Post-operative pseudomeningocele should be considered a potential cause of neurological symptoms in patients with a history of spinal surgery involving dural repair, even when the onset is delayed.
Dr. Ryunosuke Fukushi, Department of Orthopaedic Surgery, Sapporo Medical University School of Medicine, S1 W16, Sapporo, Hokkaido, 060-8543, Japan. E-mail: ryunosuke_fukushi_521@yahoo.co.jp
Introduction: Pseudomeningocele is a recognized post-operative complication of spinal surgery; however, most patients remain asymptomatic, and neurological manifestations are rare. Consequently, reports providing detailed intraoperative findings are limited. Here, we report a rare case of post-operative pseudomeningocele presenting with neurological symptoms >1 year after the initial surgery.
Case Report: A 53-year-old male with thoracolumbar ossification of the ligamentum flavum (OLF) at the T1/2 and L2/3/4 levels underwent T1 laminectomy and L2–4 laminoplasty. Intraoperatively, a dural tear occurred at the lumbar level and was primarily repaired. One year later, the patient developed acute lower back pain, left lower limb pain, and progressive weakness while performing household cleaning in a forward-flexed posture. Pre-operative imaging suggested L3/4 disc herniation and residual OLF at the same level, and surgical treatment (microscopic discectomy and laminoplasty) was planned. After drilling the left facet joint for discectomy, a sac-like structure, which was continuous with the dura mater, migrated posteriorly. This structure was diagnosed as a pseudomeningocele, rather than a disc herniation. No cerebrospinal fluid leakage or dural injury was observed. Adequate decompression was performed without manipulating the pseudomeningocele. The patient’s symptoms resolved postoperatively with no recurrence at the 6-month follow-up.
Conclusion: This case demonstrates that a pseudomeningocele, although typically asymptomatic, can cause delayed neurological symptoms >1 year after dural repair. Clinicians should consider post-operative pseudomeningocele as a differential diagnosis in patients with new neurological deficits after spinal surgery.
Keywords: Pseudomeningocele, dural repair, spinal surgery.
A pseudomeningocele is an extradural collection of cerebrospinal fluid (CSF) resulting from a dural defect and may occur as a complication of spinal surgery. Although iatrogenic dural injury is a known intraoperative complication, it is infrequent. Most patients with post-operative pseudomeningoceles remain asymptomatic, and delayed neurological deficits are exceedingly rare. Furthermore, few studies have reported detailed intraoperative findings or discussed the potential mechanisms underlying delayed clinical manifestations. Here, we present the rare case of a patient with pseudomeningocele who developed neurological symptoms 1 year after dural repair and was initially diagnosed with recurrent lumbar disc herniation.
Patient information and initial surgery
A 53-year-old male diagnosed with thoracolumbar ossification of the ligamentum flavum (OLF) at T1/2 and L2/3/4 underwent T1 laminectomy and L2–4 laminoplasty (Fig. 1). During lumbar surgery, an iatrogenic dural injury occurred at the lumbar level and was repaired. The patient’s post-operative recovery was uneventful, and all pre-operative symptoms resolved.
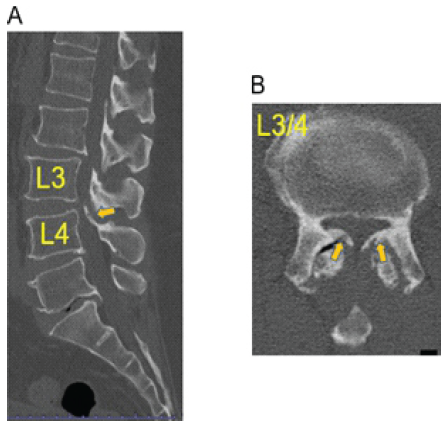
Figure 1: Computed tomography images before the initial surgery. (a) Sagittal view (b) Axial view at the L3–4 level.
Symptom onset
At post-operative 1 year, the patient experienced a sudden onset of acute lower back pain, left lower limb pain, and progressive weakness while performing household cleaning in a forward-flexed posture. The symptoms gradually worsened, leading to repeated falls and gait difficulty, and the patient was referred to a local orthopedic surgeon for further evaluation.
Physical examination and imaging findings
Neurological examination revealed mild weakness in the left quadriceps (manual muscle testing score 4/5), decreased left patellar reflex, bilateral Achilles hyperreflexia, diminished pain and temperature sensation in the left thigh and distal leg, and numbness around the lateral thigh and knee. The straight leg raise test result was positive on the left side (Fig. 2). The Visual Analog Scale (VAS) before surgery demonstrated low back pain of 45/100 and leg pain of 75/100. Computed tomography revealed residual OLF at L3/4. Magnetic resonance imaging (MRI) revealed adequate decompression at L2/3 but canal narrowing at L3/4 due to disc bulging. Based on these findings, the patient was diagnosed with left L3/4 disc herniation with insufficient decompression owing to residual OLF, and microscopic discectomy with extended laminoplasty was planned (Fig. 3).
