The technique of dual plating is an economically viable option for failed megaprothesis particularly in people who are young and engaged in high-demand work.
Dr. Mantu Jain, Department of Orthopedics, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Knee arthrodesis following failed total knee arthroplasty is a viable limb salvage option, and this procedure is reserved for failed two-stage revision surgery in severe comorbid patients with irreparable extensor mechanism disruption, severe instability, and extensive soft tissue loss. Knee arthrodesis using a dual-plate construct has been scarcely reported. We report a case of knee arthrodesis using a dual-plate construct in a male in his 20s who presented to us with a broken distal femur megaprosthesis.
Case Report: An anterior midline incision was given. The cement mantle and broken prosthetic components were removed. The bone surfaces were freshened up and fixed using two orthogonal locking plates. After 4 months, there was a solid fusion in the knee, and the patient started walking independently with a short limb gait. The patient was advised limb lengthening for a shortening of 3 cm, but he denied it and managed with a shoe raise. After 4 years, he was pain free, and radiographs revealed a solid knee fusion. The patient was fully satisfied with the procedure, and he resumed manual work.
Conclusion: This case report revealed that knee arthrodesis using a dual-plate construct is an economically viable salvage option for failed distal femur megaprosthesis.
Keywords: Megaprosthesis, broken, knee arthrodesis, dual plating.
Knee arthrodesis following failed total knee arthroplasty is a viable limb salvage option, and this procedure is reserved for failed two-stage revision surgery in severe comorbid patients with irreparable extensor mechanism disruption, severe instability, and extensive soft-tissue loss. Numerous techniques and devices have been used to achieve knee fusion, such as intramedullary nails, compression plates, cannulated screws, and external fixators [1-4]. The technique to be adopted for knee fusion depends on available bone stock, soft-tissue condition, leg length discrepancy, presence of infection, and surgeon experience. The most commonly used technique for arthrodesis is intramedullary nailing. However, such long intramedullary devices are not always available. The other potential drawbacks include long operative times, huge blood loss, nail migration, loss of anatomic valgus knee alignment, and lack of tibial rotational control [4-6]. Moreover, it is difficult to put a nail in if there is a proximal hip prosthesis or in the presence of a bony deformity. External fixators, on the other hand, can be performed in the presence of an infection and large bone defects. However, it is not acceptable for many patients to mobilize with a bulky construct [3]. The pin tract infections and the long duration of treatment are other obstacles to the treatment of a patient [7]. The use of cannulated screws has also been described in the literature [8]. The screws can only be used in the presence of good bone stock. In addition, rigid immobilization is required by any other means, such as casts or external fixators, to ensure a satisfactory fusion. The dual-plate technique for knee arthrodesis was first described in 1913 for the treatment of tuberculosis of the knee [9]. This technique has several advantages, including debridement and knee fusion through the same incision, compression at the fusion site, and fixation even in the case of surrounding hardware (such as the long femoral stem of total hip arthroplasty or antegrade femoral nail) and extra-articular deformity. However, there are limited data about this technique. Each technique has its own merits and demerits, and no technique has been proven to be superior to others in all situations [10,11]. The available literature on knee arthrodesis is mainly following failed total knee arthroplasty, and there are only a few case reports following failed megaprosthesis. The bone defect following a failed megaprosthesis is massive and hence poses a challenge to achieving fusion. We report repost a case of knee fusion using a dual-plate construct in a young patient following a broken distal femur megaprosthesis. To the best of our knowledge, the literature has no reports on plate construct fusion following failed distal femur megaprosthesis. Consent for the publication of this case report was obtained.
A male in his 20s, a manual laborer by occupation, presented with severe pain around the left knee after a fall while walking. The pain was constant and increased with a slight movement of the limb. He was walking with the help of a pair of crutches, non-weight-bearing on the affected side. He had a history of distal femur megaprosthesis surgery 5 years ago for management of an infected open injury of the distal femur with extensive bone loss. However, the details of the procedure and images were not available to the patient. Anterior-posterior and lateral radiographs of the knee revealed a broken distal femur megaprosthesis (Fig. 1). The prosthesis was broken at the junction of the stem and shaft. Blood investigations revealed normal complete blood counts (TLC 8400/mm3), erythrocyte sedimentation rate (19 mm/h), and C-reactive protein (3 mg/dL). As there were no clinical signs of infection and the laboratory markers were normal, infection risk was excluded.
