A single-stage biplanar tibial tuberosity osteotomy augmented with tricortical iliac crest bone grafting and dual-pillar fixation provides a reliable and reproducible method for correcting complex genu recurvatum with anterior tibial subluxation, offering stable alignment, preservation of patellar height, rapid bone healing, and early functional recovery in young active patients.
Dr. A S Hemapriya, Independent Researcher, 42, MR Blossom Apartments, 1st Main Road, 2nd Cross Street, Srinivasapuram, Korattur, Chennai, Tamil Nadu, India. E-mail: hemapriyasekhar@gmail.com
Introduction: Genu recurvatum with anterior tibial subluxation is an uncommon but functionally debilitating deformity that can cause progressive pain, instability, and altered gait mechanics in young adults. When conservative management fails, surgical correction becomes necessary to restore alignment, joint biomechanics, and functional capacity. This report describes a reproducible single-stage corrective technique for complex genu recurvatum using biplanar osteotomy, bone graft augmentation, and dual-pillar fixation.
Case Report: A 19-year-old male presented with a 3-month history of progressive left knee pain, exacerbated by walking and stair climbing. Clinical examination revealed valgus alignment with hyperextension, and radiographs confirmed complex genu recurvatum with anterior tibial subluxation. Laboratory and serological investigations were within normal limits. The patient underwent a single-stage surgical procedure consisting of an 8 mm biplanar tibial tuberosity osteotomy performed distal to the patellar tendon, augmentation with a tricortical iliac crest bone graft, and dual-pillar fixation using medial and lateral plates along with tibial tuberosity screw fixation under C-arm guidance. The post-operative course was uneventful. At 2 months, he demonstrated 0–100° of knee flexion with significant pain reduction. By 5 months, he achieved a full range of motion, complete pain relief, and radiological signs of progressive bone union. At 9 months, he showed stable alignment, full functional recovery, and returned to sports without pain or limitations.
Conclusion: This case highlights the effectiveness of a combined biplanar osteotomy with bone grafting and dual-pillar fixation for treating complex genu recurvatum with anterior tibial subluxation. The technique offers durable correction, maintains patellar height, promotes rapid healing, and supports early return to full functional activities.
Keywords: Genu recurvatum, tibial plateau subluxation, bone grafting, tricortical, orthopedic fixation devices, knee joint stability.
Genu recurvatum, characterized by knee hyperextension exceeding 5–15°, is a relatively uncommon deformity that can lead to significant functional impairment and anterior knee pain due to altered joint loading and soft tissue imbalance [1]. Complex recurvatum deformities often involve anterior subluxation of the tibia, further exacerbating patellofemoral maltracking and joint overloading [2]. Surgical correction aims to restore normal sagittal alignment, preserve patellar height, and reestablish stable patellofemoral mechanics [3]. Proximal tibial osteotomy techniques, including opening-wedge, closing-wedge, and biplanar approaches, have been described to address these issues [4]. The biplanar osteotomy distal to the tibial tuberosity allows multiplanar correction while maintaining the patellar tendon attachment, thus preserving patellofemoral mechanics and preventing patella baja [2]. Tricortical iliac crest bone graft augmentation enhances structural stability and promotes early osteotomy site healing [5]. Despite various techniques, there remains no consensus on the optimal method for managing complex genu recurvatum with anterior subluxation. This case report describes a single-stage approach combining an 8 mm biplanar tibial tuberosity osteotomy, tricortical iliac crest graft augmentation, and dual-pillar plating, resulting in sustained deformity correction, pain relief, and full functional recovery.
A 19-year-old male patient presented to the Asian Orthopaedic Institute at SRM Institute of Medical Sciences, Chennai, Tamil Nadu, India, with a 3-month history of progressive left knee pain and functional limitation. The patient reported an insidious onset of pain that was moderate in intensity, aggravated by walking and climbing stairs, and relieved by rest and medications. The symptoms significantly limited his daily activities, prompting surgical consultation.
Clinical findings
Physical examination revealed a left knee valgus deformity with hyperextension positioning. The knee demonstrated active toe and ankle movements with palpable distal pulses. Vital signs were within normal limits (pulse: 86/min, BP: 120/80 mmHg, temperature: 97.6°F, respiratory rate: 20/min). Systemic examination was unremarkable with normal cardiovascular, respiratory, abdominal, and neurological findings.

