Progressive kyphosis deformity can rarely lead to dislocation of the intervertebral joints, worsening myelopathy.
Dr. Hiroshi Noguchi, Department of Orthopedic Surgery, Faculty of Medicine, University of Tsukuba, 1-1-1 Tennodai, Tsukuba, Ibaraki 305-8575, Japan. E-mail: noguhiro0164@tsukuba-seikei.jp
Introduction In Japan, laminoplasty is often chosen over anterior surgery for the treatment cervical spondylotic myelopathy because most patients are the elderly with multiple stenoses. Laminoplasty is associated with lower perioperative risk, and it can be executed by inexperienced surgeons with relative ease. However, it is also associated with progression of kyphosis, which can result in the deterioration of neck pain and recurrence of myelopathy. Herein, we present a case in which kyphosis deformity progressed post-laminoplasty, resulting in intervertebral joint dislocation and worsening myelopathy.
Case Presentation A 70-year-old Japanese man who underwent laminoplasty 10 months ago, presented with worsening myelopathy symptoms that had recurred after previously persisting for several days. These symptoms were associated with restenosis of the spinal canal at the C4/5 level due to spondylolisthesis and facet dislocation. As a corrective surgery, we performed anterior-posterior surgery. His post-operative course was almost satisfactory, and post-operative magnetic resonance imaging showed an improvement in spinal cord compression.
Conclusion Progressive kyphosis deformity can rarely lead to dislocation of the intervertebral joints, worsening myelopathy. Although the prevention of kyphotic deformity is still difficult, laminoplasty should be performed in patients with a high risk of post-operative kyphosis, such as in this case, considering the possibility of deterioration of myelopathy associated with kyphosis.
Keywords Cervical spine, laminoplasty, kyphosis, facet dislocation.
