Minimally invasive approach for corrective osteotomy of the phalanx.
Dr. Jonathan Persitz, Hand Program, Division of Plastic, Reconstructive and Aesthetic Surgery, University Health Network, Toronto Western Hospital, Affiliated with Temerty Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada. E-mail: jonathan.persitz@uhn.ca
Introduction: Patients facing post-traumatic malunion or congenital hand differences often contend with functional and cosmetic issues. Traditional correction methods involve open osteotomy, marked by drawbacks like scarring, non-union risks, prolonged rehabilitation, and adhesions. We therefore introduce a novel minimally invasive technique called Minimally Invasive Corrective Osteotomy of the Hand (MICO), which can be performed under local anesthesia. MICO employs a low-speed, high-torque burr to address finger malunions and congenital anomalies.
Case Report: A 49-year-old male patient, generally healthy and right hand dominant, presented with a post-traumatic left middle finger, middle phalanx malunion who underwent the MICO procedure, with a 1-year post-operative follow-up.
Conclusion: Our findings suggest that MICO offers a straightforward, reproducible, and delicate solution for correcting hand malunions and congenital finger deformities, potentially mitigating the well-established disadvantages and complications associated with the traditional open approach. Although early results of MICO are promising, a larger case series is needed to evaluate the superiority of this technique compared with current open corrective osteotomy methods. Level of Evidence: IV
Keywords: Osteotomy, minimal invasive surgery, finger deformity.
Congenital hand deformities and post-traumatic malunions of the hand can result in significant functional limitations and esthetic concerns. These deformities encompass conditions such as finger scissoring, tendon imbalance, and reduced grip strength [1]. Corrective osteotomy is a commonly employed procedure to restore proper anatomical alignment, thereby enhancing functional outcomes. This surgical intervention entails the precise incision and realignment of the deformed bone through the utilization of handheld osteotomes or saws, followed by the subsequent stabilization of the osteotomy site using pins or plates [2]. While an open surgical approach is frequently required to address these deformities, the available data regarding open corrective osteotomy procedures is limited. The existing literature primarily comprises outdated descriptions, predominantly composed of case series and case reports, which often feature limited follow-up data [3-5]. The drawbacks of an open approach are well described and include inevitable surgical incision scarring, non-unions due to abrupt soft-tissue dissection, long rehabilitation time, and up to 50% chance of adhesions in some of the studies [5-8]. The conventional osteotomy instruments, including oscillating saws and osteotomes, carry the inherent risk of causing nerve and soft-tissue damage, present limitations in terms of precise control during the procedure, and may result in substantial heat generation at the fracture site, with these issues being further compounded by the proximity of crucial anatomical structures surrounding the bones [6,9]. The utilization of low-speed burrs in minimally invasive surgery for correcting hallux valgus is an increasingly expanding approach, offering potential advantages such as smaller incisions, reduced pain and recovery duration, decreased likelihood of neurovascular complications, and enhanced range of motion (ROM) [10]. The objective of this study was to document the technical aspects and outcomes in a group of patients experiencing phalangeal deformities that were affecting both their appearance and functionality. In this context, we introduce a novel technique known as percutaneous Minimally Invasive Corrective Osteotomy of the Hand (MICO), which can be carried out using local anesthesia.
A 49-year-old male patient, in overall good health and right-hand dominant, sought medical attention due to an untreated malunion of the middle phalanges of his middle and ring fingers. He had not previously consulted with a hand specialist. On conducting a physical examination, it was apparent that the middle finger exhibited radial deviation, while the ring finger displayed ulnar deviation (Fig. 1). His primary concern was the radial deviation of his middle finger, which was significantly affecting his daily activities.

Radiographic images confirmed the radial deviation of the third finger and the ulnar deviation of the fourth finger, particularly around the middle phalanges.
The affected extremity was prepared and draped. We administered an 8 cc injection of 1% Lidocaine solution for digital nerve block. The precise correction site was identified as the point nearest to the center of correction and angulation (CORA). This had been determined preoperatively and confirmed using fluoroscopy before the osteotomy. The CORA location, situated around the neck of the middle phalanx, was marked on the ulnar side of the skin. A 2-mm mid-lateral incision was made at the marked location using a 367-beaver blade. We employed an electric motor-driven machine with adjustable speed (NSK Surgic Pro, NSK, IL, USA) for the osteotomy. A 12*2 mm Shannon burr was introduced beyond the skin to precisely determine the osteotomy site on the ulnar aspect of the middle phalanx’s neck, and this was confirmed with fluoroscopy. The ulnar dorsal and palmar cortex were then unilaterally cut using the burr, operating at a speed of 2500 RPM and a torque of 80 Nm (low speed, high torque) (Fig. 2).


