The importance of classifying post-traumatic elbow stiffness preoperatively to guide treatment and the need for Open arthrolysis is emphasized for cases of intra-articular stiffness, where severe adhesions or joint deformities are present. This procedure allows direct access to remove obstructive tissue, improving mobility when other treatments fail.
Dr. Tarun Prashanth K R, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai - 600 116, Tamil Nadu, India. E-mail: tarun10007@gmail.com
Introduction: Elbow stiffness can be a debilitating condition that significantly impacts a individual’s ability to perform activities of daily living (ADL). Neglected distal humerus fractures when left untreated result in malunion causing the elbow joint to undergo arthrofibrosis with capsular contracture with interspersed osteophytes and formation of loose bodies. The elbow joint is particularly susceptible to stiffness due to its highly congruent bony anatomy, relatively confined joint space tightly stabilizing collateral ligament complex, and the close relationship of the surrounding muscles acting as secondary stabilizers.
Case Report: A 31-year-old man presented to the OPD 5 months after injury following 3 cycles of native splinting for distal humerus fracture. He had severe painful restriction of movements, with diffuse tenderness and deformity over the elbow joint affecting his ADL. He underwent a left elbow manipulation under anaesthesia after capsular release.
Discussion: Late presentation of distal humerus intra-articular comminuted fracture which has undergone mal-union can present with gross elbow stiffness commonly. Moreover, if the fracture was treated with native splinting or prolonged immobilisation it is prone for stiffness and other complications. Open approach confers additional advantage of addressing the bony hindrance in addition to soft-tissue release.
Conclusion: The clinical decision of choosing open approach versus arthroscopic approach is determined by the severity of the stiffness. In our case, since the patient has severe stiffness with only 30° arc of motion, we decided to go ahead with an open arthrolysis and the patient had good functional improvement.
Keywords: Stiff elbow, stiffness, post traumatic elbow stiffness, arthrolysis, open arthrolysis, arthroscopic arthrolysis, classification of stiff elbow
Elbow joint is a functionally very demanding joint which helps in performing various activities of daily living (ADL) and any condition which is going to predispose the elbow joint to stiffness will cause debilitating results in the patient. Morrey et al. [1] found the functional arc of elbow motion during activities of daily living to be 100° for both flexion–extension (30°–130°) and pronation–supination 50° in either direction. Stiffness is common in elbow due to the congruity of the joint, the close muscular proximity of brachialis and triceps tendons, and the tendency to develop heterotrophic ossification (HO). Posttraumatic stiffness occurs as a result of four stages: bleeding, edema, granulation, and fibrosis [2]. The resulting elbow stiffness can be mild or severe and may be extremely difficult for the patient because of pain and resultant limitations in ADL [3,4]. The complexity of choosing arthrolysis either arthroscopic or open and which approach depends on arriving at an etiology, choosing the correct surgery and rehabilitation can be a cumbersome procedure for both the patient and the surgeon.
A 31-year-old man a daily laborer by occupation with right dominant upper extremity, presented to the OPD 5 months following a road traffic accident with complaints of deformity and painful restriction of movements of his left elbow for the past 2 months. He gave a history of road traffic accident 5 months back and sustained isolated injury to his left elbow for which he underwent native splinting of the elbow for 60 days consisting of four cycles, 15 days each. Following the removal of the splint, he was asked to mobilise his elbow without any supervised physio protocol. He presented with inability to flex or extend his elbow beyond a certain degree, with significant functional limitation. The meagre movements which were present were also painful and he was unable to return to work. On examination, diffuse swelling was present over the left elbow joint with obliteration of the anconeus triangle. No scars, ulcerations, or dilated veins were visible. On palpation, no warmth was present. Diffuse tenderness was present over the elbow joint. The elbow joint was fixed in 60° of flexion (Fig. 3), and further extension was not possible. Flexion up to 90° was possible, and attempting further was painful and restricted. There was no restriction of supination (Fig. 2) and pronation (Fig. 1). Distal neuromuscular status of the left upper limb was normal.