The treatment for cervical spondylotic myelopathy can be divided into two distinct methods: Anterior and posterior surgeries. Laminoplasty, a representative procedure of posterior cervical spine surgery, is characterized by simultaneous multiple-level decompression and is widely performed in patients with spinal cord compression due to multiple intervertebral stenoses [1]. In Japan, laminoplasty is often chosen over anterior surgery [2] because most patients are the elderly with multiple stenoses. Moreover, the perioperative risk of laminoplasty is low, and it can be easily performed by relatively inexperienced surgeons. One of the well-known post-operative complications of laminoplasty is the progression of kyphosis, which can result in the deterioration of neck pain and recurrence of myelopathy. In this study, we describe a rare case of kyphosis post-laminoplasty with facet dislocation and worsening myelopathy.
History and examination
A 70-year-old Japanese man underwent cervical laminoplasty 10 months ago at another hospital for cervical spondylotic myelopathy. Postoperatively, his hand numbness had been improving; however, his cervical alignment became kyphotic (Fig. 1). Ten months after surgery, he experienced sudden onset of severe neck pain and numbness and muscle weakness in both upper limbs, following which he visited his previous doctor, who detected facet dislocation with progressive kyphotic deformity post-laminoplasty. The patient was referred to our department for further evaluation and treatment. He had a history of diabetes mellitus and alcoholic liver cirrhosis with no evidence of neuromuscular disease.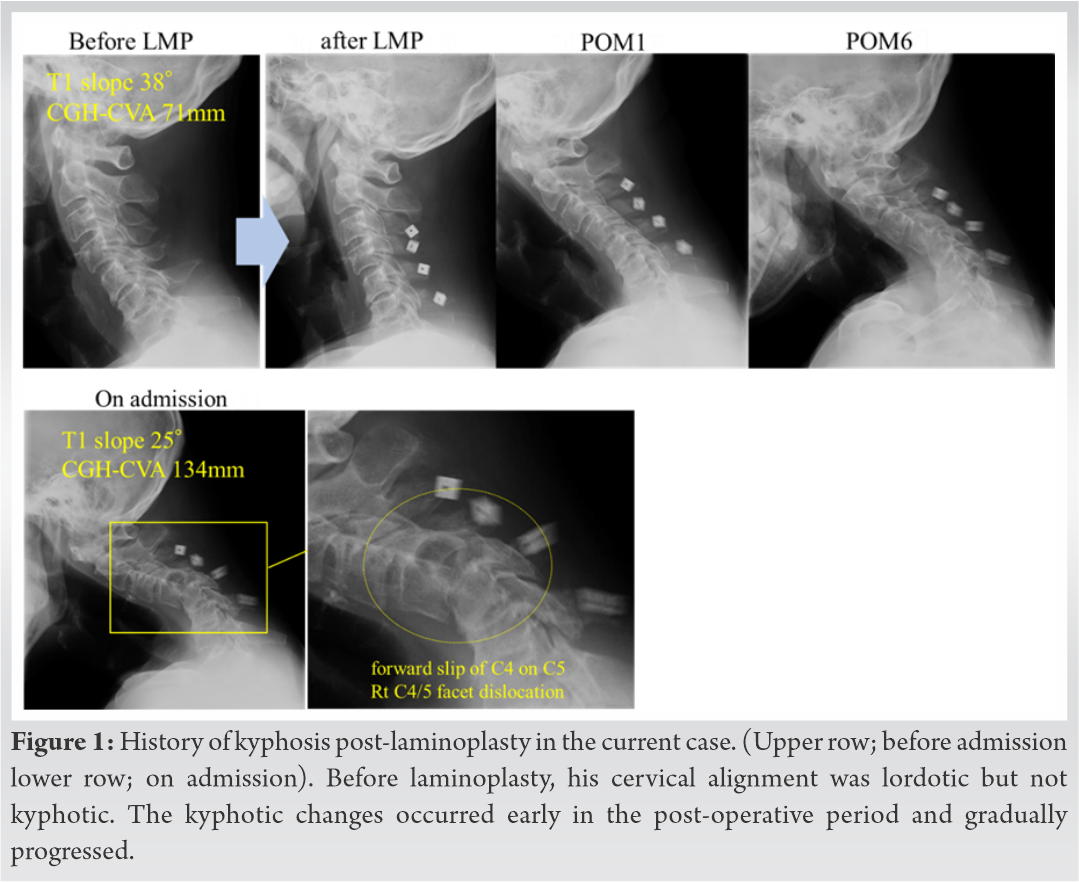
On admission, he was unable to stand or sit because of severe neck pain and complained of severe numbness and weakness in both upper limbs. The patient showed distal dominant upper limb muscle weakness (manual muscle testing level of 3–4/5). Decreased sensation was observed in both palms, and bladder-rectal function was slightly diminished. The patellar and Achilles tendon reflexes were enhanced in both sides, and the patient exhibited a spastic gait. The Japanese Orthopedic Association (JOA) score for cervical myelopathy was 7.5 points out of 17 (full marks).
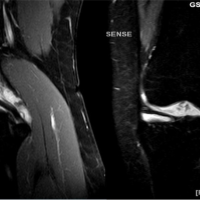
