In the case of a large chronic Morel-Lavellée lesion, a small incisional open debridement procedure may serve as an attractive management choice. With the use of adjuncts such as drains and vacuum dressings, good short-term outcomes can be achieved as well as minimal cosmetic evidence of the scar.
Dr. Nicolas S Piuzzi, Department of Orthopaedic Surgery, Cleveland Clinic, 9500 Euclid Ave, A41, Cleveland, 44195, Ohio. E-mail: piuzzin@ccf.org
Introduction: Morel-Lavallée lesion (MLL) is a closed degloving injury that occurs after traumatic damage to soft tissue, leading to the formation of an encapsulated serosanguinous collection of fluid. Although some MLLs resolve spontaneously, chronic MLLs present with a significant risk of infection and may impede patients’ quality of life. Chronic lesions require surgical intervention to evacuate and debride the hematoma, often resulting in severe cosmetic damage postoperatively.
Case Report: We documented a large 19.4 cm × 4.2 cm × 15.10 cm MLL on the right lateral hip that presented a significant impediment to the patient’s daily functions. After the failure of conservative management, the patient was treated surgically through a minimal incision debridement procedure, utilizing a wound drain and vacuum-assisted compressional dressing upon closure. Excellent 1-year post-operative outcomes were achieved with no recurrence of the lesion and limited cosmetic evidence of the MLL.
Conclusion: This case highlights the value of a limited incisional debridement procedure for the management of a chronic Morel-Lavellée lesion. When using this technique, surgeons can effectively treat these lesions with promising short-term outcomes and minimal wound scarring.
Keywords: Morel-Lavallée lesion, chronic, minimal scarring, surgical management.
Morel-Lavellée lesions (MLLs) are closed degloving injuries initiated from a shearing force that separates the skin, subcutaneous fat, and superficial fascia from the deep fascia and underlying muscles, thus creating a potential cavity [1-3]. This mechanical separation, combined with the initial traumatic injury, damages blood and lymphatic vessels, which results in serosanguinous drainage into the cavity [1,2]. MLLs can be differentiated based on time. Acutely, seroma formation occurs, resulting in a homogenous serous/lymphatic collection of fluid (type I MLL). Subacutely, fat globules, blood products, and internal septation are observed in the hematoma (type II MLL). Chronically, the formation of a fibrotic capsule around the lesion that impairs drainage may occur, resulting in a hematoma with necrotic tissue, granulation tissue, fibrin, and blood clots (type III MLL) [1,3]. Risk factors include motor vehicle accidents, falls, and injuries from high-impact sports such as football [4]. Most frequently, these lesions are found overlying the greater trochanter of the femur in the anterolateral thigh and present as enlarging, tender lesions with associated pain and tightness [1,5,6]. MLLs are often missed if not associated with underlying fractures, contributing to their progression to chronicity. Overall, they remain a rare condition, with reported incidence around 8.3% in pelvic trauma and 1.7% in acetabular fractures requiring emergency care [7,8]. Their infrequency has hindered the establishment of formal treatment guidelines. However, despite their rarity, chronic lesions warrant expedited management. The large static fluid collections pose risk of infection, negatively impact quality of life, and may cause long-term morbidity if left untreated [6]. Increased awareness and reporting of techniques and outcomes are needed to define best practices for this uncommon but potentially serious traumatic injury. Here, we present a case of chronic MLL managed with a small single longitudinal incisional debridement procedure to ensure minimal cosmetic scarring.
A 64-year-old male with a history of a traumatic fall on his right side presents with a large mass and associated pain in his right hip.
History
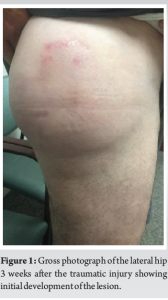
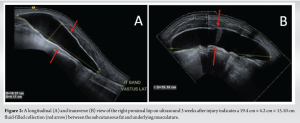
The patient initially presented to our outpatient orthopedic clinic with complaints of a large mass on the right lateral hip. He confirmed a traumatic fall down seven stairs, 6 weeks prior. Immediately after the fall, he was assessed in the emergency department, but with no signs of a mass on the hip or any other complications at that time, he was discharged home. However, 10 days later, the patient started to develop a swelling on his right hip which gradually increased in size to around 20 × 15 cm (Fig. 1). He presented to our outpatient clinic reporting continuous mild aching pain in the right hip which started at the same time as the onset of the mass. There was no associated fever, chills, numbness, or instability present. On physical examination, mild tenderness was present upon palpation of the mass with no erythema. The patient exhibited full range of motion and strength on the right hip. Gait was found to be stable without assistance with a negative Trendelenburg sign. Hip X-rays showed no evidence of fracture to the femur or pelvis and blood tests did not suggest any infective causes. Preliminary ultrasound images indicated a compressible serosanguinous fluid-filled cavity in between the superficial and deep fascial layers of the lateral hip of approximately 19.4 cm × 4.2 cm × 15.10 cm in dimension (Fig. 2). The mode of injury, imaging, and patient history were consistent with an MLL. Through shared decision-making, an initial conservative management approach of elastic bandaging with adequate compression to allow the MLL to resolve spontaneously was agreed upon.