Figure 1: Clinical photographs showing the patient’s knee alignment and deformity before surgery. (a) Anterior view demonstrating valgus alignment with hyperextension; (b) Lateral view showing knee hyperextension (recurvatum deformity); (c) Posterior view illustrating leg alignment and calf contour; (d) Oblique lateral view highlighting knee posture and recurvatum.
Fig. 1 shows the clinical photographs demonstrating the patient’s knee deformity, including valgus alignment, hyperextension, and abnormal posture in anterior, lateral, posterior, and oblique views.
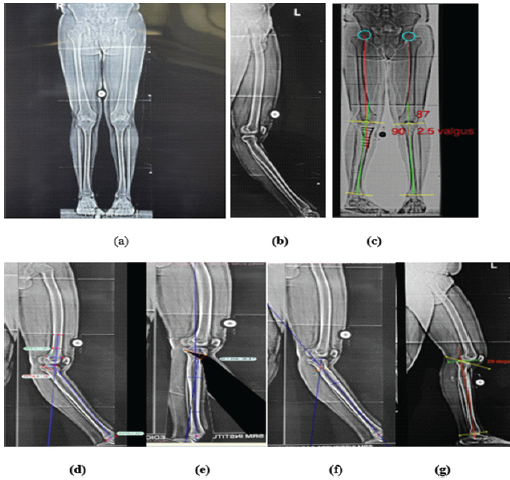
Figure 2: Radiological images demonstrating the preoperative deformity and postoperative correction. (a) Full-length lower-limb anteroposterior (AP) view; (b) Lateral view of left lower limb; (c) Full-length lower-limb AP view with mechanical axis and angle measurements; (d) Lateral view of left lower limb with angle measurements; (e) Left knee lateral view with alignment lines; (f) Left knee extended lateral view with axis lines; (g) Left knee lateral view showing flexion angle (20°).
Fig. 2 presents the radiological images illustrating the preoperative deformity with mechanical axis deviation and postoperative correction on both anteroposterior (AP) and lateral views. Together, these figures depict the clinical appearance and radiological confirmation of the deformity and its correction.
Diagnostic assessment
Laboratory investigations showed normal hematological parameters (hemoglobin: 14.5–12.0 g/dL, white blood cell: 9180/μL, platelets: 255,000/μL), renal function (creatinine: 0.70 mg/dL, blood urea: 17 mg/dL), and coagulation profile (prothrombin time: 13.9 s, international normalized ratio: 1.00). Serological markers were negative for hepatitis B, human immunodeficiency virus, and hepatitis C. Inflammatory markers showed minimal elevation (erythrocyte sedimentation rate: 02 mm/h, C-reactive protein: 1.44 mg/L). Radiological evaluation confirmed the diagnosis of left knee complex recurvatum deformity with anterior knee subluxation and anterior knee joint overloading pain. The imaging demonstrated significant hyperextension deformity with anterior displacement of the tibial component relative to the femur.
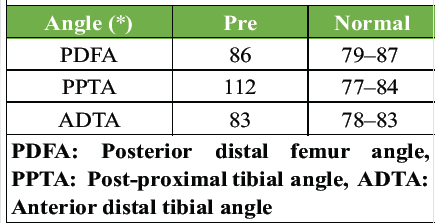
Table 1: Lateral scanogram lower-limb chart with normal reference value
In Table 1, using TRAUMACAD SOFTWARE, angle lines are drawn pre-operative in the AP lower-limb scanogram medial proximal tibial angle (90) and lateral distal femur angle (87) which are in the physiological range, whereas the lateral lower-limb scanogram measurement shows posterior distal femur angle (PDFA – 86°), post proximal tibial angle is 112° (PPTA – 112°), and anterior distal tibial angle is 83° (ADTA – 83°). These angles and measurements show that deformity is in the proximal tibia, recurvatum deformity with center of rotation of angulation (CORA) at the level of the proximal tibia.