The patient was advised for revision of the distal femur megaprosthesis. However, the patient could not afford the cost of the prosthesis and expressed his desire to resume manual work. He revealed that his financial condition had deteriorated over the last 5 years after the prosthetic implantation as he was not able to perform physical labor.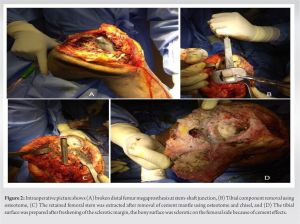
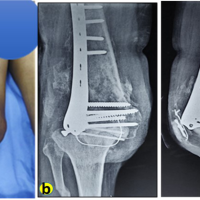
As per his demand and financial condition, knee arthrodesis was planned. After due consent from the patient and a pre-anesthetic evaluation, we proceeded with the removal of the broken implant, followed by knee fusion. The previous midline scar was used as the line of incision, and a medial knee joint arthrotomy was performed. On flexing the knee joint, the broken distal end of the prosthesis was delivered. The cement mantle was removed with an osteotome. The proximal part of the prosthesis had to been pulled out using an extractor. We used 1.5 mm K-wire to drill around the component and break the prosthesis-cement bonding, and later, using multiple curettes and a fine osteotome, we removed the cement mantle. The tibial component was then removed using multiple stack osteotomes (Fig. 2), and similarly, the cement was removed. As a backup, we were prepared to place a screw in the stem and use a slap hammer to extract. The patient was explained about creating a cortical window or corticotomy below or above the prosthesis, breaking the cement mantle, and pushing the component toward the joint in case the need arises. Accordingly, all-size implants were kept ready. The surrounding devitalized soft tissues were debrided. The bone surfaces were freshened up and approximated in near-anatomical positions. The apposed bony surfaces were provisionally fixed with K-wires in the desired position (neutral coronal and sagittal alignments with 15° external rotation), followed by definite fixation with two orthogonal limited contact dynamic compression plates contoured to the surface: one on the medial aspect (6-hole combi-hole locking plate) and the other on the anterior aspect (11-hole combi-hole locking plate) (Fig. 3). The construct was found to be stable. A cancellous bone graft harvested from the iliac crest was applied at the fusion site to augment the process of healing. The tissue samples from the knee joint were sent for culture and a frozen section. A negative suction drain was placed, and the wound was closed in layers. The histopathology and culture reports did not reveal any signs of infection.
The post-operative period was uneventful. There were no distal neurovascular deficits; however, the limb was shortened by 3 cm. The postoperative radiographs were satisfactory. He was advised for an isometric quadriceps strengthening exercise, hip abductor muscle strengthening exercise, and ankle pump. The patient was mobilized with a walker on the next day of surgery, with non-weight bearing on the affected limb for 6 weeks. After that, toe touch weight bearing was started, and full weight bearing was allowed once complete osseous union was achieved at the fusion site (4 months).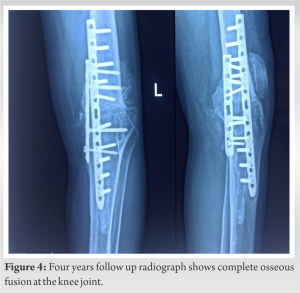
The patient was followed up biweekly for the 1st month and once a month thereafter. At the end of 3 months, the patient started walking independently without complaining of pain. However, he had a short-limb gait, and it improved after the shoe raise. The patient was advised on limb lengthening, but he denied it. He was very happy to resume his daily work. At the end of 4 years, the X-ray showed solid union at the knee arthrodesis site without complaint of back pain or any other joint pain (Fig. 4). He does not want a removal surgery at present.
Modular megaprostheses are special bone and joint prostheses that can bridge and compensate for large bone defects caused by the loss of bone stock [12]. These megaprostheses have now become a popular treatment option among orthopedic surgeons, and they not only preserve joint movement but also improve quality of life and maintain an intact body image. Earlier, their use was limited to oncology practices. But now, their use has been extended to the treatment of complex fractures, non-unions, and failed arthroplasties [13,14]. Patients treated with megaprosthesis have 5–10 times higher complication rates than normal arthroplasty patients. The incidences of infection, implant breakage, periprosthetic fracture, aseptic loosening, and functional limitation are higher in these individuals [15-17]. In the case of megaprosthesis, the incidence of implant breakage can be as high as 13% in the first 5 years [18]. The most common site of implant breakage is near the stem-shaft junction of the megaprosthesis [16]. In active individuals, the risk is even higher because of increased activities and functional demands. This could be the reason for the early breakage of the implant in our case. Management of broken megaprostheses is challenging. In the past, authors have revised a broken megaprosthesis with another megaprosthesis and reported