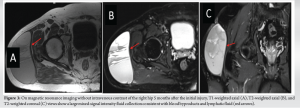
The patient returned to our clinic 3 months later with complaints of significant worsening in right hip pain and impaired daily activities such as putting on pants due to the mass. Subsequent MRI studies of the right hip confirmed the presence of a 13.6 cm × 7.3 cm × 15.3 cm chronic MLL (Fig. 3). Due to failed conservative management and a progression in pain and loss of function, the decision was made for surgical intervention.
Operation
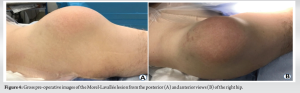
Our patient underwent surgical debridement under general anesthesia for his chronic MLL. Having been positioned in the left lateral decubitus, the right leg was draped and prepared in the usual sterile fashion (Fig. 4). Exposure to the right hip was gained through a limited 6 cm incision along the distal aspect of the MLL. The capsule containing serosanguinous fluid was carefully resected with no signs of bacterial infiltration, and subsequently, the cavity was thoroughly irrigated with 5 L of saline and 2 g of vancomycin powder were placed in the wound. The surgical incision was then sutured closed with a Hemovac drain emplaced in the wound over the tensor fascia. An incisional vacuum-assisted compression dressing (Prevena vacuum-assisted closure) was placed on top. Bacterial cultures obtained during surgery were negative and thus did not warrant changes to standard antibiotic prophylaxis. Patient was instructed to weight bear as tolerated.
Follow-up
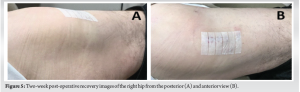
2 weeks post-operatively, the drain was removed, and the patient exhibited limited tissue scarring from the procedure with no signs of tissue necrosis or infection (Fig. 5). At 1-year follow-up, he reported no pain and no activity limitations.
Chronic MLLs represent a rare but potentially serious complication following traumatic injury. Despite their low incidence, prompt diagnosis and management are crucial as large, unresolved lesions carry a high risk of delayed wound healing, infection, and long-term functional impairment. However, at present, no established treatment algorithm exists to guide clinical decision-making. Conservative approaches such as compression wraps and needle aspiration may be appropriate for small acute lesions, but large chronic collections often require more aggressive intervention. In this case report, we describe our experience of successfully managing a chronic MLL with open surgical debridement. Our minimal incision technique allowed for lesion evacuation and capsule resection while limiting cosmetic damage. The addition of quilting sutures, irrigation, intra-wound antibiotics, a Hemovac drain, and vacuum-assisted dressing helped prevent recurrence and optimize recovery. While further studies are needed, this case highlights the potential value of surgical debridement in treating problematic chronic MLLs. Our initial conservative management with compression wraps was reasonable given the patient’s minimal symptoms early on. However, conservative therapies such as aspiration, wraps, and cryotherapy have limited efficacy for large, chronic MLLs [9]. As these lesions persist unresolved over time, they have a high incidence of delayed wound healing, tissue necrosis, and bacterial colonization [2,3]. A review by Hak et al. [10] found nearly 50% of surgically treated lesions already exhibited infection. More aggressive surgical options are often necessary in these cases, including debridement, drainage, sclerodesis, and resection [2,3,11,12]. A systematic review by Shen et al. demonstrated improved resolution with surgical techniques compared to conservative measures alone [12]. Although no singular gold standard approach exists, local debridement with drainage was the most common and effective intervention. Regardless of technique, expedited surgical management is critical for chronic, high volume lesions to enable healing and prevent further complications such as necrosis and colonization. While reasonable initially, conservative therapies proved ineffective for our patient, requiring the transition to successful surgical treatment. Clinical guidelines for the treatment of MLLs are limited, but Singh et al. [6] proposed an algorithm suggesting open drainage for large chronic lesions with intact overlying skin, as in our case. Wide debridement incisions often lead to disfiguring scars, so adjunct techniques to limit scarring are recommended [6,13]. Quilting sutures can promote drainage while minimizing dead space [6,13]. Curettage and irrigation remove debris and lower infection risk. Low-suction drains can also enhance evacuation and prevent recurrent fluid build-up [6,13]. Although effective for treatment, large open incisions result in considerable scarring and cosmetic damage. However, as seen in our case, small limited incisions for debridement can yield similar success with less scarring [2]. These minor incisions have better cosmetic outcomes that are more acceptable to patients, improving satisfaction. Our minimal incision technique, with adjuncts like intraoperative antibiotics, quilting sutures, and a Hemovac drain, allowed adequate lesion drainage and capsule removal while optimizing cosmesis. Further study on minimal incision techniques is warranted to establish standardized guidelines.