Based on the clinical and radiological findings, a comprehensive surgical approach was planned to correct deformity at the level of CORA, following the steps planned.
- Left knee complex anterior midline skin flap exposure
- Anterior patella tuberosity biplanar osteotomy, tibia osteotomy, anterior open wedge, keeping the posterior tibia as the hinge point at the level of CORA
- Tricortical iliac bone graft augmentation 2.5 cm (graft length was calculated prior with software)
- Stabilization with medial and lateral pillar plating
- Tibial tuberosity fixation with screws
- Complex anterior flap /skin closure.
Surgical procedure
Preoperative preparation
The patient underwent pre-operative anesthesia fitness evaluation and internal medicine consultation. All investigations were within normal limits, confirming surgical candidacy. Informed consent was obtained detailing the surgical procedure, risks, benefits, and expected outcomes.
Operative technique
Patient positioning and preparation
The patient was positioned supine under general anesthesia with C-arm fluoroscopy guidance. The left lower limb was prepared and draped in a sterile fashion.
Bone graft harvesting
A 2.5 cm skin incision was made over the left anterior superior iliac spine. Tricortical iliac bone graft was harvested using a standard technique. The harvest site was irrigated, closed in layers, and skin approximated with surgical staples.
Primary surgical approach
A long midline anterior skin incision was made over the left knee. Medial and lateral flaps were carefully elevated to expose the underlying structures while preserving neurovascular integrity.
Biplanar osteotomy technique
An 8 mm biplanar osteotomy of the tibial tuberosity was performed. The osteotomy was designed to maintain the tibial tuberosity attached to the patella tendon while allowing for anterior elevation. This technique prevents patella baja and maintains optimal patellofemoral mechanics.
Deformity correction
The osteotomy was extended from anterior to posterior planes. The harvested tricortical iliac bone graft was placed at the osteotomy site to maintain correction and promote healing. The recurvatum deformity was corrected to achieve normal knee alignment.
Stabilization
Multiple fixation methods were employed:
- Medial column stabilization using locking plate with two screws on either side of the osteotomy
- Lateral column stabilization using lateral locking plate with one screw on either side
- Tibial tuberosity fixation with four screws and washers to maintain position.
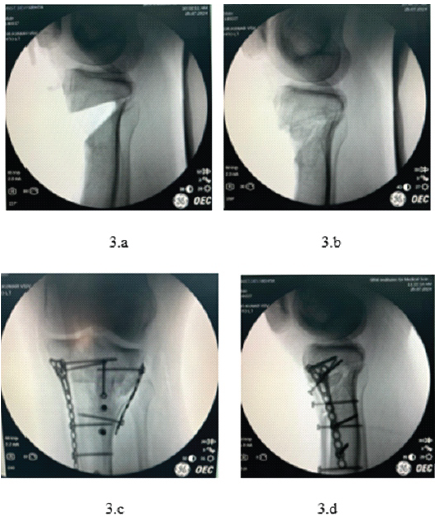
Figure 3: Intraoperative fluoroscopic images illustrating osteotomy and fixation stages. (a) Lateral view after completion of biplanar tibial tuberosity osteotomy, before graft placement and fixation; (b) Anteroposterior view after osteotomy, showing gap created for graft insertion; (c) Anteroposterior view following final implant fixation with tricortical graft in place; (d) Lateral view following dual-pillar plate fixation and tibial tuberosity screw placement.
Fig. 3 shows intraoperative fluoroscopic images demonstrating the osteotomy site (Fig. 3a and b) and the subsequent fixation with a locking plate and screws after deformity correction (Fig. 3c and d). These images illustrate the stepwise execution of the osteotomy and stabilization.
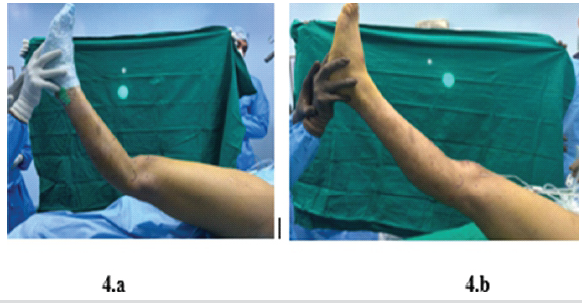
Figure 4: Intraoperative clinical images demonstrating correction of knee hyperextension. (a) Pre-correction positioning showing excessive knee hyperextension. (b) Post-correction positioning illustrating restored knee flexion and alignment.
