Achromobacter xylosoxidans is a pathogen capable of causing prosthetic joint infection even in immunocompetent patients.
Dr. Mukund Madhav Ojha, Department of Orthopaedic, AIIMS, New Delhi, India. E-mail: mukund1203@gmail.com
Introduction: Achromobacter xylosoxidans is an uncommon opportunistic organism, mainly causing infection in immune-compromised hosts. A. xylosoxidans is a non-fermenting Gram-negative bacillus. Being closely associated with Alcaligenes species was also called A. xylosoxidans.
Case Report: A few cases of periprosthetic infection by A. xylosoxidans have been reported outside India. A periprosthetic infection with A. xylosoxidans following a total knee arthroplasty is reported in a female.
Conclusion: A. xylosoxidans is a pathogen capable of causing prosthetic joint infection even in immunocompetent patients. Thorough debridement and appropriate antibiotic treatment is essential for the success of revision surgery.
Keywords: Prosthetic joint infection, total knee arthroplasty, Achromobacter xylosoxidans.
Achromobacter xylosoxidans is an uncommon opportunistic organism, mainly causing infection in immune-compromised hosts. A. xylosoxidans is a non-fermenting Gram-negative bacillus. Being closely associated with Alcaligenes species was also called as Alcaligenes xylosoxidans [1]. First identified and described by Yabuchi and Ohyama in 1971 from seven cases of chronic otitis media, it belongs to the family alcaligenaceae and genus achromobacter [2], with two subspecies, namely xylosoxidans, and denitrificans. Few cases of periprosthetic infection by A. xylosoxidans have been reported outside India [3]. Here is a case of periprosthetic infection with A. xylosoxidans following a total knee arthroplasty is reported in a female.
A 61-year-old non-diabetic, non-hypertensive female was admitted complaining of pain, swelling, and pus discharge from her right knee. She was operated on outside our institute for bilateral knee end-stage arthritis with bilateral total knee arthroplasty (TKA) done 1 year ago. She underwent debridement and liner exchange 2 months back for an infected right TKA outside our institute. On pre-operative physical examination, the thigh and calf muscles were wasting, and a healed surgical scar with one discharging sinus with seropurulent discharge in the infrapatellar region was present. Pre-operative x-rays of the right knee show loosening of tibial and femoral components (Fig. 1). Blood investigations were done showing raised erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels and raised total leukocyte count (TLC). Synovial fluid analysis shows increased leukocyte numbers and more than 90% of neutrophils. Under the impression of deep prosthesis infection, a two-stage revision TKA operation was planned, and the patient underwent Stage I revision of the right TKA. Antibiotics were stopped 2 weeks before Stage I surgery to increase the efficacy of culture results.
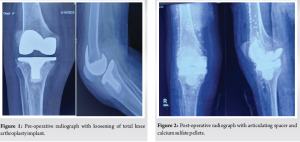
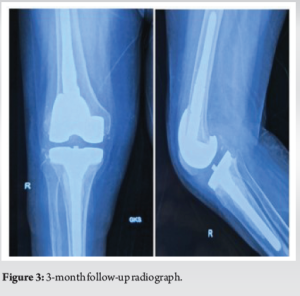
TKA prosthesis removal was done with debridement and irrigation with a temporary articulating knee cement spacer with antibiotics (vancomycin 1 g + colistin 1 MIU) and calcium sulfate pellets application (Fig. 2). Extracted implants were sent for sonication, synovial fluid specimens, and five deep tissue samples from the medial and lateral gutter, posterior capsule, and supra and infrapatellar region were taken and divided into two and sent for aerobic and anaerobic cultures at the time of debridement. The patient was mobilized postoperatively with a knee ROM brace. Postoperatively alternate day basis, ESR and CRP were done and showed a decreasing trend. The operative specimen’s implants and synovial tissue cultures revealed A. xylosoxidans as the causative organism. The patient then received intravenous antibiotics (cefoperazone + sulbactam 2 g iv BD) according to the results of the antibiotic sensitivity testing and after consulting with the infectious department medical team. Clinically, the knee was cool, non-tender, and showed no external signs of infection. The CRP decreased after treatment with cefoperazone + sulbactam, pain, and wound discharge improved and the patient was planned for 6-week IV antibiotics coverage. The patient underwent Stage II revision after 8 weeks when CRP and ESR were within normal limits. After 3 months of follow-up, patient is doing well with no local and systemic signs and symptoms of infections (Fig. 3).