Before the initial surgery, his cervical alignment was lordotic but not kyphotic. Kyphosis occurred early in the post-operative period and gradually progressed. On admission, we observed severe kyphosis with a forward slip of C4 on C5 with C4/5 facet dislocation (Fig. 1). The sagittal alignment parameters of the cervical spine were as follows: C2-7 angle, -52; T1 slope, 25°; and center of gravity of the head (CGH)–C7 sagittal vertical axis (SVA), 134 mm. Computed tomography images revealed a C4/5 facet dislocation on the right side. Restenosis of the enlarged spinal canal at the C4/5 level was observed on magnetic resonance imaging (Fig. 2).
Surgery
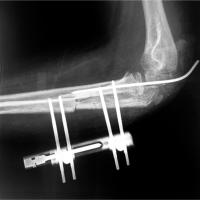
The patient was diagnosed with cervical kyphotic change with restenosis of the spinal canal at the C4/5 level by spondylolisthesis and facet dislocation, and anterior-posterior surgery was selected. First, we attempted and successfully performed the close reduction of facet dislocation under anesthesia. Second, we performed anterior cervical discectomy fusion with an intervertebral cage (CeSPACE®XP Interbody System, B. Braun Aesculap, Germany) filled with artificial bone (Affinos, Kuraray, Japan) at the C4/5 level to improve cervical alignment. Subsequently, we performed posterior cervical fusion with C3-6 lateral mass screws (SYMPHONY OCT System, DePuy Synthes, USA). After surgery, his cervical spine was corrected for lordosis. Post-operative cervical sagittal parameters were as follows: C2-7 angle, 2.5°; C4/5 angle, 3°; T1 slope, 30°; and CGH-SVA, 80 mm (Fig. 3).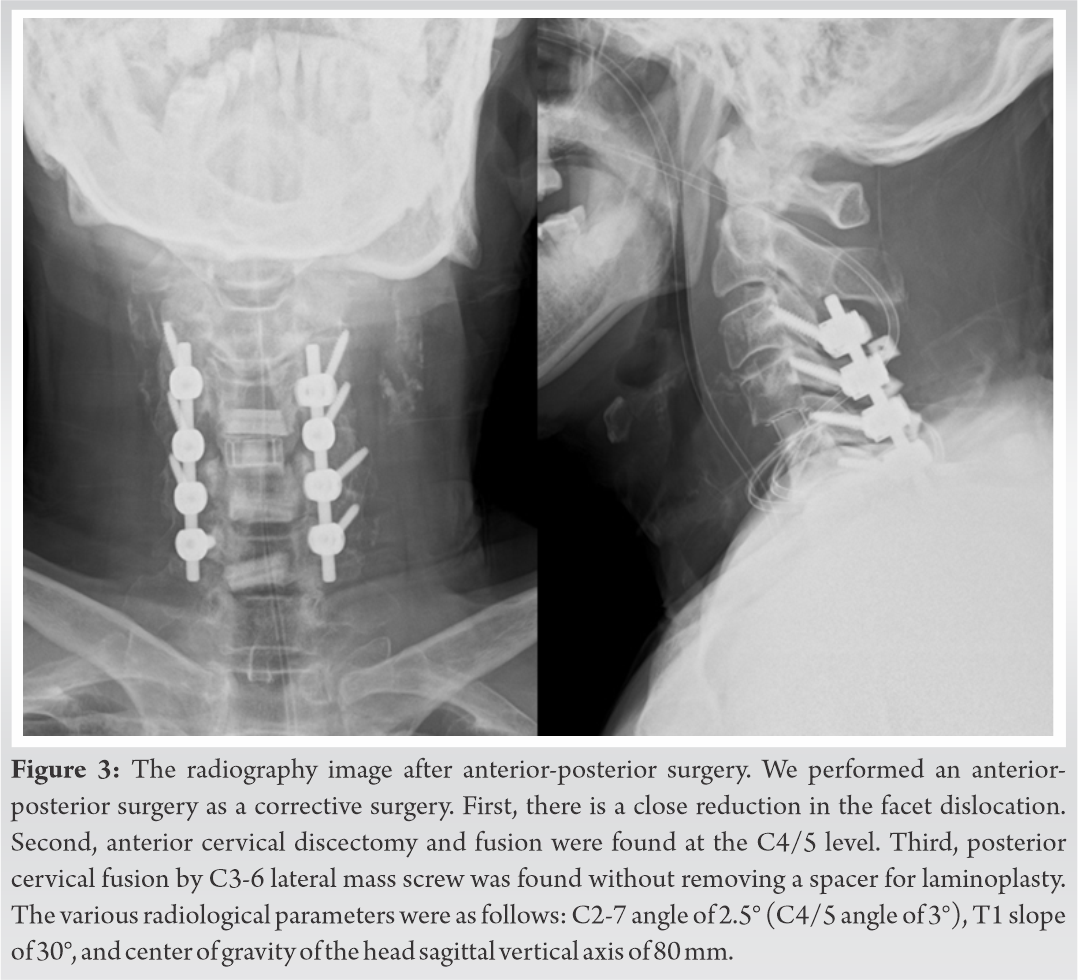
Post-operative course
The patient was kept intubated on the day of surgery and extubated 3 days after surgery to treat the swelling of the pharynx caused by the combined anterior-posterior surgery. His hand numbness and skilled movements improved immediately after surgery, and he was able to walk using a walker 1 week after surgery. Three weeks after surgery, the patient was transferred to the previous doctor for rehabilitation. The JOA score for cervical myelopathy improved to 10.5 points out of 17 (recovery rate of the JOA score, 31.6%) a year after surgery. Post-operative magnetic resonance imaging showed the attenuation of spinal cord compression, and interbody fusion at