Fig. 4 shows intraoperative clinical images demonstrating knee stability and range of motion after deformity correction. Fig. 4a depicts knee flexion, while Fig. 4b shows full knee extension following osteotomy and fixation.
Wound closure
The surgical site was thoroughly irrigated. Hemostasis was achieved, and the wound was closed in anatomical layers. Skin closure was performed using sutures and surgical staples.
Postoperative course
Immediate postoperative period
The patient’s immediate post-operative course was uneventful. Pain management was achieved with a combination of paracetamol (1 g 3 times daily), lornoxicam (8 mg twice daily), and pantoprazole (40 mg twice daily) for gastric protection. Prophylactic antibiotic coverage was provided with cefuroxime (500 mg twice daily) for 5 days.
Mobilization protocol
A structured physiotherapy program was initiated:
- Non-weight-bearing walking with walker support
- Active assisted knee range of motion limited to 30° for the 1st week
- Static quadriceps strengthening exercises
- Ankle pump exercises to prevent thromboembolism
- Ice pack application for pain and swelling control
- Knee brace application during ambulation for protection.
Follow-up and outcomes
Short-term follow-up (2 months post-surgery – September 2024)
At the 2-month follow-up visit in September 2024, the patient demonstrated excellent early surgical outcomes. Clinical examination revealed successful knee recurvatum deformity correction with good bone graft integration at the osteotomy site. The patient achieved 0–100° of knee flexion range of motion, indicating satisfactory functional recovery. Pain levels were significantly reduced compared to preoperative status, and the patient demonstrated good healing of both the surgical site and iliac crest bone graft harvest site.
Progressive weight-bearing mobilization was initiated with support, transitioning from the initial non-weight-bearing protocol. The structured physiotherapy program showed positive results with improved quadriceps strength and functional mobility.
Intermediate follow-up (5 months post-surgery – December 2024)
The 5-month follow-up assessment in December 2024 revealed continued improvement in clinical parameters. The patient reported being clinically and functionally well with no complaints of pain or functional limitation. Radiological evaluation demonstrated good progression in healing of the osteotomy site with evidence of bone union.
The knee demonstrated a full range of motion without any residual deformity or instability. The patient had successfully transitioned to full weight-bearing ambulation without assistive devices, indicating complete functional recovery. No complications such as hardware failure, infection, or loss of correction were observed.
Long-term follow-up (9-month post-surgery – April 2025)
At the 9-month follow-up in April 2025, the patient maintained excellent long-term outcomes. Clinical assessment showed sustained deformity correction with no recurrence of recurvatum or anterior subluxation. The patient demonstrated normal knee function with full range of motion and returned to regular activities including sport participation.
Radiological evaluation confirmed complete bone union at the osteotomy site with well-integrated tricortical iliac bone graft. The metallic implants remained in the appropriate position without any sign of loosening or migration. The tibial tuberosity fixation showed solid healing with restoration of normal patellofemoral mechanics.
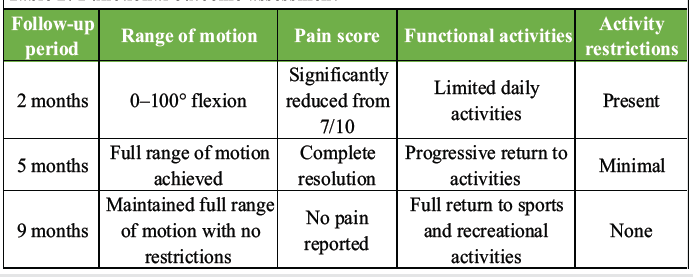
Table 2: Functional outcome assessment
In Table 2, throughout the follow-up period, the patient demonstrated progressive improvement in functional parameters, and the functional outcome assessment shows a clear pattern of steady recovery over time. At 2 months, the patient had limited shoulder mobility, significant pain, and noticeable restrictions in daily activities. By 5 months, the patient achieved a full range of motion with complete pain resolution and only minimal limitations, allowing a gradual return to routine activities. By 9 months, the patient maintained full mobility without pain, resumed sports and recreational activities, and demonstrated complete functional recovery with no activity restrictions.
