Mini TightRope® is an ideal tool for the reconstruction of the intermetacarpal ligament after a delayed dislocation of the fifth carpometacarpal joint.
Dr. Keiichi Muramatsu, Department of Orthopedic Surgery, Nagato General Hospital, 85 Higashi-Fukawa, Nagato, Yamaguchi 759-4194, Japan. E-mail: kemuramatsu@outlook.jp
Introduction: Isolated dislocations of the fifth carpometacarpal joint (CMCJ) are uncommon injuries of the hand that is often missed but can be diagnosed correctly with a high index of suspicion and adequate imaging. Treatment for chronic cases is usually open reduction with temporary fixation using Kirschner wires, but for this case, we used Mini TightRope® as well to allow for early finger exercise. The case presented here is unique because of a delayed dislocation of a CMCJ detected 9 weeks from initial injury which was treated with a novel form of fixation with Mini TightRope®.
Case Report: A 70-year-old, right-hand dominant, male farmer injured his left hand when he slipped and fell on a concrete surface, landing on the ulnar side of his left hand. He was immediately seen in the clinic, just with a swollen left hand but no obvious deformity and with apparently normal PA and oblique radiographs of the hand. Nine weeks later, he came back due to persistent ulnar-sided hand pain; repeat radiographs and a CT scan of the left hand showed ulno-palmar dislocation of the fifth CMCJ. He then underwent trial closed reduction of the 5th CMCJ dislocation but failed. Open reduction, temporary K-wire fixation, and fixation using Mini TightRope® through the 4th and 5th metacarpals were done. A full range of motion of the hand was allowed immediately post-operative. Reduction was maintained and no complications were noted on subsequent follow-up visits.
Conclusion: This paper presents a brief literature review on 5th CMCJ dislocation, discussing the anatomic considerations contributing to joint stability, helpful radiographic parameters for diagnosis, and enumeration of treatment options.
Keywords: Fifth carpometacarpal joint, dislocation, reduction, mini tightrope, internal fixation
Dislocation of the fifth carpometacarpal joint (5th CMCJ) is a rare injury of the ulnar side of the hand. A correct diagnosis necessitates multiple radiographic views; not only the standard posteroanterior (PA) and oblique views but also lateral and 30° semi-pronated views of the hand should be performed to comprehensively evaluate the ulnar CMCJ when an injury is suspected. Several authors have listed radiographic parameters on the PA view to look out for ulnar offset of the 5th metacarpal base, loss of the parallel M lines (the lines formed by the second through fifth CMCJ and the distal ends of the carpal bones trapezoid, capitate, and hamate), asymmetry of the joint space, overlap of the opposing joint surfaces, and divergent metacarpal cascade lines (lines drawn through the longitudinal axes of the metacarpals should converge at a point about 2 cm proximal from the articular surface of the distal radius). On the lateral view, the fifth metacarpal shaft will be seen as not parallel with the uninjured metacarpals, an intermetacarpal angle of more than 10 degrees, and dislocation of the metacarpal shaft either dorsally or volarly [1,2]. Depending on the timing of diagnosis and stability of the joint, patients were treated with the following: Closed reduction casting, closed reduction and pinning with K-wires perpendicular to the 4th and 5th metacarpals or open reduction and pinning with K-wires. In this paper, we presented a case with a dislocation of the 5th CMCJ, wherein the patient presented with apparently normal PA and oblique radiographs of the hand but came back 9 weeks later due to persistent ulnar-sided pain of the hand with repeat radiographs showing the aforementioned dislocation.
Our patient is a 70-year-old male, right-hand dominant farmer who presented at the outpatient clinic after falling on the concrete and landing on his left hand. The patient complained of pain on the ulnar side of his hand and swelling was noted on examination. No apparent deformity of the little finger was noted, finger cascade was normal, and full range of motion was elicited but with pain on motion. Ulnar nerve function was intact. Radiographs of the left hand were performed and showed no fractures or dislocations (Fig. 1).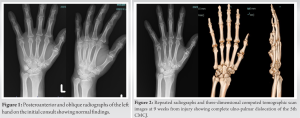
The patient denied any interval injuries but had persistent pain on the ulnar side of his left hand, prompting him to come back to the clinic 9 weeks later. Repeat radiographs showed complete ulno-palmar dislocation of the 5th CMCJ. A CT scan with 3-D reconstruction was also done, confirming said injury, and no associated fractures were noted (Fig. 2). Manual closed reduction was done under fluoroscopic guidance, but the joint was noted to be unstable when traction was removed. The patient was then indicated for open reduction of the 5th CMCJ.