A. xylosoxidans is a Gram-negative bacillus widespread in the natural environment [4]. It is an opportunistic human pathogen. Those whose immune response is weakened or who have underlying diseases linked to immunodeficiency are particularly vulnerable [5]. A review of the literature identified one case of septic arthritis caused by this organism after TKA. In this case, the patient had rheumatoid arthritis and was on high doses of prednisone, both conditions contributing to a weakened immune system [6]. A rare case of A. xylosoxidans septic arthritis in immunocompetent child patients has been reported in India. A. xylosoxidans is a rarer etiology of septic arthritis in pediatric patients [7]. The most familiar invasive manifestations of A. xylosoxidans are pneumonia, device-related infections, and primary uncomplicated bacteremia. Eshwara et al. have reported the first pancreatic pseudocyst report and local wound infection of metastatic ductal carcinoma due to A. xylosoxidans [1] and perinephric abscess case is reported by Vinod et al., from India [8]. A case of A. xylosoxidans septic arthritis was found in adult that too in immunocompromised systemic lupus erythematosus patients [9]. In our case, the synovial fluid culture might have been falsely negative because antibiotics were used before the joint aspiration from outside the institute. In addition, the value of microbiological cultures for diagnosing late periprosthetic infections is limited, standard methods may fail to detect biofilm-forming sessile or other fastidious slow-growing bacteria [10]. A. xylosoxidans strains frequently resistant to aminoglycosides, ampicillin, 1st– and 2nd-generation cephalosporins, and chloramphenicol. However, they typically respond to anti-pseudomonas third-generation cephalosporins, carbapenems, and trimethoprim-sulfamethoxazole [11].
This case demonstrates that A. xylosoxidans is a pathogen capable of causing prosthetic joint infection even in immunocompetent patients and implies that to cure the infection of late stage, removal of implant, thorough debridement and appropriate antibiotic treatment are essential for the success of revision surgery.
Uncommon pathogens like A. xylosoxidans can also lead to periprosthetic joint infection.
References
- 1.Eshwara VK, Mukhopadhyay C, Mohan S, Prakash R, Pai G. Two unique presentations of Achromobacter xylosoxidans infections in clinical settings. J Infect Dev Ctries 2011;5:138-41. [Google Scholar | PubMed]
- 2.Yabuuchi E, Yano I, Goto S, Tanimura E, Shiito T, Ohyama A. Description of Achromobacter xylosoxidans Yabuuchi and Ohyama 1971. Int J Syst Evol Microbiol 1974;24:470-7. [Google Scholar | PubMed]
- 3.Taylor P, Fischbein L. Prosthetic knee infection due to Achromobacter xylosoxidans. J Rheumatol 1992;19:992-3. [Google Scholar | PubMed]
- 4.Reverdy ME, Freney J, Fleurette J, Coulet M, Surgot M, Marmet D, et al. Nosocomial colonization and infection by Achromobacter xylosoxidans. J Clin Microbiol 1984;19:140-3. [Google Scholar | PubMed]
- 5.Ramos JM, Domine M, Ponte MC, Soriano F. Bacteremia caused by Alcaligenes (Achromobacter) xylosoxidans). Description of 3 cases and review of the literature. Enferm Infecc Microbiol Clin 1996;14:436-40. [Google Scholar | PubMed]
- 6.Lee SC, Nam CH, Park IS, Yoon JY, Jung KA, Hwang SH. Achromobacter xylosoxidans infection following total knee arthroplasty. J Korean Orthop Assoc 2014;49:385-8. [Google Scholar | PubMed]
- 7.Suryavanshi TK, Lalwani SK. Uncommon pathogen: Serious manifestation: A rare case of Achromobacter xylosoxidans septic arthritis in immunocompetetant patient. Indian J Pathol Microbiol 2015;58:58-3. [Google Scholar | PubMed]
- 8.Vinod V, Kumar A, Sanjeevan KV, Dinesh KR, Karim S. Perinephric abscess due to Achromobacter xylosoxidans following de-roofing of renal cyst. Surg Infect (Larchmt) 2013;14:422-3. [Google Scholar | PubMed]
- 9.San Miguel VV, Lavery JP, York JC, Lisse JR. Achromobacter xylosoxidans septic arthritis in a patient with systemic lupus erythematosus. Arthritis Rheum 1991;34:1484-5. [Google Scholar | PubMed]
- 10.Schäfer P, Fink B, Sandow D, Margull A, Berger I, Frommelt L. Prolonged bacterial culture to identify late periprosthetic joint infection: A promising strategy. Clin Infect Dis 2008;47:1403-9. [Google Scholar | PubMed]
- 11.Gales AC, Jones RN, Andrade SS, Sader HS. Antimicrobial susceptibility patterns of unusual nonfermentative gram-negative bacilli isolated from Latin America: Report from the SENTRY antimicrobial surveillance program (1997-2002). Mem Inst Oswaldo Cruz 2005;100:571-7 [Google Scholar | PubMed]
- 12.[Google Scholar | PubMed]