We present a case of successful surgical management of a chronic MLL using a limited incisional approach. While these lesions are rare, large chronic collections can lead to pain, functional impairment, and risk of infection if left unresolved. Our technique of a small longitudinal debridement incision enabled adequate evacuation and capsule resection while minimizing cosmetic damage. The addition of quilting sutures, antibiotic irrigation, a drain, and vacuum-assisted dressing likely contributed to the excellent outcomes of healed wound and full return of function at 1 year with minimal scarring. While there are no established guidelines, this case highlights the potential for minimal incision techniques to balance optimal lesion resolution and tissue preservation in the management of problematic chronic MLLs. Further study of outcomes using small incisional approaches is warranted.
The presented case underscores the significant role of a limited incisional debridement procedure for the management of a chronic MLL. Utilizing a wound drain and vacuum-assisted incisional dressing, surgeons can effectively treat these lesions with promising 1-year outcomes and minimal wound scarring.
References
- 1.Bonilla-Yoon I, Masih S, Patel DB, White EA, Levine BD, Chow K, et al. The Morel-Lavallée lesion: Pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol 2014;21:35-43. [Google Scholar | PubMed]
- 2.Scolaro JA, Chao T, Zamorano DP. The Morel-Lavallée lesion: Diagnosis and management. J Am Acad Orthop Surg 2016;24:667-72. [Google Scholar | PubMed]
- 3.Nickerson TP, Zielinski MD, Jenkins DH, Schiller HJ. The mayo clinic experience with Morel-Lavallée lesions: Establishment of a practice management guideline. J Trauma Acute Care Surg 2014;76:493-7. [Google Scholar | PubMed]
- 4.Mettu R, Surath HV, Chayam HR, Surath A. Chronic Morel-Lavallée lesion: A novel minimally invasive method of treatment. Wounds 2016;28:404-7. [Google Scholar | PubMed]
- 5.Nair AV, Nazar P, Sekhar R, Ramachandran P, Moorthy S. Morel-lavallée lesion: A closed degloving injury that requires real attention. Indian J Radiol Imaging 2014;24:288-90. [Google Scholar | PubMed]
- 6.Singh R, Rymer B, Youssef B, Lim J. The Morel-Lavallée lesion and its management: A review of the literature. J Orthop 2018;15:917-21. [Google Scholar | PubMed]
- 7.Judet R, Judet J, Letournel E. Fractures of the acetabulum: Classification and surgical approaches for open reduction: Preliminary report. J Bone Joint Surg Am 1964;46:1615-46. [Google Scholar | PubMed]
- 8.Tseng S, Tornetta P 3rd. Percutaneous management of Morel-Lavallee lesions. J Bone Joint Surg Am 2006;88:92-6. [Google Scholar | PubMed]
- 9.Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: Twenty-seven cases in the national football league. Am J Sports Med 2007;35:1162-7. [Google Scholar | PubMed]
- 10.Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: The Morel-Lavallée lesion. J Trauma 1997;42:1046-51. [Google Scholar | PubMed]
- 11.Greenhill D, Haydel C, Rehman S. Management of the Morel-Lavallée lesion. Orthop Clin North Am 2016;47:115-25. [Google Scholar | PubMed]
- 12.Shen C, Peng JP, Chen XD. Efficacy of treatment in peri-pelvic Morel-Lavallee lesion: A systematic review of the literature. Arch Orthop Trauma Surg 2013;133:635-40. [Google Scholar | PubMed]
- 13.Jones RM, Hart AM. Surgical treatment of a Morel-Lavallée lesion of the distal thigh with the use of lymphatic mapping and fibrin sealant. J Plast Reconstr Aesthet Surg 2012;65:1589-91. [Google Scholar | PubMed]