After completing the close-wedge osteotomy (Fig. 3), a retrograde 1.2 Kirschner wire was guided through the distal interphalangeal (DIP) joint and the osteotomy site under fluoroscopic guidance, while concurrently compressing the osteotomy line. A second retrograde oblique Kirschner wire was inserted through the fracture site for rotational stability. We confirmed the intact rotational alignment of the finger through active finger flexion and extension. A volar aluminum splint was used to immobilize the DIP joints. After 4 weeks, when radiographs indicated union, the Kirschner wires were removed. Following this, patients commenced hand therapy exercises aimed at improving the ROM in all their finger joints to achieve full grip and extension. The initial follow-up radiographs after the correction revealed successful deformity correction and proper positioning of the Kirschner wires (Fig. 4).
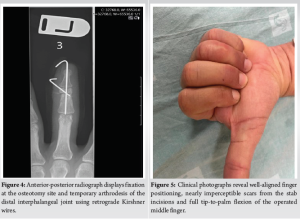
At the 1-year follow-up, subsequent radiographs indicated complete union at the osteotomy site, while physical examination demonstrated a well-aligned finger arrangement, full range of fingers motion, and barely noticeable incision scars (Fig. 5).
Posttraumatic malunion and congenital finger deformities may cause cosmetic and functional deficits including scissoring or finger deviation that can cause tendon imbalance and decreased grip strength [11]. In cases of impaired hand function, corrective osteotomy is recommended to restore anatomical alignment, with open approach being the predominant method currently employed. The complications of open osteotomy are well described. Common complications include post-operative scars, joint and tendon adhesions, damage to proximity structures such as nerves and blood vessels, delayed union due to periosteal dissection and infection [5-8]. The traditionally used osteotomes have numerous disadvantages including damage to the periosteal layer, significant heat generation that can lead to bone necrosis and can potentially damage adjacent neurovascular structures. Chisel’s disadvantages include the inability to control the extent of osteotomy, high risk of incurring adjacent fractures, possibility of tendon/ligament and neurovascular mechanical damage, and its impracticability for performing intra-articular osteotomies [12]. Minimal invasive chevron and akin osteotomy for hallux valgus correction have been developed by Walker and Redfern who described a high torque, low-speed modification of the Shannon burr to avoid the risk of skin or soft-tissue thermal damage [13]. While the benefits of this technique have already been recognized and widely used in foot reconstruction, MICO is the first surgical technique using this system in hand surgery. The authors concur that corrective osteotomy should be conducted at the fracture site in order to minimize the translation and/or angulation of the correction. Nevertheless, it is important to note that the original fracture site carries the highest risk for generating additional adhesions and potential damage to nearby structures during the dissection process. The utilization of MICO in hand surgery offers a distinct advantage. With MICO, surgeons can make minimal incisions, often as small as 2 mm. This obviates the need for extensive dissection of the surrounding tissues, thereby reducing the likelihood of additional adhesions and the potential for adjacent neurovascular injury. The selection of fixation modality remains a topic of active discussion. While certain rigid fixation methods, such as the use of plates, may enable early ROM, this approach demands a high level of technical expertise and entails soft tissue dissection. In addition, hardware removal and tenolysis are frequently required through a subsequent surgical procedure [14,15]. There is ongoing interest in the utilization of intramedullary headless compression screws for the management of phalangeal and metacarpal fractures [16]. A recent retrospective analysis, involving 20 patients who underwent corrective osteotomy using an oscillating saw alongside intramedullary headless compression screws, has demonstrated encouraging outcomes [17]. Using an intramedullary headless compression screw as fixation device offers several advantages, including the achievement of a sufficiently rigid fixation that facilitates early ROM, as well as the requirement for only a minimal incision. However, it is imperative to note potential limitations, such as the risk of articular surface damage at the insertion site and the technical complexities associated with screw removal. The consideration of headless compression screws used in MICO future cases should be judiciously made in select cases. Surgical scars have been identified as conspicuous indicators of psychological distress in patients experiencing symptoms of depression, anger, anxiety, and post-traumatic stress [18]. Therefore, the MICO surgical technique, with its scarless approach, is especially pertinent, making this procedure elegant, delicate, and well-suited for the hand’s gentle anatomy. The MICO technique offers several advantages over standard osteotomies conducted using an oscillating saw or osteotome. These advantages encompass the ability to perform a percutaneous osteotomy, minimizing harm to the periosteal layer, enhancing precision for improved osteotomy and bone alignment control, reducing stiffness and pain through a smaller surgical incision, minimizing the risk of collateral damage to nearby neurovascular structures, and lowering heat generation. We also recommend preforming this procedure under local anesthesia with the patient wide awake whenever possible to appreciate accurate rotational alignment of the operated finger throughout ROM.