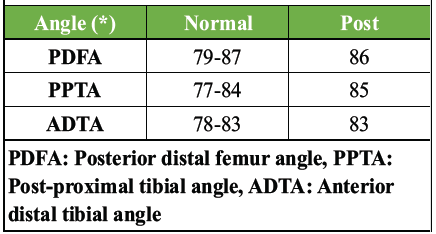
Table 3: Post angle correction using TRAUMACARD software
In Table 3, the post-angle correction values generated using the TRAUMACARD software indicate successful realignment of the proximal humerus. The PDFA improved to 86°, placing it well within the normal reference range (79–87°). The PPTA increased to 85°, slightly above the normal upper limit (77–84°), suggesting a marginal overcorrection but still within acceptable clinical limits. The ADTA measured 83°, aligning exactly with the upper boundary of the normal range (78–83°). Overall, these measurements demonstrate that post-operative alignment closely approximates normal anatomical parameters, indicating a satisfactory radiological outcome.
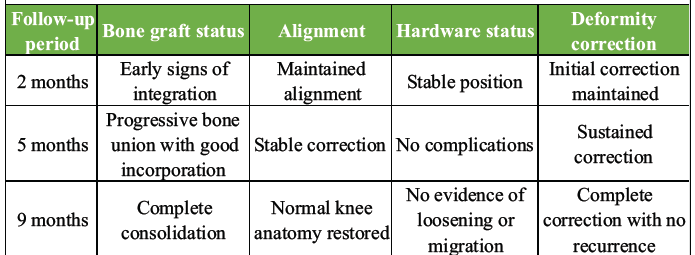
Table 4: Radiological assessment of healing and deformity correction over time
In Table 4, the radiological outcomes show consistent and progressive healing throughout the follow-up period. At 2 months, early graft integration, maintained alignment, and stable hardware indicate a good initial postoperative response. By 5 months, the bone graft demonstrates strong incorporation with stable alignment and no hardware complications, confirming sustained deformity correction. At 9 months, complete bone consolidation, restoration of normal anatomy, and the absence of hardware issues confirm a fully successful radiological outcome with no recurrence of deformity.
The correction of recurvatum deformity was maintained throughout the follow-up period with no evidence of loss of correction or hardware failure. The biplanar osteotomy technique successfully preserved patellofemoral mechanics while achieving the desired deformity correction.
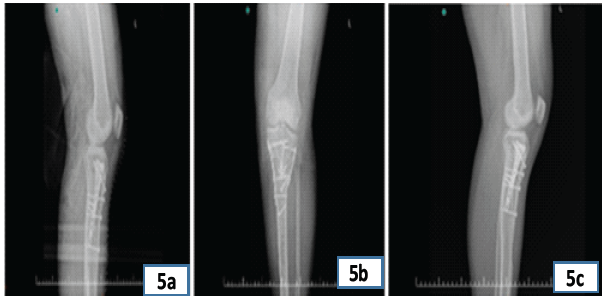
Figure 5: Postoperative radiographic images demonstrating implant position and bone healing. (a) Lateral radiograph showing fixed biplanar osteotomy with maintained alignment and implant stability; (b) Anteroposterior radiograph illustrating well-aligned knee joint and stable fixation with plates and screws; (c) Oblique radiograph highlighting bone graft incorporation and hardware position.
In Fig. 5, a retrograde intramedullary nail with interlocking screws is visible, stabilizing a femoral shaft fracture. The alignment appears maintained across all three views, showing satisfactory implant positioning.

Figure 6: Post-operative clinical photographs demonstrating functional outcomes at 5 months.
In Fig. 6, the fixation appears stable in both anteroposterior and lateral views, showing appropriate alignment. The lower photographs show the patient performing active knee and hip mobilization exercises as part of post-operative rehabilitation.
This case presents a comprehensive surgical approach to complex recurvatum deformity using biplanar osteotomy with multilevel stabilization, demonstrating excellent functional outcomes and sustained correction at 9-month follow-up. The technique employed addresses several critical aspects of deformity correction that has been extensively discussed in contemporary literature.