C4/5 was satisfactory on computed tomography images obtained 6 months after surgery (Fig. 4). Post-operative radiography revealed that his cervical spine was S shaped and slightly tilted forward without screw loosening. Cervical sagittal parameters at 12 months after surgery were as follows: C2-7 angle, −5°; T1 slope, 23°; and CGH-SVA, 81 mm (Fig. 4). The progression of kyphosis was carefully observed.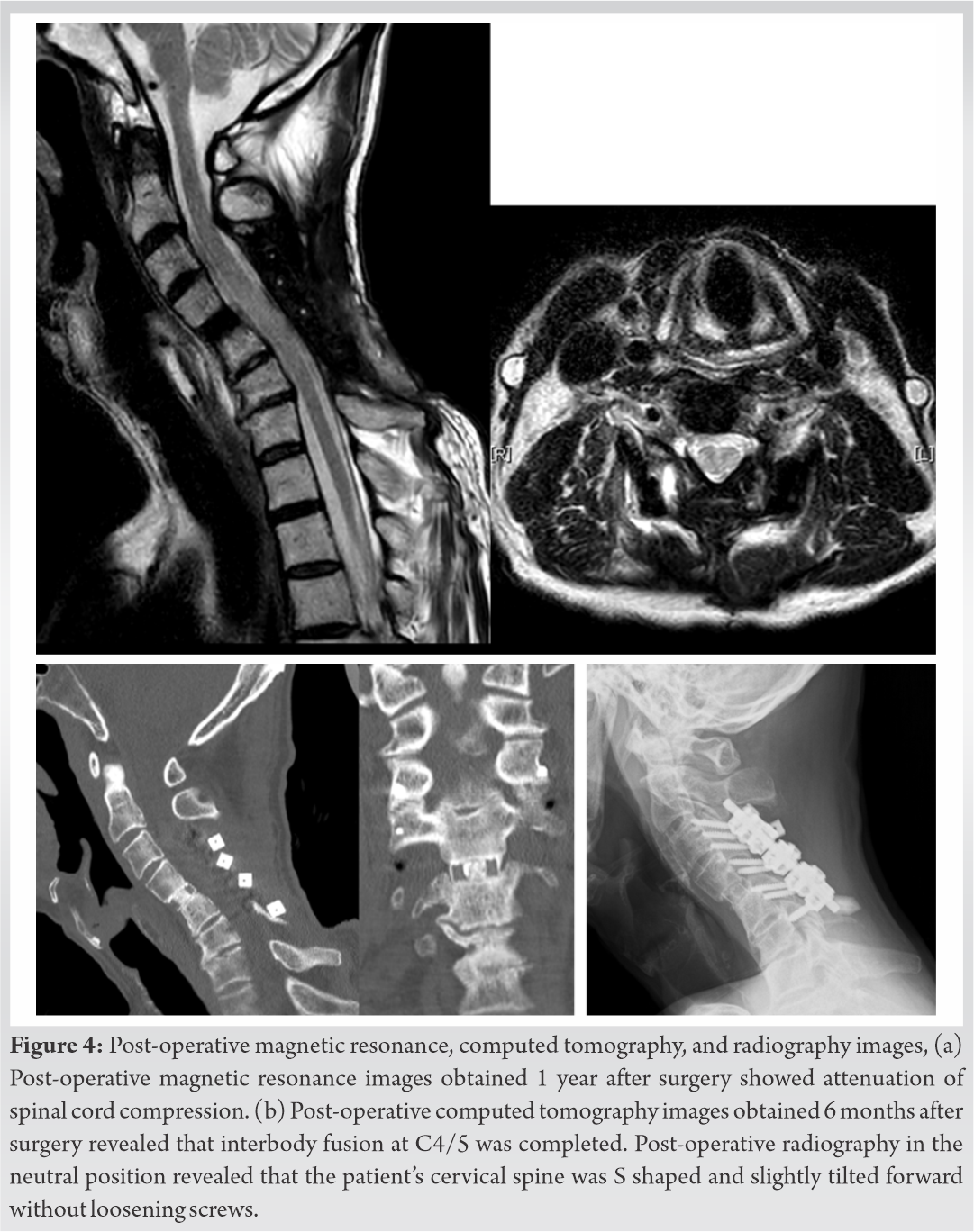
Facet dislocation due to kyphotic changes post laminoplasty, as in the present case, is very rare; therefore, we could not find similar reports, although post-operative cervical kyphosis after laminoplasty is a well-known post-operative complication. Post-operative kyphotic deformity can lead to unfavorable outcomes because kyphosis decreases posterior spinal cord shift, which is the main mechanism of spinal cord decompression by laminoplasty. The previous studies have revealed that post-operative kyphotic alignment changes are related to the deterioration of neurological symptoms [3,4]. Thus, spinal surgeons should take preventive actions against post-operative kyphotic deformities to maintain favorable long-term results.
A precise understanding of the etiology of laminoplasty kyphosis is mandatory to predict and prevent its recurrence. According to the previous reports, post-laminoplasty kyphosis is associated with multiple factors as outlined below: (1) Invasion to the posterior extensor muscles. Preservation of the cervical extensor muscles, which play an important role in maintaining cervical lordosis, is important for preventing post-laminoplasty kyphosis [5]. In particular, the preservation of the semispinalis muscle attached to the C2 spinous process is a key to preventing kyphosis. (2) Poor pre-operative cervical sagittal alignment. Lower C2-7 angle, higher T1 slope, and higher C2-7 SVA are reported as possible risk factors for post-operative kyphosis [6,7] (Fig. 5). Sakai et al. [8] and Sharma et al. [9] reported that the radiological risk factors for kyphotic change post-laminoplasty are CGH-SVA >42 mm and T1 slope >29.5°. (3) Pre-operative local instability (e. g., anterior slip).
