There was no associated chest pain, dyspnea, or systemic complaints such as fever or malaise. He had no known comorbidities and no history of immunosuppressive conditions. On general examination, the patient was hemodynamically stable, afebrile, and oriented. Local examination revealed a 3 × 1 cm laceration over the posterior axillary fold on the right side (Fig. 1a). The surrounding skin was erythematous and mildly warm to the touch. Diffuse soft tissue swelling was present, extending from the axilla to the elbow (Fig. 1b). Palpation elicited crepitus throughout the upper arm, suggestive of SE. There was no active discharge or signs of gross contamination. Active and passive movements of the shoulder were restricted due to pain.
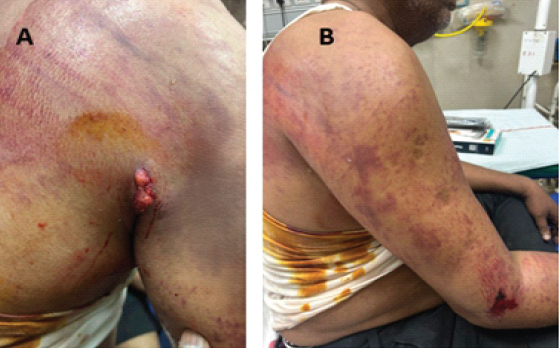
Figure 1: (a) Clinical image showing an open laceration over the axillary region with surrounding ecchymosis and swelling. (b) Extensive bruising and swelling of the upper limb extending from the shoulder to the elbow, consistent with underlying soft tissue trauma and subcutaneous emphysema.
The right upper limb was neurovascularly intact distally. Peripheral pulses (radial, ulnar, and brachial) were palpable and equal to the contralateral limb. Sensory and motor functions were preserved. There were no signs of compartment syndrome or systemic sepsis.
Investigations
Anteroposterior and lateral radiographs of the right shoulder and elbow showed linear radiolucent streaks within the soft tissues, consistent with SE (Fig. 2). An extra-articular fracture of the scapular body was also noted. A chest radiograph revealed no evidence of pneumothorax, hemothorax, rib fractures, or mediastinal shift.
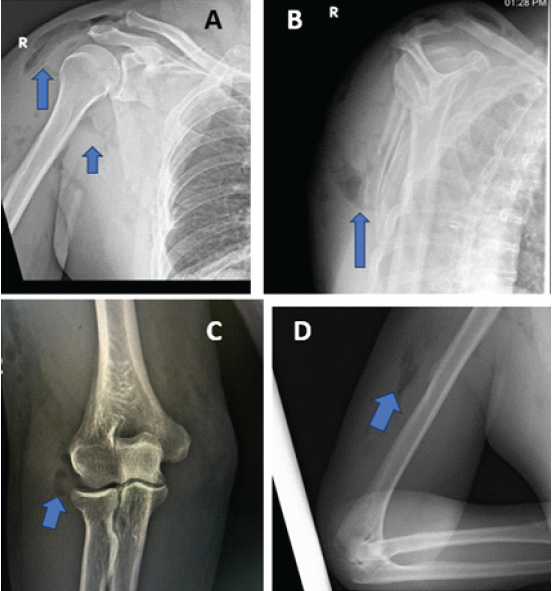
Figure 2: Plain radiographs of the right upper limb. (a) Anteroposterior (AP) view of the shoulder showing air lucencies in the soft tissue planes around the scapula and proximal arm (blue arrows), suggestive of subcutaneous emphysema. (b) Scapular Y-view demonstrating subcutaneous air in the axillary region (blue arrow). (c) AP view of the elbow showing air shadows in the subcutaneous tissue overlying the distal humerus (blue arrow). (d) Lateral view of the elbow confirming subcutaneous emphysema in the posterior soft tissue planes (blue arrow).