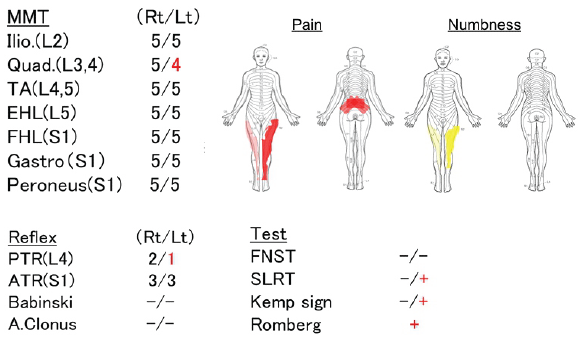
Figure 2: Physical examination findings on presentation to our institution.
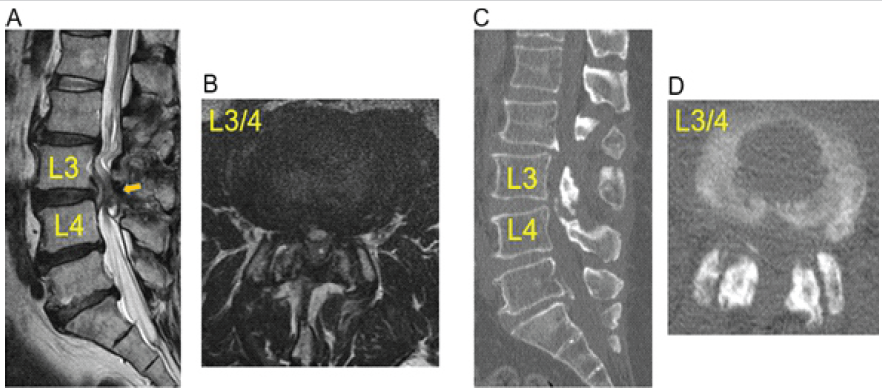
Figure 3: Pre-operative imaging before the revision surgery. (a) Sagittal MRI view. (b) Axial MRI view at the L3–4 level. (c) Sagittal CT view. (d) Axial CT view at the L3–4 level. CT: Computed tomography, MRI: Magnetic resonance imaging.
Intraoperative findings
Re-exploration of the prior surgical site allowed removal of the residual OLF at L3/4. During drilling of the left facet joint to access the presumed disc herniation, a sac-like structure that was continuous with the dura mater shifted posteriorly. Accordingly, the patient was diagnosed with a pseudomeningocele and not a disc herniation as initially suspected. No active CSF leakage or new dural tears were observed. Motor-evoked potentials remained stable throughout surgery. Decompression was completed without manipulating the pseudomeningocele, which was left intact (Fig. 4).
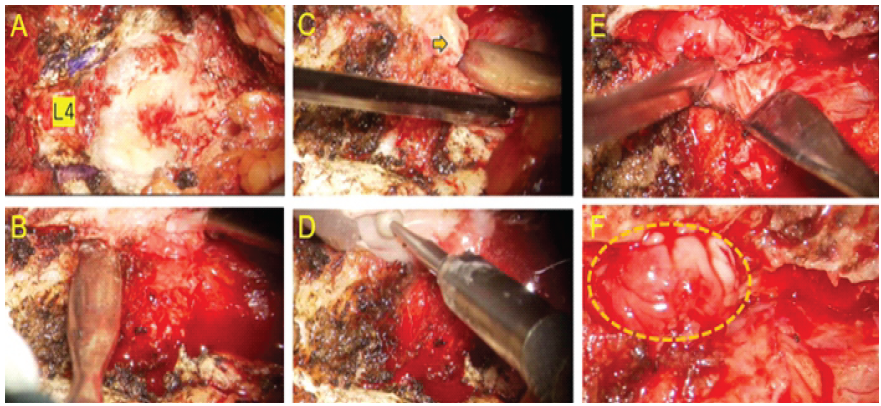
Figure 4: Intraoperative findings during revision surgery. (a) Exposure of the surgical field. (b and c) Residual ossified ligamentum flavum. (d) Removal of the residual ossified ligamentum flavum using an air drill. (e) Retraction of the dura to approach the intervertebral disc. (f) Pseudomeningocele identified intraoperatively (dotted area).
Post-operative course
The patient’s back and leg pain resolved immediately after surgery, with both VAS scores improving to 0/100. In addition, the gait was normalized, and no recurrence of neurological symptoms was observed at the 6-month follow-up.