The dislocated joint was approached from the dorsoulnar side and scar tissue was carefully removed from the 5th CMCJ (Fig. 3). All ligaments of the 5th CMCJ were torn including the pisometacarpal ligament. Using manual longitudinal traction and dorsally directed force to the 5th metacarpal base, the 5th CMCJ was repositioned to its anatomic location. A K-wire was inserted perpendicular to the long axis of the 5th through 4th metacarpals as a temporary fixation. Thereafter, intermetacarpal fixation was performed between the 4th and 5th metacarpals using Mini TightRope® (Arthrex, FL, USA) (Fig. 4). Under C-arm guidance, 1.2-mm holes were drilled with a trajectory about 1 cm distal from and parallel to the articular surfaces of the 5th metacarpal base to the 4th metacarpal base, approximating the original location of the intermetacarpal ligament. Together with one of the stainless-steel metal buttons, a loop of the Mini TightRope® construct is passed from the ulnar to the radial hole of the 4th metacarpal. Mini TightRope® construct was then pulled to tension until the button was flush on the radial cortex of the 4th metacarpal base. The two strands of Mini TightRope® FiberWire were then passed through the radial to ulnar holes of the 5th metacarpal, and second button was then loaded into the sutures and pushed until it was flush against the ulnar cortex of the 5th metacarpal. While maintaining tension, a provisional knot is created, and range of motion and finger cascade are then checked. Once deemed acceptable, sutures were then tied for up to 5 knots over the ulnar button. Remaining strands are then cut using a blade 11 scalpel. Capsule, fascia, and skin were then closed. Immediately after surgery, the patient was allowed to use his fingers freely with unrestricted range of motion. K-wires were removed at 2 weeks postoperatively. Follow-up radiograph at 1 year postoperatively showed maintained proper alignment of the 5th CMCJ (Fig. 5) and the little finger had no limitation of motion. There are no plans to remove the Mini TightRope®, unless the patient begins to complain of pain related to the aforementioned hardware.
Among all the CMC joints, the 5th CMCJ is the most mobile with an arc of 15–30° range of motion [3], hence making it the most common CMCJ prone to solitary dislocation. A direct blow or an axial high-energy force to the ulnar side of the hand is the usual mechanism of injury. 5th CMCJ dislocations are classified by Nalebuff into dorsal and volar dislocations. Dorsal dislocations are more common than volar dislocations. Volar or palmar dislocations are further sub-classified into radio-palmar or ulno-palmar. In radio-palmar injuries, all the ligamentous attachments are torn from the fifth metacarpal base, while in ulno-palmar injuries, the pisometacarpal ligament remains intact together with the flexor carpi radialis and extensor carpi ulnaris tendons [4]. Based on the cadaveric study of hands by Nakamura et al., the intermetacarpal interosseous ligament appears to be the primary stabilizer of the 5th CMCJ. They have observed that the 5th CMC joint is still difficult to dislocate even if they have deliberately divided the dorsal and volar carpometacarpal ligaments as long as the intermetacarpal ligament is intact. The flexor and extensor carpi ulnaris tendons, which both insert at the base of the fifth metacarpal, serve as the deforming forces that pull the metacarpal proximally [3]. Several case reports have been published about ulno-palmar 5th CMCJ dislocations [3, 5-10]. However, there has been no standard algorithm with regard to the treatment options. In general, closed reduction is performed, and immobilization with a cast or ulnar gutter splint for stable injuries, and percutaneous pinning may be needed if the joint is deemed unstable. An irreducible joint will be indicated for an open reduction with internal fixation with Kirschner wires, tension band suturing, or internal bracing. Villán et al. proposed an algorithm for the treatment of 5th CMCJ dislocation based on temporality (acute if less than 10 days), the position of the dislocation (dorsal, ulno-palmar, or radio-palmar), stability, and other factors. Acute injuries can most likely be treated through closed reduction with casting and or pinning for 4–6 weeks, depending on stability, while for chronic cases, patients would most likely undergo open reduction due to the presence of scar tissue or soft-tissue interposition [9]. Unreduced 5th CMCJ dislocation could result in complications such as grip weakness, stiffness, contractures, and post-traumatic arthritis. Our case appears to be very unique in the aspect that it was not a missed diagnosis of a 5th CMCJ dislocation, but the joint seemed to have dislocated slowly in the interim after the injury. The radiographs on the first consult appear to be normal. The parallel M lines are symmetrical, there is no apparent shortening of the 5th metacarpal in comparison to the other metacarpals, and there is no overlap of the CMCJ surface. On physical examination, the patient has no hand deformity that would give a suspicion of dislocation such as little finger abduction, dimpling at the 5th metacarpal base, or shortening and catching of the little finger. We thought that the intermetacarpal ligament could have still been intact at first or only partially torn which might have offered some stability and prevented the dislocation. Since the patient was sent home and allowed to use his hand, the intermetacarpal ligament may have eventually completely torn, thus causing the 5th CMCJ to dislocate. Based on the present literature, for cases with a CMCJ dislocation that warranted open reduction, most authors only used Kirschner wires to temporarily hold their reduction [6-10]. Among the case reports, only three authors attempted to reconstruct the torn ligaments. McWhorter reported a case with a radio-palmar 5th CMCJ dislocation, wherein he sutured the base of the 5th metacarpal to the hamate [5]. Xiao et al. did a tension band suture of the avulsed rim of the 5th metacarpal and the capsule on an ulno-palmar 5th CMCJ dislocation [7]. Villán et al. placed an internal brace (Arthrex, FL, USA) at the dorsal side of the 5th metacarpal base, 4th metacarpal base, and hamate [9], but this procedure is not an anatomical reconstruction.