To evaluate the full extent of soft tissue air and rule out deeper involvement, a contrast-enhanced computed tomography (CT) scan of the thorax and shoulder was performed. It confirmed the presence of SE confined to the soft tissues of the axilla and upper arm (Fig. 3). There was no extension into the pleural cavity, no pneumomediastinum, and no vascular or pulmonary parenchymal injuries. The scapular body fracture was confirmed to be minimally displaced and extra-articular.
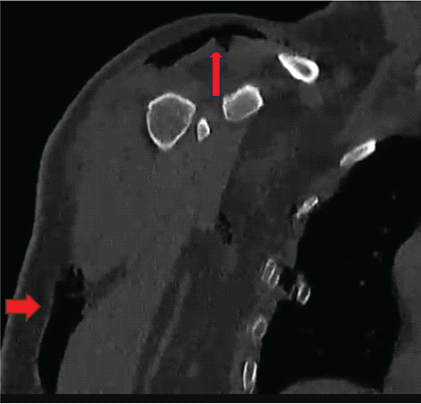
Figure 3: Coronal computed tomography image of the chest and left upper extremity. The red arrows highlight extensive subcutaneous air in the soft tissue planes of the upper limb (horizontal arrow) and axillary region (vertical arrow), consistent with subcutaneous emphysema.
Baseline laboratory investigations were within normal limits, including complete blood count, erythrocyte sedimentation rate, C-reactive protein, and serum lactate. A wound swab for culture and sensitivity, collected intraoperatively, showed no growth.
Management
The patient was taken for emergency surgical debridement. The laceration was irrigated thoroughly with saline, and no foreign body, devitalized tissue, or communication with deeper structures was identified. The wound was closed primarily over a closed suction drain. Empirical broad-spectrum intravenous antibiotics (piperacillin–tazobactam and clindamycin) were initiated and continued postoperatively. The antibiotics were later rationalized based on negative culture results. Analgesics and limb elevation were advised. The scapular body fracture was managed conservatively using an arm sling for immobilization, with instructions to avoid active shoulder movements in the early healing phase. The patient was closely monitored for signs of wound infection, systemic toxicity, or progression of emphysema. Daily clinical assessments over the first 48 h showed stable findings with no clinical deterioration.
Outcome and follow-up
By post-operative day 3, the erythema had subsided, the drain output was minimal, and the drain was removed. The wound remained clean and dry, with no signs of infection or recurrence of emphysema. At a 3-week follow-up, the wound had healed completely with no residual crepitus or swelling. There were no complications observed during the recovery period. At 1-year follow-up, the patient was asymptomatic and had regained full functional use of the affected upper limb. Functional assessment demonstrated a Constant–Murley score of 92; disabilities of the arm, shoulder, and hand score of 6; and American Shoulder and Elbow Surgeons score of 94, consistent with excellent functional outcome.
Subcutaneous emphysema (SE) of the limb is an uncommon but often benign clinical entity, most frequently resulting from penetrating injuries, high-pressure injection mechanisms, or minor lacerations [1-3,6]. In rare circumstances, SE may occur following blunt trauma with associated fractures, including scapular fractures, as demonstrated in the present case [4]. Despite its typically benign course, the presence of air within soft tissue planes can raise concern for life-threatening infections such as necrotizing fasciitis or clostridial myonecrosis, necessitating careful diagnostic evaluation [1,6]. In our patient, extensive SE developed after a two-wheeler accident in association with an extra-articular scapular body fracture and a posterior axillary laceration. The absence of systemic toxicity, normal inflammatory markers, lack of skin necrosis, and stability of the emphysema on serial examinations supported a benign traumatic etiology rather than an infectious process [2,3,15,16]. Similar presentations have been reported in the literature, where conservative management resulted in complete resolution without complications [Table 1].
