Orthopaedic surgeons play a critical role in ensuring medical device safety by actively participating in materiovigilance. Understanding the importance of identifying, reporting, and analyzing adverse events can significantly improve patient outcomes, refine device design, and elevate the standard of orthopaedic care in India.
Dr. Sachin Kale, Consultant Orthopaedic Surgeon, Apollo Hospital, Belapur, Navi Mumbai, Maharashtra, India. Professor Orthopaedics, Dr D Y Patil School of Medicine, Nerul, Navi Mumbai, Maharashtra, India. E-mail: sachinkale@gmail.com
Abstract: Advanced medical devices serve an important role in modern medicine, particularly in orthopaedics, by improving patients’ mobility and quality of life. However, the intricacy of devices such as joint replacements and spine implants raises hazards such as mechanical failures and biocompatibility difficulties. Materiovigilance, notably through India’s Materiovigilance Programme of India, is critical for detecting and treating adverse events, hence assuring device safety and efficacy. Despite its relevance, hurdles such as a lack of understanding and reporting issues impede implementation. Strengthening materiovigilance through education, simplified reporting, and a supportive culture may spur innovation, enhance patient outcomes, and position India as a worldwide leader in medical device optimization.
Keywords: Materiovigilance, orthopaedics, medical devices, patient safety.
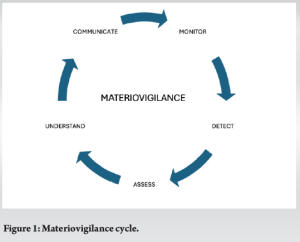
In the rapidly evolving field of modern medicine, the use of advanced medical devices has become indispensable, especially in orthopaedics. The mobility and quality of life of patients have been greatly enhanced by contemporary orthopaedic implants, including as total hip replacement (THR), total knee replacement, spine implants, etc. These devices symbolize the confluence of engineering and medicine, creating unprecedented opportunities for patient care. These implants and devices sometimes stay in a patient’s body for their lifetime. However, their growing complexity also poses significant challenges, particularly regarding patient safety and device reliability. The adverse effects stemming from device malfunctions can range from mild discomfort to severe complications such as infections, disability, or the need for revision surgeries. These risks underscore the critical importance of materiovigilance — a systematic approach to monitoring, evaluating, and addressing adverse events associated with medical devices. While materiovigilance keeps an eye on the functionality and safety of medical devices, pharmacovigilance guarantees the safety of pharmaceuticals. The Materiovigilance Programme of India (MvPI), launched in 2015, offers a framework for healthcare professionals to actively contribute to the safety and efficacy of medical devices. This article delves into the vital role materiovigilance plays in orthopedics, the barriers hindering its adoption, and actionable strategies for strengthening its implementation. (Fig. 1)
With millions of orthopaedic surgery and a population of 1.4 billion, India presents a special opportunity for materiovigilance. India has access to a large collection of data on patient outcomes and implant performance, which it can use to find trends, spot problems, and enhance implant quality and design. India may end up leading the world in medical device optimization, providing safer, more efficient orthopaedic solutions, and fostering innovation as a result. Orthopaedic surgery is unique in its reliance on medical devices that are often implanted within the human body for extended periods. Devices such as joint replacements, screws, plates, and external fixators are subjected to constant biomechanical stresses, making them susceptible to wear, tear, and, occasionally, failure. (Fig. 2)

The inherent complexity of these devices introduces several risks:
- Mechanical failures: Issues such as implant loosening, breakage, or wear are common, especially in joint replacements where components interact under high loads
- Material degradation: Corrosion or degradation of device materials, such as metal-on-metal implants, can lead to systemic effects like metallosis or local tissue damage
- Biocompatibility issues: Some devices elicit adverse immune responses, resulting in inflammation or rejection
- Human error and surgical factors: Incorrect implantation techniques or intraoperative mishandling can also compromise device functionality.
These risks are magnified in orthopedics due to the critical role these devices play in patient mobility and overall quality of life. Failures not only result in physical harm but also carry significant emotional and financial consequences for patients and healthcare systems.
Materiovigilance addresses these risks by enabling the systematic collection and analysis of data on adverse events. Through reports submitted by orthopaedic surgeons and other healthcare professionals, the MvPI:
- Identifies patterns of device-related complications
- Alerts regulators, manufacturers, and clinicians to emerging safety concerns
- Facilitates design modifications to improve device safety and efficacy
- Establishes evidence-based guidelines for device use and surgical procedures.