Orthogonal radiograph of left elbow joint (Fig. 4) with AP and lateral views was taken, and it showed a malunited comminuted intra-articular fracture of distal humerus with multiple osteophytes around and inside the elbow joint and mild arthritic changes in the distal humerus. Heterotrophic ossificans seen in the olecranon fossa with specs of calcification visualized anteriorly over the region brachialis distally above the coronoid process of the olecranon.

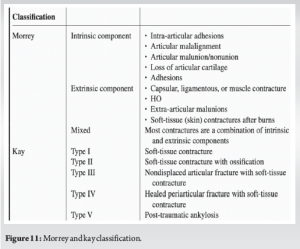
He was admitted, and all routine blood investigations were done. The radiograph (Fig. 4) showed an acceptable articular congruity with some osteophytes and diffuse osteopenic changes noted most probably caused being immobilzation posttrauma. The blood parameters were normal, and inflammatory markers were also not elevated. CT elbow with 3D reconstruction confirmed the same findings noticed in the radiographs. Following the interpretation of all findings with a history of immobilization for a prolonged period, it was imperative that the elbow fixed flexion deformity and stiffness could be a result of soft-tissue contracture associated with intraarticular adhesions possibly heterotrophic ossificans. The patient was diagnosed as mixed contracture under Morrey anatomical classification and Type 3 under Kay classification of elbow stiffness. The patient was planned for release of soft-tissue contracture and removal of heterotrophic ossificans through open arthrolysis, resection of intraarticular ossificans and soft-tissue release combined with manipulation under anesthesia. Under general anesthesia, patient in supine position and left upper limb on hand table with shoulder in 90° of abduction with a rolled towel underneath the elbow to elevate and give an additional valgus force to the joint, the elbow joint was initially assessed through a range of movement after muscle relaxation under anaesthesia and yielded to further flexion until 100° following which , elbow joint was accessed using lateral column approach. Skin and soft tissues dissected and lateral epicondyle identified and through the plane between extensor digitorum communis and extensor carpi radialis brevis (Fig. 5), elbow joint capsule was visualised and found to be contracted severely. Anterior and posterior parts of the capsule was released and osteophytes were removed using a mini osteotome and rongeurs from the olecranon fossa. Serial assessment was done after the intra-articular adhesion releases and following removal of loose bodies from the joint. The integrity of LCL and MCL was observed. The need for a medial approach if needed was also taken into consideration in case of instability. At the end of the procedure, the elbow joint was manipulated throughout the full possible range of movements and flexion of 160° (Fig. 6) and near normal extension (Fig. 7) was attained. The surgical wound was closed and the sterile dressing was done and a dorsal slab applied in extension.


The immediate post-operative period was uneventful and was started on active left elbow mobilisation exercises on POD 1. Prophylaxis for the prevention of HO was started Indomethacin 25 mg for 3 weeks. Post-operative radiograph was taken and was satisfactory (Fig. 10). Sutures were removed on POD 14 and surgical site wound recovery was uneventful.

He was on regular follow-up and he was reviewed recently at 6 months’ follow-up where his painfree range of motion was recorded and was found to be around 130° with a fixed flexion deformity of 10° (Fig. 8) and flexion of around 140° (Fig. 9). He is able to do his day to day activities with ease and has good Quality of Life (QoL) post the procedure evident with excellent MEPS score.
Elbow joint is an important joint of the upper limb that is instrumental in carrying out several day to day activities [1]. A stiff elbow following trauma can be due to a variety of causes [4]. A functional elbow joint is essential for good QoL for the individual. A range of motion of atleast 30°–130° [5] has been deemed to essential for the proper functionality of the joint in making day to day activities possible. Initially, it was around 100° of flexion, but due to the significance given to the usage of mobile phones, now a flexion of 130° [5] has been deemed as functional. Many classifications systems [6] have been in use for classifying the elbow stiffness, discern the etiology, forecast the porbable prognosis and arrive at a decision for mode of management .We classified using the Morrey [7] and Kay’s classification (Fig. 11) accordingly with mixed in Morrey’s classification and Type 4 in Kay’s classification.