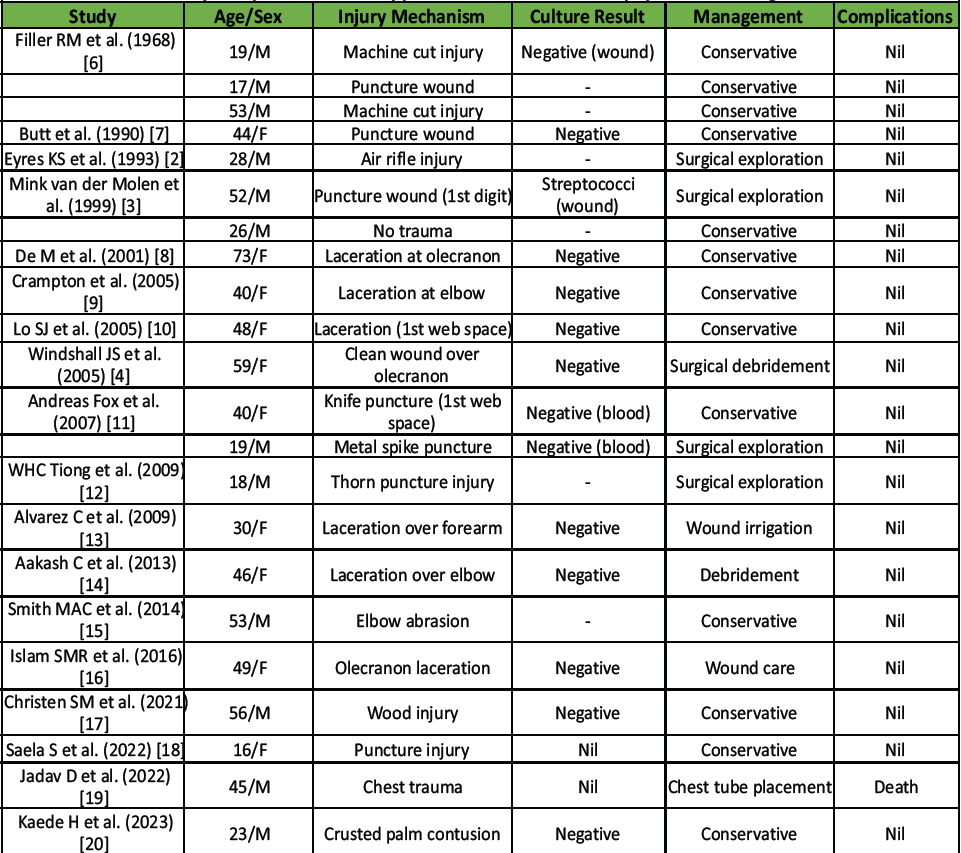
Table 1: Summary of reported cases of upper -limb subcutaneous emphysema following minor trauma
Diagnostic Considerations and Differential Diagnosis
The combination of crepitus, erythema, and swelling following trauma mandates exclusion of necrotizing soft tissue infections, which are associated with rapid progression, severe pain disproportionate to clinical findings, and systemic deterioration [1,6]. In contrast, benign traumatic SE is characterized by stable clinical findings, minimal pain progression, and absence of systemic signs [2,6,15]. These distinguishing features were clearly evident in our patient. Plain radiographs are useful for initial identification of subcutaneous air; however, computed tomography is the imaging modality of choice to delineate the extent of emphysema and to exclude deep fascial involvement, vascular injury, or thoracic communication [1,18]. In the present case, CT imaging confirmed that air was confined to the subcutaneous compartment, supporting conservative management.
Mechanism and Anatomical Considerations
The axilla represents an anatomical conduit through which air can easily track along fascial planes into the upper limb [1]. Superficial lacerations in this region, particularly when associated with underlying fractures and soft tissue disruption, may facilitate the ingress and spread of air during limb movement or pressure changes [5,18]. This mechanism likely explains the extensive distribution of SE observed in our patient.
Review of the Literature and Management Strategy
Published reports indicate that the majority of cases of traumatic upper limb SE are managed non-operatively, with surgical intervention reserved for diagnostic uncertainty, retained foreign bodies, or concern for infection [Table 1]. Our literature review corroborates these findings, demonstrating favorable outcomes with conservative treatment in most cases. Based on this evidence and our clinical experience, a structured diagnostic and management algorithm may assist clinicians in safely managing similar presentations [Fig. 4].