Given our knowledge of the anatomy and stabilizers of the 5th CMCJ, we thought that it was best to place a Mini TightRope® construct between the 4th and 5th metacarpal base, to approximate the anatomic location of the intermetacarpal ligament, hence reconstructing the primary stabilizer of the 5th CMCJ. This type of stabilization had never been reported and allowed the patient to immediately use his hand, thus avoiding the sequelae of prolonged finger immobilization such as finger contractures and grip weakness.
Fifth CMCJ dislocation is an injury that can be managed through closed reduction and immobilization if detected and diagnosed acutely. For chronic dislocations, open reduction is often required to reduce the joint anatomically, followed by temporary fixation with a K-wire and immobilization for several weeks. Prolonged immobilization of the joints of the hand can result in contractures and joint stiffness. The use of Mini TightRope® to reconstruct the intermetacarpal ligament to the 4th and 5th metacarpal is a novel technique that orthopedic surgeons may consider to allow immediate range of motion of the affected hand and avoid the aforementioned complications.
References
- 1.Fisher MR, Rogers LF, Hendrix RW. Systematic approach to identifying fourth and fifth carpometacarpal joint dislocations. AJR Am J Roentgenol 1983;140:319-24. [Google Scholar | PubMed]
- 2.Hodgson PD, Shewring DJ. The ‘metacarpal cascade lines’; use in the diagnosis of dislocations of the carpometacarpal joints. J Hand Surg Eur Vol 2007;32:277-81. [Google Scholar | PubMed]
- 3.Nakamura K, Patterson RM, Viegas SF. The ligament and skeletal anatomy of the second through fifth carpometacarpal joints and adjacent structures. J Hand Surg Am 2001;26:1016-29. [Google Scholar | PubMed]
- 4.Nalebuff EA. Isolated anterior carpometacarpal dislocation of the fifth finger: Classification and case report. J Trauma 1968;8:1119-23. [Google Scholar | PubMed]
- 5.McWhorter GL. Isolated and complete dislocation of fifth carpometacarpal joint: Open operation. Surg Clin Chicago 1918;2:793-6. [Google Scholar | PubMed]
- 6.Boltuch AD, Harker JN. Operative intervention for a chronic fifth carpometacarpal dislocation: A case report and review of literature. J Orthop Case Rep 2021;11:108-12. [Google Scholar | PubMed]
- 7.Xiao R, Stenquist D, Dyer G. Volar dislocation of the fifth carpometacarpal joint mistaken for radial collateral ligament injury. Orthop J Harvard Med School 2019;20:29-35. [Google Scholar | PubMed]
- 8.Lim Z, Sebastin SJ. Palmar dislocations of the 5(th) carpometacarpal joint: Case report of a rare injury and review of published cases. J Hand Surg Asian Pac Vol 2020;25:368-72. [Google Scholar | PubMed]
- 9.Villán JL, Latorre LF, Quintero JI, Serrano CL. Late presentation of palmar dislocation of the fifth metacarpal bone: Review of the literature, treatment algorithm, and case report. J Orthop Case Rep 2022;12:84-8. [Google Scholar | PubMed]
- 10.Chen VT. Dislocation of carpometacarpal joint of the little finger. J Hand Surg Br 1987;12:260-3. [Google Scholar | PubMed]