Surgical technique considerations
The biplanar osteotomy technique utilized in this case represents an evolution in the management of complex recurvatum deformities. Johnson et al. demonstrated that osteotomy distal to the tibial tuberosity allows for multiplanar correction while maintaining patellofemoral mechanics [4]. Our approach of performing an 8 mm biplanar osteotomy of the tibial tuberosity is consistent with established principles that emphasize preservation of the patella tendon attachment while allowing anterior elevation [2]. The biplanar technique has been shown to be superior to traditional approaches as it can simultaneously address both osseous deformity and soft tissue components [6]. Nathan and Parikh [3] reported that opening wedge osteotomy proximal to the tibial tuberosity combined with tibial tuberosity osteotomy provides greater ability to adjust patellar height and achieve greater correction of deformity. This supports our decision to incorporate tibial tuberosity fixation with screws as part of the multilevel stabilization approach. The preservation of patellar height is crucial, as studies have demonstrated that osteotomies above the tibial tuberosity can significantly affect patellofemoral mechanics [7].
Bone graft selection and integration
The use of tricortical iliac bone graft in our case follows established principles for deformity correction. Capanna et al. demonstrated that osteotomy and placement of tricortical bone graft at the apex of deformity allow immediate and accurate alignment correction with low complication rates [8]. Borrelli et al. in their study of 17 patients showed 94% healing rates with tricortical iliac crest grafts, consistent with our patient’s excellent bone integration at 2 months and complete consolidation by 9 months [5].
Recent literature by Capanna et al. has further validated the use of tricortical iliac crest grafts for complex reconstructions, showing that these grafts provide excellent structural support and promote rapid healing. The authors emphasized that tricortical grafts are particularly valuable when significant bone loss or structural deficiency is present, which aligns with our case where substantial correction was required [8].
Stabilization methods and hardware considerations
The dual-pillar plating system employed in this case represents a comprehensive approach to fixation. Schwartz et al. demonstrated that lateral and medial double-plating fixation provides superior stability compared to single-plate constructs. Their study showed that double-plating significantly reduced the risk of hardware failure and loss of correction, particularly in complex deformities [9]. The use of locking distal T LOW PROFILE plates for both medial and lateral stabilization in our case follows this principle of achieving maximum stability through strategic hardware placement. The medial pillar stabilization with two screws on either side of the osteotomy and lateral pillar stabilization with one screw on either side reflects the differential loading patterns in knee biomechanics. This approach is supported by biomechanical studies showing that medial stabilization requires greater screw density due to higher compressive loads [10].
Comparison with alternative techniques
Several alternative approaches for recurvatum deformity correction have been described in recent literature. Bottlang M et al. reported excellent outcomes with anterior opening-wedge proximal tibial osteotomy for slope correction, achieving mean knee hyperextension reduction from 17–32° preoperatively to 0–7° postoperatively. However, their technique focused primarily on slope correction without addressing the complex anterior subluxation component present in our case [11]. The hexapod frame technique described by Johnson et al. offers gradual correction advantages but requires prolonged external fixation (average 225 days) compared to our single-stage approach. While hexapod frames allow fine-tuning during correction, the immediate definitive correction achieved in our case eliminated the need for prolonged external fixation and associated complications [4]. Banovetz et al. described biplanar proximal tibial opening-wedge osteotomy for chronic posterior cruciate ligament (PCL) tears with good outcomes, but their technique was specifically designed for PCL insufficiency rather than primary recurvatum deformity. The comprehensive approach in our case addresses both osseous and soft tissue components that contribute to complex recurvatum patterns [6].
Patellar height preservation
One of the critical advantages of our technique is the preservation of patellar height, which has been a significant concern in proximal tibial osteotomies. Ding T et al. demonstrated that patellar height changes significantly affect postoperative function and can lead to patellofemoral complications. The biplanar technique with tibial tuberosity osteotomy used in our case specifically addresses this concern by maintaining the tibial tuberosity-patella tendon relationship [7]. Recent studies by Nathan and Parikh have shown that tibial tuberosity osteotomy combined with opening wedge osteotomy provides superior control over patellar height compared to traditional techniques. Our patient’s maintenance of normal patellofemoral mechanics throughout follow-up supports this approach [3].
