Intra-articular steroids may precipitate viral reactivation in susceptible individuals.
Dr. Kashif Akhtar Ahmed, Department of Orthopaedics, All India Institute of Medical Sciences, Silbharal, Changsari, Guwahati – 781101, Assam, India. E-mail: kashifahmed@aiimsguwahati.ac.in
Introduction: Ramsay Hunt syndrome (RHS) results from reactivation of latent varicella-zoster virus in the geniculate ganglion, typically presenting with otalgia, auricular vesicles, and ipsilateral facial palsy. While systemic immunosuppression is a recognized trigger, RHS following local corticosteroid injection is exceedingly rare.
Case Report: We report a 55-year-old woman who developed classical RHS 4 days after ultrasound-guided bilateral intra-articular triamcinolone injections for knee osteoarthritis. She received early oral acyclovir and achieved full recovery within 6 months.
Conclusion: This case suggests that even locally administered corticosteroids may precipitate viral reactivation in susceptible individuals. Vigilance for cranial neuropathies after regional steroid procedures is warranted, and prompt antiviral therapy remains essential for optimal outcomes.
Keywords: Acyclovir, herpes zoster, immunosuppression, osteoarthritis, Ramsay Hunt syndrome, triamcinolone.
Ramsay Hunt syndrome (RHS), also known as herpes zoster oticus, results from the reactivation of latent varicella-zoster virus (VZV) within the geniculate ganglion of the facial nerve. It classically presents with otalgia, vesicular eruptions around the ear, and ipsilateral lower motor neuron facial palsy [1]. Although systemic immunosuppression is a known precipitating factor, VZV reactivation following local corticosteroid injection is exceedingly rare. Intra-articular steroid injections are widely used for osteoarthritis management due to their potent anti-inflammatory properties, but they may occasionally cause transient immunosuppression [2,3]. We present a rare case of classical RHS that developed after an ultrasound (US)-guided intra-articular triamcinolone injection, highlighting the importance of early recognition, antiviral therapy, and vigilance for potential viral reactivation following regional steroid use. To our knowledge, a classic case of RHS following intra-articular steroid injection has never been reported before.
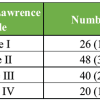
A 55-year-old female presented to our Pain Management Center 1 year ago with non-traumatic bilateral knee pain associated with mild swelling. She had no known comorbidities. Before presentation, she had received a 7-day course of anti-inflammatory analgesics and supportive therapy, which provided only mild relief. Radiographs of both knee joints revealed bilateral Kellgren–Lawrence grade II osteoarthritis. With appropriate written informed consent, US-guided intra-articular injections of triamcinolone acetonide (40 mg each) were administered into both knee joints. She reported significant pain relief within 48 h. However, on the 4th day, she developed pain on the left side of her face, predominantly around the ear, followed by painful vesicular eruptions on the same side. Two days later, she developed ipsilateral facial palsy, prompting her return to our center. The vesicular rashes were characteristic of a herpes zoster virus infection, and the facial palsy was of the lower motor neuron type (Fig. 1a). No associated visual or auditory disturbances were noted. On further inquiry, she reported a history of VZV infection (chickenpox) during adolescence. A discussion with the Ear, Nose, and Throat department was undertaken, and a diagnosis of RHS was established based on the characteristic constellation of clinical findings.

Figure 1: (a) Vesicular eruptions over the left periauricular and mandibular region with ipsilateral lower motor neuron facial palsy (face turned to one side) at presentation following ultrasound-guided intra-articular triamcinolone injection. (b) Complete clinical recovery with restoration of facial symmetry at 6-month follow-up.
Oral acyclovir, 800 mg 5 times daily, was prescribed for 10 days along with other supportive measures. Gradual improvement was observed, with near-complete recovery achieved by approximately 14 weeks. At 6-month follow-up, she had made a complete recovery (Fig. 1b). During the same period, US-guided bilateral intra-articular injections of hyaluronate were administered into both knee joints, resulting in good symptomatic relief on follow-up without any untoward effect.