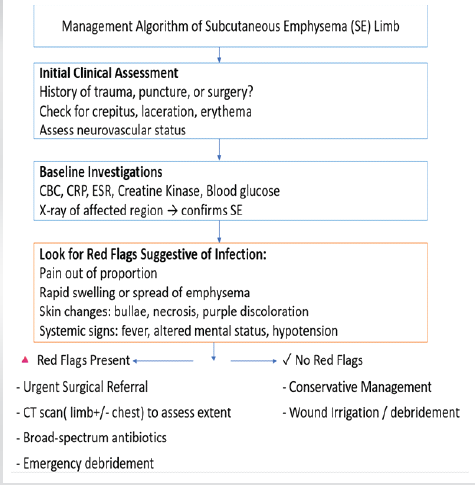
Figure 4: Simplified management algorithm for evaluating subcutaneous emphysema of the limb.
Limitations
This report is limited by its single-patient design, which precludes broad generalization of the findings. Nevertheless, case reports play a crucial role in highlighting rare clinical presentations and potential diagnostic pitfalls. By integrating our experience with a review of the available literature, this report aims to increase awareness of benign post-traumatic SE of the upper limb and provide a practical diagnostic framework for clinicians. Furthermore, the inability to directly confirm the mechanism represents a limitation of this case report.
SE of the upper limb following minor trauma or superficial laceration is rare but generally benign. Conservative management is effective in most cases, while surgical intervention is reserved for diagnostic clarification or wound care. This case adds to the limited literature and reinforces that isolated scapular fractures with overlying soft tissue injury can result in benign emphysema without systemic implications.
Post-traumatic SE of the upper limb, even when extensive, can be benign in the context of minor lacerations and isolated scapular fractures. Careful clinical assessment, early imaging (radiographs and CT), and close monitoring are essential to differentiate it from limb-threatening infections such as necrotizing fasciitis. Awareness of this rare presentation helps avoid unnecessary aggressive surgical intervention, while targeted conservative management with wound care and antibiotics ensures safe and effective recovery.
References
- 1. Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema: pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144(7):1447–1453. [Google Scholar] [PubMed]
- 2. Eyres KS, Bruce CE. Surgical emphysema of the hand following air rifle injury. J Accid Emerg Med. 1993;10(3):209. [Google Scholar] [PubMed]
- 3. Mink van der Molen AB, Smeets MJ, van Ginkel RJ. Surgical emphysema of the hand after minor trauma. J Hand Surg Br. 1999;24(3):369–370. [Google Scholar] [PubMed]
- 4. Winshall J.S., Weissman B.N. Images in clinical medicine. Benign subcutaneous emphysema of the upper extremity. N. Engl. J. Med. 2005;352:1357. doi: 10.1056/NEJMicm040914. [Google Scholar] [PubMed] [CrossRef]
- 5. Cole PA, Gauger EM, Herrera DA, Anavian J. Scapula fractures. Curr Rev Musculoskelet Med. 2013;6(1):79–87. [Google Scholar] [PubMed]
- 6. Filler RM, Griscom NT, Pappas A (1968) Post-traumatic crepitation falsely suggesting gas gangrene. N Engl J Med 278: 758-761. [Google Scholar] [PubMed]
- 7. Butt M, Hird G F. Surgical emphysema of the dorsum of the hand. J Hand Surg 199015B379–380. [Google Scholar] [PubMed]
- 8. De M, Stevenson J. Subcutaneous emphysema of upper limb. Emerg Med J. 2001 Nov;18(6):522. doi: 10.1136/emj.18.6.522. PMID: 11696529; PMCID: PMC1725699. [Google Scholar] [PubMed] [CrossRef]