Watts and Bains [6] modified Morrey’s classification system in which they proposed capsular causes for elbow stiffness as an isolated etiology and included neurological etiology as a separate group thus classifying all causes of elbow stiffness not only the post-traumatic ones. Hence their classification system included (1) Extra-articular, (2) Intra-articular, (3) Capsular, (4) Neurological.
Another classification system is the S.T.I.F -Stiffness types and influencing factors [6] developed by Shawn O’ Driscoll which describes the 5 common etiologies causing stiffness as well as the 6 influencing factors that often effect the treatment and clinical outcome which also gives useful information regarding the probable pathogenesis and deciding on the management and approach.
We decided to go ahead with an open arthrolysis [8] of the left elbow and went ahead with a Kaplan’s approach through the plane between Extensor digiorum communis and Extensor carpi radialis brevis. After exposing the elbow joint, we partly excised the contracted capsule and released the anterior and posterior parts of the remaining contracted capsule [9]. Intra-articular osteophytes were also removed and thorough manipulation was done [3].
The decision to proceed with open approach as against an arthroscopic arthrolysis was made because of the combination of bony and soft-tissue pathology in the elbow joint. As evident from the literature [5], the access to the elbow joint in a stiff elbow arthroscopically is very difficult and also carries the risk of iatrogenic nerve injury due to the close proximity of ulnar nerve. Furthermore, open approach had better results postoperatively if the flexion arc is less than 90° and in long standing flexion contractures.
Arthroscopic arthrolysis has been resorted to as the management in refractory elbow stiffness to physical therapy, when the restriction of movements [10] is less. The results after arthroscopic arthrolysis for severe elbow stiffness, with flexion arc <80°, bony anomalies, previous surgical history including history of ulnar nerve transposition are poor [11].
Kruse et al. proposed lateral access associated with posterior mini-open access. At an average follow-up of 38 months, all patients had displayed improvements. The average ROM during flexion improved from 99° pre-operative to 128° at the final follow-up in the post-traumatic rigid elbow, and from 98° to 126° in the rigid degenerative elbow. Similarly, the extension improved from an average of 52°–19° in the post-traumatic group, and from 41° to 17° in the degenerative stiffness group. The average gain in both groups was 57° in flexion-extension [12].
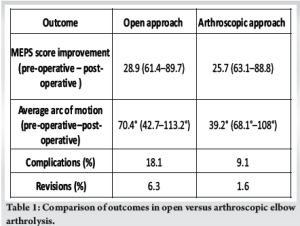
Table 1 shows the comparison of the outcomes of the stiff elbow treated via open vs arthroscopic approach as discussed by Siemensma et al. [5]. Thus, the improvement in MEPS (Mayo Elbow performance Score) score and improvement in range of motion was higher in open approach compared with arthroscopic approach.
Lanzerath et al. [9] through their extensive systematic review compared the functional outcomes in the form of improvement in MEPS score , the complication rates amongst open vs arthroscopic arthrolysis by reviewing around 27 stduies including 1666 patients . In their study they showed that the results were satisfactory in both arthroscopic and open approach cohorts, with a slight superior MEPS (mayo Elbow performance Score) in the arthroscopic cohort and reduced complication and revision rates, while imporved range of motion was seen in the open approach cohort.
Other treatment options include interposition arthroplasty with external fixator in young individuals, Total elbow Arthroplasty in elderly individuals [5]. Kodde et al. conducted a study [13] where the improvement in range of motion was highest in arthrolysis with external fixator followed by arthroplasty, open arthrolysis, and finally arthroscopic arthrolysis. Because of the poor functional performance and higher complication rates, arthroplasty and arthrolysis using external fixators have been rarely employed.
It was also noted that initiating CPM [5,8] (continuous passive motion) postoperatively gave better results as compared to physiotherapy. He was started on elbow mobilization exercises from post-operative day 1 and has been continuously performing elbow ROM exercises. He was reviewed recently at 3 months’ post-operative period and has regained a flexion of 140° and extension of +10° and is able to carry out his daily activities with ease with good QoL indicators and without pain.