In the present case, the pre-operative sagittal alignment parameters were as follows: C2-7 angle, 13.2°; T1 slope, 38°; and CGH-SVA, 71 mm. Pre-operative cervical spine lateral radiography in the flexion position showed a mild anterior slip at C4. Moreover, surgical records from a former hospital indicated that the C2 semispinalis had been invaded. Therefore, the present case fulfilled all possible risk criteria for post-laminoplasty kyphosis mentioned above.
The treatment strategy for patients with cervical spondylotic myelopathy at risk of post-laminoplasty kyphosis is controversial. In the present case, we chose anterior-posterior surgery as a salvage procedure because it could deal with any deformity. The C4/5 slipped vertebrae were successfully reduced by anterior cervical discectomy and the unstable posterior elements, including dislocated facet joints, were supported by posterior fixation. Based on the surgeon’s preference, the patient’s general condition, and the patient’s previous history, one of the following surgical techniques should be selected: Anterior, posterior, or combined [10,11,12].
Progressive kyphosis deformity can rarely lead to dislocation of the intervertebral joints, worsening myelopathy. When performing posterior surgery in a patient with a high risk of post-operative kyphotic deformity, the patient must be informed of the possibility that additional surgery may be required due to the deterioration of myelopathy associated with cervical kyphosis.
Progressive kyphosis deformity can rarely lead to dislocation of the intervertebral joints, worsening myelopathy. When performing posterior surgery in a patient with a high risk of post-operative kyphotic deformity, the patient must be informed of the possibility that additional surgery may be required due to the deterioration of myelopathy associated with cervical kyphosis. Even in the lordotic position, patients with a large SVA, T1 slope, and anterior slip should be recognized as a high risk of developing post-operative kyphosis.
References
- 1.Bow CH, Cheung E, Cheung CL, Xiao SM, Loong C, Soong C, et al. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int 2012;23:879-85. [Google Scholar | PubMed]
- 2.Harada A, Matsuyama Y, Nakano T, Deguchi M, Kuratsu S, Sueyoshi Y, et al. Nationwide survey of current medical practices for hospitalized elderly with spine fractures in Japan. J Orthop Sci 2010;15:79-85. [Google Scholar | PubMed]
- 3.Hu SS. Internal fixation in the osteoporotic spine. Spine 1997;22:43S-8. [Google Scholar | PubMed]
- 4.Taiji R, Takami M, Yukawa Y, Hashizume H, Minamide A, Nakagawa Y, et al. A short-segment fusion strategy using a wide-foot-plate expandable cage for vertebral pseudarthrosis after an osteoporotic vertebral fracture. J Neurosurg Spine 2020;33:1-8. [Google Scholar | PubMed]
- 5.Fukuda K, Katoh H, Takahashi Y, Kitamura K, Ikeda D. Minimally invasive anteroposterior combined surgery using lateral lumbar interbody fusion without corpectomy for treatment of lumbar spinal canal stenosis associated with osteoporotic vertebral collapse. J Neurosurg Spine 2021;1:1-9. [Google Scholar | PubMed]
- 6.Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: An analysis of the Nationwide Inpatient Sample database. Spine J 2014;14:2019-27. [Google Scholar | PubMed]
- 7.Yamamoto T, Yagi M, Suzuki S, Nori S, Tsuji O, Nagoshi N, et al. Limited cost benefit of lateral interbody fusion for adult spinal deformity surgery. Spine 2021;46:48-53. [Google Scholar | PubMed]
- 8.Arutyunyan GG, Angevine PD, Berven S. Cost-effectiveness in adult spinal deformity surgery. Neurosurgery 2018;83:597-601. [Google Scholar | PubMed]
- 9.Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H, et al. Complications associated with lateral interbody fusion: Nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine 2017;42:1478-84. [Google Scholar | PubMed]
- 10.Henry HY, Asuma MP, Wallace CS, Kelly MP, Kang DG. Should surgery for adult degenerative lumbar deformity be staged? Clin Spine Surg 2019;32:269-71. [Google Scholar | PubMed]
- 11.Yoshida G, Hasegawa T, Yamato Y, Kobayashi S, Oe S, Banno T, et al. Predicting perioperative complications in adult spinal deformity surgery using a simple sliding scale. Spine (Phila Pa 1976) 2018;43:562-70. [Google Scholar | PubMed]
- 12.Rhee JM, Basra S. Posterior surgery for cervical myelopathy: laminectomy, laminectomy with fusion, and laminoplasty. Asian Spine J 2008;2:114-26. [Google Scholar | PubMed]