Complex recurvatum deformity with anterior knee subluxation represents a challenging orthopedic condition requiring precise surgical planning and execution. This single-stage approach – consisting of an 8 mm biplanar tibial tuberosity osteotomy, tricortical iliac crest bone graft augmentation, and dual-pillar plating – achieved and maintained full deformity correction, restored patellofemoral mechanics, and enabled complete pain resolution. Progressive functional gains culminated in unrestricted activities and return to sports by 9 months postoperatively. The use of tricortical grafts provided robust structural support and expedited bone healing, while multilevel stabilization ensured mechanical stability without hardware complications. This technique offers a reproducible and effective solution for similar complex genu recurvatum deformities, combining deformity correction, patellar height preservation, and early rehabilitation to optimize patient outcomes.
Early recognition and timely surgical intervention in complex genu recurvatum with anterior tibial subluxation can prevent long-term functional disability. A structured single-stage approach using biplanar osteotomy, bone graft augmentation, and dual-pillar fixation ensures stable correction; restores normal biomechanics; and supports rapid return to daily and sports activities.
References
- 1. Dirnberger J, Homan MD, Kennedy NI, LaPrade RF. Anterior opening wedge proximal tibial osteotomy for slope correction of genu recurvatum. Video Journal of Sports Medicine. 2024;4(3): doi:10.1177/26350254231213392. [Google Scholar] [PubMed] [CrossRef]
- 2. Dean CS, Chahla J, Moulton SG, Nitri M, Serra Cruz R, LaPrade RF. Anterolateral biplanar proximal tibial opening-wedge osteotomy. Arthrosc Tech 2016;5:e531-40. [Google Scholar] [PubMed]
- 3. Nathan ST, Parikh SN. Genu recurvatum after tibial tuberosity fracture. Case Rep Orthop 2013;2013:952978. [Google Scholar] [PubMed]
- 4. Johnson L, McCammon J, Cooper A. Correction of genu recurvatum deformity using a hexapod frame: A case series and review of the literature. Strategies Trauma Limb Reconstr 2021;16:116-9. [Google Scholar] [PubMed]
- 5. Borrelli J Jr., Leduc S, Gregush R, Ricci WM. Tricortical bone grafts for treatment of malaligned tibias and fibulas. Clin Orthop Realt Res 2009;467:1056-63. [Google Scholar] [PubMed]
- 6. Banovetz MT, Braaten JA, Homan MD, Kennedy NI, LaPrade RF. Biplanar proximal tibial opening wedge osteotomy for a chronic PCL tear with medial compartment arthritis. Video Journal of Sports Medicine. 2023;3(4):26350254231174911. doi:10.1177/26350254231174911. [Google Scholar] [PubMed] [CrossRef]
- 7. Ding T, Tan Y, Tian X, Xue Z, Ma S, Hu Y, et al. Patellar height after high tibial osteotomy of the distal tibial tuberosity: A retrospective study of age stratification. Comput Math Methods Med 2022;2022:7193902. [Google Scholar] [PubMed]
- 8. Capanna R, Bufalini C, Campanacci M. A new technique for reconstructions of large metadiaphyseal bone defects. Orthop Traumatol 1993;2:159-77. [Google Scholar] [PubMed]
- 9. Schwartz LB, Kingery M, Ganta A, Egol K, Konda S. Novel use of tricortical iliac crest bone allograft to reconstruct the lateral tibia plateau articular surface: A case series. J Orthop Case Rep 2025;15:22-7. [Google Scholar] [PubMed]
- 10. Bai Z, Gao S, Hu Z, Liang A. Comparison of clinical efficacy of lateral and lateral and medial double-plating fixation of distal femoral fractures. Sci Rep 2018;8:4863. [Google Scholar] [PubMed]
- 11. Bottlang M, Doornink J, Lujan TJ, Fitzpatrick DC, Marsh JL, Augat P, et al. Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am 2010;92 Suppl 2:12-22. [Google Scholar] [PubMed]