Hence, deciding on a management is challenging but quintessential in providing the patient with a functional elbow joint with good range of motion arc in performing his day-to-day activities. With further advancements in artificial intelligence [14] and higher imaging, the future has scope for further development in this respect and aiding the patient with faster recovery and less morbidity.
Post-traumatic tiff elbow can be a debilitating hazard for the patient in performing ADL and greatly affects his/her QoL. Thus , determining the cause and choosing an appropriate management for the stiff elbow is quintessential. The clinical decision of choosing open approach versus arthroscopic approach is determined by the severity of the stiffness, the etiology, the needs of the patient, the range of motion at presentation and a consensus has to be arrived at after explaining to the patient the benefits and shortcomings of both the approaches. In our case, since the patient has severe stiffness with only 30° arc of motion we decided to go ahead with an open arthrolysis and the patient had good functional improvement.
This article aims at proving the significance of classifying the post-traumatic elbow stiffness, the severity of the post-traumatic elbow stiffness and catering a suitable surgical approach depending on the same.
References
- 1.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 1981;63:872-7. [Google Scholar | PubMed]
- 2.Adolfsson L. Post-traumatic stiff elbow. EFORT Open Rev 2018;3:210-6. [Google Scholar | PubMed]
- 3.Vardakas DG, Varitimidis SE, Goebel F, Vogt MT, Sotereanos DG. Evaluating and treating the stiff elbow. Hand Clin 2002;18:77-85, vi. [Google Scholar | PubMed]
- 4.Myden C, Hildebrand K. Elbow joint contracture after traumatic injury. J Shoulder Elbow Surg 2011;20:39-44. [Google Scholar | PubMed]
- 5.Siemensma MF, van der Windt AE, van Es EM, Colaris JW, Eygendaal D. Management of the stiff elbow: A literature review. EFORT Open Rev 2023;8:351-60. [Google Scholar | PubMed]
- 6.Marinelli A, Guerra E, Bain G. Classification of elbow stiffness. J ISAKOS 2024;9:234-9. [Google Scholar | PubMed]
- 7.Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am 1990;72:601-18. [Google Scholar | PubMed]
- 8.Masci G, Cazzato G, Milano G, Ciolli G, Malerba G, Perisano C, et al. The stiff elbow: Current concepts. Orthop Rev (Pavia) 2020;12:8661. [Google Scholar | PubMed]
- 9.Lanzerath F, Wegmann K, Hackl M, Uschok S, Ott N, Müller LP, et al. Surgical arthrolysis of the stiff elbow: A systematic review. Arch Orthop Trauma Surg 2023;143:2383-93. [Google Scholar | PubMed]
- 10.Willinger L, Siebenlist S, Lenich A, Liska F, Imhoff AB, Achtnich A. Arthroscopic arthrolysis provides good clinical outcome in post-traumatic and degenerative elbow stiffness. Knee Surg Sports Traumatol Arthrosc 2018;26:312-7. [Google Scholar | PubMed]
- 11.Pederzini LA, Nicoletta F, Tosi M, Prandini M, Tripoli E, Cossio A. Elbow arthroscopy in stiff elbow. Knee Surg Sports Traumatol Arthrosc 2014;22:467-73. [Google Scholar | PubMed]
- 12.Kruse KK, Papatheodorou LK, Weiser RW, Sotereanos DG. Release of the stiff elbow with mini-open technique. J Shoulder Elbow Surg 2016;25:355-61. [Google Scholar | PubMed]
- 13.Kodde IF, van Rijn J, van den Bekerom MP, Eygendaal D. Surgical treatment of post-traumatic elbow stiffness: A systematic review. J Shoulder Elbow Surg 2013;22:574-80. [Google Scholar | PubMed]
- 14.Bartlett J, Kazzazi F, To K, Lawrence J, Khanduja V. Virtual reality simulator use stimulates medical students’ interest in orthopaedic surgery. Arthrosc Sports Med Rehabil 2021;3:e1343-8. [Google Scholar | PubMed]