A prime example of how material vigilance aids in implant improvement is the use of ceramic bearing designs with highly cross-linked polyethylene in THR. Metal-on-metal hip implants have been recalled and redesigned as a result of the outstanding performance of Materialovigilance in improving orthopaedic implants. Reports of negative consequences, such as metallosis, brought attention to the need for improved designs and materials. Recalls and more stringent monitoring procedures resulted from the Food and Drug Administration and Medicines and healthcare Healthcare Products regulatory agency’s response. Alternative materials, such as ceramic and highly cross-linked polyethylene, were created by manufacturers to lessen articulating surface wear. This improved implant safety and longevity, reduced problems, and ultimately improved patient results and faith in orthopedic surgery. The ultimate goal of materiovigilance is to create a feedback loop that continuously refines medical devices and improves patient outcomes. Materiovigilance in medical devices is similar to the art of sculpting, in which little, precise strikes with a chisel polish a stone into a flawless figure. Each report, inquiry, and remedial action smoothes out faults, improving the safety and performance in medical devices.
Orthopaedic innovations include newer materials such as carbon fiber implants for fixing metastatic spines, flexible rods for junctional spinal failures, newer technologies such as robotic-assisted instruments for total joint replacements, and newer designs like the femoral neck system for treating femoral neck fractures. Although these technologies show promise in terms of better results and increased accuracy, their long-term dependability and reproducibility have not been established. For orthopaedic surgeons to track performance in the real world, identify any problems, and improve designs, materiovigilance is therefore crucial.
- Reporting adverse events: Surgeons can identify and document device-related complications, providing valuable data to the MvPI
- Collaborative investigations: By engaging with manufacturers and regulators, surgeons can help identify the root causes of device failures
- Shaping device design: Feedback from surgeons has historically led to design innovations, such as improved implant materials or changes in device geometry to enhance durability and compatibility.
Reporting in materiovigilance is analogous to voting in politics: Each report may appear insignificant on its own, but when combined, they have enormous influence. When many reports identify similar vulnerabilities, it leads to substantial improvements in device safety and regulations.
Hence growing awareness is of utmost importance. Despite their pivotal role, many orthopedic surgeons in India do not actively participate in materiovigilance due to several barriers:
- Lack of awareness: Many are unaware of the MvPI or its processes
- Misconceptions about reporting: There is a widespread belief that reporting adverse events could lead to legal or professional repercussions
- Time constraints: Busy clinical schedules often leave little room for administrative tasks like adverse event reporting
- Inadequate training: Few surgeons receive formal instruction on identifying and reporting adverse device events.
These challenges highlight the need for systemic efforts to empower surgeons to embrace materiovigilance as an integral part of their practice.
The MvPI has laid the groundwork for effective materiovigilance but its implementation in the orthopedic community faces significant obstacles. Addressing these barriers is critical for maximizing the program’s impact.
Many healthcare professionals remain unaware of materiovigilance initiatives. Even among those familiar with the program, there is confusion about how to report adverse events. The absence of streamlined reporting tools further exacerbates this issue.
In a healthcare environment where adverse event reporting is often stigmatized, many surgeons fear being blamed or held liable for complications. This culture discourages open reporting and transparency, hindering the collection of meaningful data.
Orthopaedic surgeons often work in resource-constrained settings where time, personnel, and administrative support are limited. These constraints make it difficult to prioritize materiovigilance over clinical duties.
Few medical institutions incorporate materiovigilance training into their curricula. As a result, even experienced surgeons may lack the knowledge needed to identify and report adverse device events effectively.
Overcoming these barriers requires a concerted effort by healthcare institutions, regulatory bodies, and professional organizations. Key strategies include:
Educational campaigns
- Workshops and seminars: Regular training sessions can demystify the reporting process and emphasize its importance
- CME programs: Including materiovigilance as a topic in continuing medical education programs ensures ongoing professional development
- Public awareness drives: Informing patients about the importance of materiovigilance can also encourage them to report device-related complications.
Simplifying reporting
- Digital platforms: User-friendly mobile apps and online portals can streamline the reporting process, making it faster and more accessible
- Integration with electronic health records (EHRs): Embedding reporting tools within EHR systems can simplify data collection and submission.
Encouraging a supportive culture
- Non-punitive reporting: Establishing policies that prioritize learning and improvement over blame can encourage participation
- Recognition programs: Acknowledging and rewarding surgeons who actively contribute to materiovigilance can motivate others to follow suit.
Collaborative approaches
- Interdisciplinary collaboration: Engaging engineers, regulators, and researchers alongside surgeons can improve the analysis of adverse events
- Global benchmarks: Learning from successful materiovigilance programs in other countries can help refine India’s approach.
The MvPI has the potential to revolutionize orthopaedic care by ensuring the safety and efficacy of medical devices. However, its success depends on the active participation of orthopedic surgeons. By embracing materiovigilance, surgeons can:
- Safeguard their patients from preventable complications
- Drive continuous improvements in device design and usage
- Contribute to a national database that enhances the quality of care across the healthcare system.
As medical devices become increasingly sophisticated, the need for robust monitoring systems will only grow. Orthopaedic surgeons must recognize their role as stewards of patient safety and champions of materiovigilance. Through collaboration, education, and a shared commitment to excellence, the orthopedic community can lead the way in building a safer, more reliable future for healthcare.