good functional outcomes [19,20]. However, these devices are expensive and may not be suitable for manual laborers willing to resume their work. In such a scenario, knee arthrodesis is an economically viable option as it meets the demand of the patient and is cost-effective. Knee arthrodesis produces a painless, stable joint that can help in walking at the expense of joint movements. Recently, knee arthrodesis using the intramedullary device has been preferred over plating or an external fixator [21,22]. However, the availability of long nails, the curvature of the femur or tibia, and incisions at other sites are major limitations. Even prior surgery with a cemented stem renders the bone sclerotic and brittle, or at times, osteolytic [23]. Reaming the medullary canal in the sclerotic bone can be difficult, and it may lead to inadvertent cortical penetration, causing an iatrogenic fracture. Most of these problems can be obviated by the two-plate construct fusion of the knee. The major advantages are single incision and rigid fixation by adequate compression at the fusion site by the orthogonal plates. Unlike following failed total knee arthroplasty, the large bone defect created after the removal of the megaprosthesis increases the risk of non-union. Usually, after the extraction of total knee prostheses, the cancellous exposed bones of the metaphyseal regions on both the femoral and tibial sides provide more surface area of contact. However, this is not the scenario after extraction of the distal femur megaprosthesis; in this instance, the diaphyseal part of the femur is apposed to the metaphyseal region, thereby increasing the risk of non-union. Because of the cement exposure, the bones are also sclerotic and brittle, thus further increasing the risk of non-union. In such cases, the surgeon must freshen up the margins until bleeding bone surfaces are available for apposition. Probably, a good surgical technique, adequate compression with combi-hole locking plates, and cancellous bone grafting resulted in solid union at the fusion site in our case. There are very few reports on the dual-plate construct in knee fusion. In their review of salvage procedures for infected hip and knee arthroplasty, Mahmoud et al. reported that the dual-plate construct has minimal complications rates (9%) compared to intramedullary nails (55–57%), external fixators (24–80%), cannulated screws (25%), and the Stanmore prosthesis (22%) [11]. Kuo et al. used locking compression plates for knee fusion in 3 patients with infected total knee arthroplasty and reported successful fusion in all cases [1]. Nichols et al. used a parallel construct of dual-compression plating in 11 patients with failed arthroplasty and reported satisfactory fusion in all the patients after an average of 5.6 months [24]. They reported one femoral stress fracture (4.5%) and one persistent infection (4.5%). Lucas and Murray used a perpendicular construct of plates consisting of an anterior and medial plate for arthrodesis of the knee in 18 patients [25]. They achieved successful fusion in 17 cases, and only one patient required a second procedure to achieve fusion. Infection, limb length discrepancy, stress fracture, and non-union are potential complications following dual plating [11,26]. Ransone et al. reported a series of three peri-implant fractures following a dual-plate construct for knee fusion [26]. The main reason for these fractures is the excessive stress on the surrounding bone. The staggered configuration of plates can reduce the incidence of stress fractures. The increased infection rate has been reported following plate fixation in prosthetic joint infection cases. We believe that knee arthrodesis is an easy, cost-effective, and reliable way to deal with knee instabilities and can be taken up in the case of a broken mega prosthesis. This will not only help in early mobilization but also preserve the appearance of the limb. The only shortcoming in this surgery is limb shortening, which is quite obvious due to the pre-existing bone loss. This can be managed by using a shoe raise (till a 5 cm limb length discrepancy) or a limb lengthening procedure by bone transport.
In summary, knee arthrodesis using a dual-locked plate construct is an economically viable option for salvage in broken distal femur megaprosthesis.
Knee arthrodesis following failed total knee arthroplasty is a viable limb salvage option, and this procedure is reserved for failed two-stage revision surgery in severe comorbid patients with irreparable extensor mechanism disruption, severe instability, and extensive soft tissue loss. The most commonly used technique for arthrodesis is intramedullary nailing. However, such long intramedullary devices are not always available, and they have their own potential drawbacks. The dual-plate technique has several advantages, including debridement and knee fusion through the same incision, compression at the fusion site, and fixation even in the case of surrounding hardware. Our case demonstrates the excellent outcome of its use.