Pseudomeningocele after spinal surgery is often under-recognized, particularly when symptoms arise after a prolonged post-operative interval. The present case is notable because neurological symptoms manifested 1 year after the initial procedure, and a pseudomeningocele without evidence of an active CSF leak was identified intraoperatively. Most post-operative pseudomeningoceles originate from iatrogenic dural injuries recognized during surgery or from unrecognized microdefects. Persistent CSF leakage through a small dural defect may create a “ball-valve” mechanism, allowing gradual accumulation of CSF in the extradural space [1,2,3]. Over time, fibroblast-mediated collagen deposition results in the formation of a fibrous capsule that expands or shifts dynamically with changes in pressure, eventually producing neurological symptoms. In addition, certain anti-adhesion agents or sealants used during dural repair may delay wound healing or impair fibroblast migration, potentially contributing to pseudomeningocele formation [3]. These mechanisms may explain why some patients develop symptoms despite the absence of a persistent CSF fistula. Previous reports have documented symptomatic pseudomeningoceles presenting at variable intervals. Oterdoom et al. described cauda equina entrapment within a pseudomeningocele following schwannoma excision [4]. Foo et al. reported acute neurological deterioration due to a thoracic pseudomeningocele 1 week postoperatively [5]. Nold et al. reported a delayed cervical pseudomeningocele appearing decades after trauma [6]. Rahimizadeh and Javadi described a lumbosacral symptomatic pseudomeningocele related to root avulsion injury [7]. These cases highlight that pseudomeningoceles may mimic other spinal pathologies and present after prolonged asymptomatic periods, as observed in the present case. This report highlights several important clinical considerations. First, pseudomeningocele should be considered in the differential diagnosis of new neurological symptoms after spinal surgery, regardless of the interval since the initial procedure. MRI, particularly T2-weighted sequences, is valuable for identifying extradural CSF collections and determining their continuity with the dura [8,9,10]. Second, pseudomeningoceles do not necessarily require direct surgical repair, especially when the absence of an active CSF leak and the adequacy of decompression can be confirmed intraoperatively [1,3]. Avoiding unnecessary manipulation of the dura may help reduce surgical risk. Third, meticulous dural closure during the initial surgery remains essential, and reinforcement techniques may be beneficial when the dural defect is large or when the risk of persistent leakage is high [2,3]. This study has several limitations. Pre-operative imaging was not specifically optimized to evaluate pseudomeningocele, limiting insights into its evolution. In addition, follow-up beyond 6 months was unavailable, preventing assessment of potential late recurrence. Finally, the precise mechanism underlying the delayed onset of symptoms remains unclear. Future research should include prospective documentation of post-operative pseudomeningoceles with serial imaging, evaluations of CSF pressure dynamics, and studies on repair materials or techniques that may improve dural healing.
Pseudomeningoceles after dural repair can present with delayed neurological symptoms. Clinicians should consider this condition when evaluating post-operative neurological decline.
A pseudomeningocele is an important differential diagnosis in patients with new or delayed-onset neurological symptoms after successful repair of intraoperative dural injury with an uneventful post-operative course. Recognizing this possibility helps prevent misdiagnosis and guides appropriate evaluation and surgical decision-making.
References
- 1. Shu W, Wang H, Zhu H, Li Y, Zhang J, Lu G, et al. Nerve root entrapment with pseudomeningocele after percutaneous endoscopic lumbar discectomy: A case report. J Spinal Cord Med 2020;43:552-5. [Google Scholar] [PubMed]
- 2. Couture D, Branch CL Jr. Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus 2003;15:E6. [Google Scholar] [PubMed]
- 3. Solomon P, Sekharappa V, Krishnan V, David KS. Spontaneous resolution of postoperative lumbar pseudomeningoceles: A report of four cases. Indian J Orthop 2013;47:417-21. [Google Scholar] [PubMed]
- 4. Oterdoom DL, Groen RJ, Coppes MH. Cauda equina entrapment in a pseudomeningocele after lumbar schwannoma extirpation. Eur Spine J 2009;19 Suppl 2:S158-61. [Google Scholar] [PubMed]
- 5. Foo CH, Hii BY, Wong CC, Ohn KM. Acute neurological deficit caused by thoracic pseudomeningocele after spinal surgery. BMJ Case Rep 2021;14:e243788. [Google Scholar] [PubMed]
- 6. Nold TM, Mansour TR, Telemi E, Tahir RA, Abdulhak MW. Delayed presentation of a ventral cervical pseudomeningocele resulting in intracranial hypotension and extremity paresis. ACS Case Rev Surg 2025;5:5-9. [Google Scholar] [PubMed]
- 7. Rahimizadeh A, Javadi SA. Symptomatic intraspinal lumbosacral pseudomeningocele, a late consequence of root avulsion injury secondary to a gunshot wound. N Am Spine Soc J 2020;3:100025. [Google Scholar] [PubMed]
- 8. Sklar EM, Quencer RM, Green BA. Posttraumatic spinal pseudomeningocele: MR and clinical features. AJNR Am J Neuroradiol 1990;11:1184. [Google Scholar] [PubMed]
- 9. Beckman SP, Proctor C, Toms JB. The management of recurrent post-myelography lumbar pseudomeningocele with epidural blood patch. Cureus 2023;15:e35600. [Google Scholar] [PubMed]
- 10. Yokoyama K, Yamada M, Tanaka H, Ito Y, Sugie A, Wanibuchi M, et al. A case of dural herniation of the cauda equina caused by enlarged spinal subdural extra-arachnoid hygroma following lumbar microsurgical decompression: Case report. NMC Case Rep J 2021;8:261-5. [Google Scholar] [PubMed]