- 9. Crampton JA. An unusual case of surgical emphysema. Injury Extra. 2005;36:225–7. doi: 10.1016/j.injury.2004.10.032. [Google Scholar] [PubMed] [CrossRef]
- 10. LO SJ, HUGHES J, ARMSTRONG A. Non-Infective Subcutaneous Emphysema of the Hand Secondary to a Minor Webspace Injury. Journal of Hand Surgery. 2005;30(5):482-483. doi:10.1016/j.jhsb.2005.04.020 [Google Scholar] [PubMed] [CrossRef]
- 11. Fox A, Sheick H, Ekwobi C, et al. (2007) Benign surgical emphysema of the hand and upper limb: gas is not always gangrene-a report of two cases. Emerg Med J 24: 798-799. [Google Scholar] [PubMed]
- 12. Tiong WH, Butt FS.. Subcutaneous emphysema of the upper extremity following penetrating blackthorn injury to the wrist. J Plast Reconstr Aesthet Surg. 2009;62(2):e29–e32. Feb [Google Scholar] [PubMed]
- 13. Clavijo-Alvarez JA, Stofman G. Noninfectious subcutaneous emphysema of the upper extremity. Plast Reconstr Surg. 2009 Apr;123(4):154e-155e. doi: 10.1097/PRS.0b013e31819e5c2a. PMID: 19337074. [Google Scholar] [PubMed] [CrossRef]
- 14. Aakash C., Brabender C., Mistovich R.J., Demeo P.J., Palmer B.A. An unusual cause for noninfectious subcutaneous emphysema of the upper extremity: a case report. JBJS Case Connect. 2013;3:e135. doi: 10.2106/JBJS.CC.M.00161. [Google Scholar] [PubMed] [CrossRef]
- 15. Clayton-Smith MA, Sivathasan N. A case of benign subcutaneous emphysema. BMJ Case Rep. 2014 Feb 13;2014:bcr2013202261. doi: 10.1136/bcr-2013-202261. PMID: 24526199; PMCID: PMC3926492. [Google Scholar] [PubMed] [CrossRef]
- 16. Rabiul Islam SM, Mamman KG, Pande KC. Benign Subcutaneous Emphysema of the Upper Limb: A Case Report. Malays Orthop J. 2016 Nov;10(3):39-41. doi: 10.5704/MOJ.1611.002. PMID: 28553447; PMCID: PMC5333683. [Google Scholar] [PubMed] [CrossRef]
- 17. Christen SM, Gruenert JG, Winsauer S. Benign subcutaneous emphysema: a rare and challenging entity a case report and review of the literature. Case Reports Plast Surg Hand Surg. 2021 Oct 1;8(1):153-157. doi: 10.1080/23320885.2021.1984922. PMID: 34621914; PMCID: PMC8491730. [Google Scholar] [PubMed] [CrossRef]
- 18. Saela S, Decilveo A, Isaac R, Patel DV. Traumatic subcutaneous emphysema of the hand/forearm: A case report. Chin J Traumatol. 2022 Nov;25(6):395-399. doi: 10.1016/j.cjtee.2022.04.001. Epub 2022 Apr 4. PMID: 35450804; PMCID: PMC9751530. [Google Scholar] [PubMed] [CrossRef]
- 19. Jadav D, Meshram VP. Unusual subcutaneous emphysema extending to the limbs following blunt chest injury. J Forensic Sci. 2022 Sep;67(5):2106-2109. doi: 10.1111/1556-4029.15078. Epub 2022 Jun 14. PMID: 35699108. [Google Scholar] [PubMed] [CrossRef]
- 20. Hiruma K, Suzuki K, Kato A, Yamaga H, Nakamura M, Inoue G, Kaki Y, Miyamoto K, Yagi M, Dohi K. Benign noninfectious subcutaneous emphysema with minor injury: A case report. Heliyon. 2022 Dec 23;9(1):e12317. doi: 10.1016/j.heliyon.2022.e12317. PMID: 36691541; PMCID: PMC9860412. [Google Scholar] [PubMed] [CrossRef]