References
- 1.Kuo AC, Meehan JP, Lee M. Knee fusion using dual platings with the locking compression plate. J Arthroplasty 2005;20:772-6. [Google Scholar | PubMed]
- 2.Figgie HE 3rd, Brody GA, Inglis AE, Sculco TP, Goldberg VM, Figgie MP. Knee arthrodesis following total knee arthroplasty in rheumatoid arthritis. Clin Orthop Relat Res 1987;224:237-43. [Google Scholar | PubMed]
- 3.Oostenbroek HJ, van Roermund PM. Arthrodesis of the knee after an infected arthroplasty using the Ilizarov method. J Bone Joint Surg Br 2001;83:50-4. [Google Scholar | PubMed]
- 4.Incavo SJ, Lilly JW, Bartlett CS, Churchill DL. Arthrodesis of the knee: Experience with intramedullary nailing. J Arthroplasty 2000;15:871-6. [Google Scholar | PubMed]
- 5.Puranen J, Kortelainen P, Jalovaara P. Arthrodesis of the knee with intramedullary nail fixation. J Bone Joint Surg Am 1990;72:433-42. [Google Scholar | PubMed]
- 6.Donley BG, Matthews LS, Kaufer H. Arthrodesis of the knee with an intramedullary nail. J Bone Joint Surg Am 1991;73:907-13. [Google Scholar | PubMed]
- 7.Manzotti A, Pullen C, Deromedis B, Catagni MA. Knee arthrodesis after infected total knee arthroplasty using the Ilizarov method. Clin Orthop Relat Res 2001;389:143-9. [Google Scholar | PubMed]
- 8.Lim HC, Bae JH, Hur CR, Oh JK, Han SH. Arthrodesis of the knee using cannulated screws. J Bone Joint Surg Br 2009;91:180-4. [Google Scholar | PubMed]
- 9.MacDonald JH, Agarwal S, Lorei MP, Johanson NA, Freiberg AA. Knee arthrodesis. J Am Acad Orthop Surg 2006;14:154-63. [Google Scholar | PubMed]
- 10.Osgood RB. The end results of excision of the knee for tuberculosis with and without the use of bone plates. Boston Med Surg J 1913;169:123. [Google Scholar | PubMed]
- 11.Mahmoud SS, Sukeik M, Alazzawi S, Shaath M, Sabri O. Salvage procedures for management of prosthetic joint infection after hip and knee replacements. Open Orthop J 2016;10:600-14. [Google Scholar | PubMed]
- 12.Lundh F, Sayed-Noor AS, Brosjö O, Bauer H. Megaprosthetic reconstruction for periprosthetic or highly comminuted fractures of the hip and knee. Eur J Orthop Surg Traumatol 2014;24:553-7. [Google Scholar | PubMed]
- 13.Freedman EL, Hak DJ, Johnson EE, Eckardt JJ. Total knee replacement including a modular distal femoral component in elderly patients with acute fracture or nonunion. J Orthop Trauma 1995;9:231-7. [Google Scholar | PubMed]
- 14.Mortazavi SM, Kurd MF, Bender B, Post Z, Parvizi J, Purtill JJ. Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty. J Arthroplasty 2010;25:775-80. [Google Scholar | PubMed]
- 15.Ahlmann ER, Menendez LR, Kermani C, Gotha H. Survivorship and clinical outcome of modular endoprosthetic reconstruction for neoplastic disease of the lower limb. J Bone Joint Surg Br 2006;88:790-5. [Google Scholar | PubMed]
- 16.Gosheger G, Gebert C, Ahrens H, Streitbuerger A, Winkelmann W, Hardes J. Endoprosthetic reconstruction in 250 patients with sarcoma. Clin Orthop Relat Res 2006;450:164-71. [Google Scholar | PubMed]
- 17.Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury 2007;38:651-4. [Google Scholar | PubMed]
- 18.Coathup MJ, Batta V, Pollock RC, Aston WJ, Cannon SR, Skinner JA, et al. Long-term survival of cemented distal femoral endoprostheses with a hydroxyapatite-coated collar: A histological study and a radiographic follow-up. J Bone Joint Surg Am 2013;95:1569-75. [Google Scholar | PubMed]
- 19.Calori GM, Colombo M, Ripamonti C, Malagoli E, Mazza E, Fadigati P, et al. Megaprosthesis in large bone defects: opportunity or chimaera? Injury 2014;45:388-93. [Google Scholar | PubMed]
- 20.Agarwal M, Gulia A, Ravi B, Ghyar R, Puri A. Revision of broken knee megaprostheses: New solution to old problems. Clin Orthop Relat Res 2010;468:2904-13. [Google Scholar | PubMed]
- 21.Arroyo JS, Garvin KL, Neff JR. Arthrodesis of the knee with a modular titanium intramedullary nail. J Bone Joint Surg Am 1997;79:26-35. [Google Scholar | PubMed]
- 22.Wiedel JD. Salvage of infected total knee fusion: The last option. Clin Orthop Relat Res 2002;404:139-42. [Google Scholar | PubMed]
- 23.Vaishya R, Chauhan M, Vaish A. Bone cement. J Clin Orthop Trauma 2013;4:157-63. [Google Scholar | PubMed]
- 24.Nichols SJ, Landon GC, Tullos HS. Arthrodesis with dual plates after failed total knee arthroplasty. J Bone Joint Surg Am 1991;73:1020-4. [Google Scholar | PubMed]
- 25.Lucas DB, Murray WR. Arthrodesis of the knee by double-plating. JBJS 1961;43:795-808. [Google Scholar | PubMed]
- 26.Ransone M, Fehring K, Curtin B, Mason JB. Peri-implant fracture after dual-plating knee arthrodesis for failed total knee arthroplasty: Case series. Arthroplast Today 2019;5:453-64. [Google Scholar | PubMed]