RHS is an uncommon but well-recognized manifestation of VZV reactivation involving the geniculate ganglion, classically presenting with ipsilateral otalgia, vesicular eruptions of the auricle/hemiface, and lower-motor-neuron facial palsy [1]. Herpes zoster is common and occurs more frequently in immunocompromised individuals, with reactivation risk increased by immune suppression, prolonged corticosteroid therapy, local trauma, or advancing age [2,3,4,5]. Reactivation of dormant VZV in the geniculate ganglion is very rare (0.8%), with the thoracic sympathetic ganglia and the first division of the trigeminal nerve being the major sites of involvement [6]. In this case, the development of vesicles, ear pain, and subsequent facial palsy within days of a US-guided intra-articular triamcinolone injection raises a plausible association between corticosteroid exposure and VZV reactivation. Although administered locally, intra-articular steroids can produce transient immunosuppression and have been linked to a modest increase in infectious complications and latent viral reactivation [3]. This has been described previously in an elderly patient with multiple comorbidities who developed dermatomal VZV lesions distal to a knee methylprednisolone injection [2]; however, our patient exhibited a distinct presentation involving non-dermatomal lesions unrelated to the injection site. In the present case, reactivation of latent VZV within the geniculate ganglion with subsequent spread along the facial nerve offers the most plausible mechanism. Transient local immune alteration and procedural irritation of neural structures have been proposed as contributing factors in similar reports following regional interventions [7,8]. Although causality cannot be definitively concluded from a single case, the close temporal sequence and absence of other immunosuppressive conditions strengthen the likelihood of association and emphasize the importance of clinical awareness regarding herpes-family virus reactivation after intra-articular corticosteroid administration in susceptible individuals. Early recognition is critical because prompt antiviral therapy (commonly acyclovir or valacyclovir), often combined with short-course systemic corticosteroids, is associated with improved facial nerve recovery and reduced pain compared with delayed treatment. Published series and reviews report substantially better facial nerve outcomes when therapy is started within 72 h of paralysis onset [9,10]. Our patient received oral acyclovir early and experienced gradual improvement with near-complete recovery by 14 weeks and full recovery by 6 months, which is consistent with favorable outcomes reported in modern series. We did not administer systemic corticosteroids in our patient due to the fear of further immunosuppression.
This case highlights a rare but important association between intra-articular corticosteroid injection and subsequent reactivation of latent VZV presenting as classical RHS. Although causality cannot be definitively established, the close temporal onset of symptoms and absence of other immunosuppressive factors suggest that even locally administered steroids may precipitate viral reactivation in susceptible individuals. Clinicians should counsel patients regarding this uncommon risk when obtaining consent for joint steroid injections and maintain a high index of suspicion when otalgia, auricular vesicles, or acute facial weakness occur following regional corticosteroid procedures. Early recognition and prompt antiviral treatment remain critical to optimize neurological recovery. Further studies are warranted to clarify the incidence, mechanism, and patient-specific risk factors for herpes virus reactivation following intra-articular steroid therapy.
Intra-articular steroids may precipitate viral reactivation in susceptible individuals. Vigilance for cranial neuropathies after regional steroid procedures is warranted, and prompt antiviral therapy remains essential for optimal outcomes.
References
- 1. Goswami Y, Gaurkar SS. Ramsay hunt syndrome: An introduction, signs and symptoms, and treatment. Cureus 2023;15:e33688. [Google Scholar] [PubMed]
- 2. Fernandes NF, Malliah R, Stitik TP, Rozdeba P, Lambert WC, Schwartz RA. Herpes zoster following intra-articular corticosteroid injection. Acta Dermatovenerol Alp Pannonica Adriat 2009;18:28-30. [Google Scholar] [PubMed]
- 3. Zacay G, Heymann AD. Intra-articular and soft-tissue corticosteroid injections and risk of infections: Population-based self-controlled-risk-interval design. Pharmacoepidemiol Drug Saf 2023;32:718-25. [Google Scholar] [PubMed]
- 4. Zhang JX, Joesoef RM, Bialek S, Wang C, Harpaz R. Association of physical trauma with risk of herpes zoster among Medicare beneficiaries in the United States. J Infect Dis 2013;207:1007-11. [Google Scholar] [PubMed]
- 5. John AR, Canaday DH. Herpes zoster in the older adult. Infect Dis Clin North Am 2017;31:811-26. [Google Scholar] [PubMed]
- 6. Waldman RA, Waldman CW, Waldman SD. Ramsay hunt syndrome type 2: A review of an uncommon and unwelcome neurodermatologic disease. J Otolaryngol Rhinol 2015;1:003. [Google Scholar] [PubMed]
- 7. Furtado-Pessoa-De-Mendonca L, Encalada S, Hallo-Carrasco A, Mosquera-Moscoso J, Cascio MA, Pagan-Rosado R, et al. Herpes zoster prevalence following epidural steroid injections: A retrospective review. Interv Pain Med 2025;4:100597. [Google Scholar] [PubMed]
- 8. Koshy E, Mengting L, Kumar H, Jianbo W. Epidemiology, treatment and prevention of herpes zoster: A comprehensive review. Indian J Dermatol Venereol Leprol. 2018;84:251-262. [Google Scholar] [PubMed]
- 9. Kim SJ, Lee HY. Acute peripheral facial palsy: Recent guidelines and a systematic review of the literature. J Korean Med Sci 2020;35:e245. [Google Scholar] [PubMed]
- 10. Monsanto RD, Bittencourt AG, Bobato Neto NJ, Beilke SC, Lorenzetti FT, Salomone R. Treatment and Prognosis of Facial Palsy on Ramsay Hunt Syndrome: Results Based on a Review of the Literature. Int Arch Otorhinolaryngol. 2016;20:394-400. [Google Scholar] [PubMed]