MICO for hand procedures represents a straightforward, delicate, reproducible, and accessible solution for addressing malunions and congenital anomalies of the fingers. It may offer advantages by circumventing the recognized drawbacks and complications associated with an open corrective osteotomy approach. While initial outcomes of MICO show promise, a more extensive case series is required to assess the potential superiority of this technique in comparison to existing open corrective osteotomy methods.
MICO is a reproducible and accessible solution for malunions and congenital anomalies of the fingers and may avoid the known disadvantages and complications of an open approach.
References
- 1.Gollamudi S, Jones WA. Corrective osteotomy of malunited fractures of phalanges and metacarpals. J Hand Surg Br 2000;25:439-41. [Google Scholar | PubMed]
- 2.Lee SG, Jupiter JB. Phalangeal and metacarpal fractures of the hand. Hand Clin 2000;16:323-32, vii. [Google Scholar | PubMed]
- 3.Weckesser EC. Rotational osteotomy of the metacarpal for overlapping fingers. J Bone Joint Surg Am 1965;47:751-6. [Google Scholar | PubMed]
- 4.Botelheiro JC. Overlapping of fingers due to malunion of a phalanx corrected by a metacarpal rotational osteotomy--report of two cases. J Hand Surg Br 1985;10:389-90. [Google Scholar | PubMed]
- 5.van der Lei B, de Jonge J, Robinson PH, Klasen HJ. Correction osteotomies of phalanges and metacarpals for rotational and angular Malunion: A long-term follow-up and a review of the literature. J Trauma 1993;35:902-8. [Google Scholar | PubMed]
- 6.Büchler U, Gupta A, Ruf S. Corrective osteotomy for post-traumatic malunion of the phalanges in the hand. J Hand Surg Br 1996;21:33-42. [Google Scholar | PubMed]
- 7.Trumble T, Gilbert M. In situ osteotomy for extra-articular malunion of the proximal phalanx. J Hand Surg Am 1998;23:821-6. [Google Scholar | PubMed]
- 8.Jupiter JB, Goldfarb CA, Nagy L, Boyer MI. Posttraumatic reconstruction in the hand. J Bone Joint Surg Am 2007;89:428-35. [Google Scholar | PubMed]
- 9.Hoigne DJ, Stübinger S, Von Kaenel O, Shamdasani S, Hasenboehler P. Piezoelectric osteotomy in hand surgery: first experiences with a new technique. BMC Musculoskelet Disord 2006;7:36. [Google Scholar | PubMed]
- 10.Gonzalez T, Encinas R, Johns W, Benjamin Jackson J. Minimally invasive surgery using a Shannon burr for the treatment of hallux valgus deformity: A systematic review. Foot Ankle Orthop 2023;8:1-11. [Google Scholar | PubMed]
- 11.Potenza V, De Luna V, Maglione P, Garro L, Farsetti P, Caterini R. Post-traumatic malunion of the proximal phalanx of the finger. Medium-term results in 24 cases treated by “in situ” osteotomy. Open Orthop J 2012;6:468-72. [Google Scholar | PubMed]
- 12.Haider T, Geisler D, Thalhammer G, Erhart J. Multiple drill-hole osteotomy in hand surgery - description of a novel application and proof of feasibility. BMC Musculoskelet Disord 2017;18:529. [Google Scholar | PubMed]
- 13.Walker R, Redfern D. Minimally invasive hallux valgus correction: The mica technique. Orthop Proc 2012;94-B:38. [Google Scholar | PubMed]
- 14.Karthik K, Tahmassebi R, Khakha RS, Compson J. Corrective osteotomy for malunited metacarpal fractures: Long-term results of a novel technique. J Hand Surg Eur Vol 2015;40:840-5. [Google Scholar | PubMed]
- 15.Yong FC, Tan SH, Tow BP, Teoh LC. Trapezoid rotational bone graft osteotomy for metacarpal and phalangeal fracture malunion. J Hand Surg Eur Vol 2007;32:282-8. [Google Scholar | PubMed]
- 16.Hug U, Fiumedinisi F, Pallaver A, van de Wall BJ, Beeres FJ, Giesen T, et al. Intramedullary screw fixation of metacarpal and phalangeal fractures - A systematic review of 837 patients. Hand Surg Rehabil 2021;40:622-30. [Google Scholar | PubMed]
- 17.Del Piñal F, Ananos D, Rúas JS, Mazarrasa R, Studer AT. Minimally invasive procedure for correcting extra-articular malunions of metacarpals and phalanges. J Hand Surg Am 2023;48:511.e1-10. [Google Scholar | PubMed]
- 18.Ngaage M, Agius M. The psychology of scars: A mini-review. Psychiatr Danub 2018;30:633-8. [Google Scholar | PubMed]









