The on-track/off-track concept helps guide management in recurrent shoulder instability, allowing tailored treatment based on bone loss and Hill-Sachs engagement. Arthroscopic Bankart repair with remplissage is effective for non-engaging Hill-Sachs lesions with minimal glenoid bone loss.
Dr. P M Mervin Rosario, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai-600044, Tamil Nadu, India. E-mail: mervinrosario45@gmail.com
Introduction: Recurrent anterior shoulder dislocation is a common sequela of traumatic shoulder injury in young adults, particularly athletes. Delayed treatment often leads to complex pathoanatomy, including Bankart and Hill-Sachs lesions. The combination of arthroscopic Bankart repair and remplissage has become a reliable solution in selected patients.
Case Report: We present the case of a 36-year-old male with a 14-year history of recurrent anterior shoulder dislocations, initially sustained during sports activity. Despite frequent episodes, all were self-managed without medical attention. Radiological evaluation revealed a Bankart lesion, on-track Hill-Sachs defect, and minimal glenoid bone loss. The patient underwent arthroscopic Bankart repair with remplissage. Post-operative recovery was uneventful, with satisfactory stabilization.
Conclusion: This case highlights the importance of comprehensive clinical and radiological assessment in chronic shoulder instability. Arthroscopic intervention combining Bankart repair and remplissage offers effective management in patients with minimal bone loss and non-engaging Hill-Sachs lesions.
Keywords: Recurrent shoulder dislocation, On track Hill-Sachs lesion, Bankart’s repair, shoulder arthroscopy, remplissage.
The shoulder joint, while being the most mobile joint in the human body, is also one of the least stable. This remarkable range of motion makes it particularly prone to dislocation, especially during high-impact sports or trauma. Among these, anterior shoulder dislocation is the most common type and frequently occurs in young, active individuals [1]. Initial dislocation events often result in damage to the soft-tissue stabilizers – most notably, the anteroinferior labrum, causing a Bankart lesion – and to the bony architecture, often producing a posterolateral compression fracture of the humeral head known as a Hill-Sachs lesion [2,3]. While many patients recover well from a 1st-time dislocation, a subset, particularly young athletes, go on to develop chronic shoulder instability with recurrent episodes [4]. Traditionally, treatment focused on repairing the Bankart lesion, particularly when the glenoid bone loss was minimal. However, this approach did not fully account for cases where patients continued to experience dislocations despite a seemingly “successful” repair. As our understanding of shoulder biomechanics has evolved, so too has our approach to treatment [5]. A major advancement in this area has been the introduction of the on-track/off-track lesion concept, developed by Yamamoto and Itoi and later expanded by Di Giacomo et al. [6-8]. This model offers a more comprehensive biomechanical perspective, taking into account both the width of the Hill-Sachs lesion and the extent of glenoid bone loss. In simple terms, the glenoid track represents the area of the humeral head that remains in contact with the glenoid during arm elevation and external rotation. If the Hill-Sachs lesion falls within this track, it is classified as on-track, meaning it is less likely to engage the glenoid rim and cause Re-dislocation [9,10]. In contrast, off-track lesions extend beyond this contact zone and are prone to engage, particularly in vulnerable arm positions, increasing the risk of instability. Understanding whether a lesion is on- or off-track helps guide treatment decisions. On-track lesions with minimal bone loss can often be successfully treated with a soft tissue procedure such as arthroscopic Bankart repair. However, in cases of off-track lesions or significant glenoid bone loss, additional procedures – such as remplissage, which “fills in” the Hill-Sachs defect, or bone augmentation techniques, such as the Latarjet procedure – may be necessary to restore stability and prevent recurrence [11]. The case we present here involves a 36-year-old male who experienced recurrent anterior shoulder dislocations over 14 years following an initial sports injury. Despite frequent dislocations, he never sought medical attention, instead opting for self-reduction each time. When he finally presented for evaluation, imaging revealed a Bankart lesion, minimal glenoid bone loss, and a non-engaging, on-track Hill-Sachs lesion [12]. Informed by detailed imaging and biomechanical principles, we performed an arthroscopic Bankart repair with remplissage – a decision based not only on radiographic measurements but also on his clinical history, activity level, and the desire to maximize long-term joint stability. This case underscores the value of a tailored, anatomy-based approach to shoulder stabilization and highlights the importance of early assessment in patients with recurrent instability [13,14].
A 36-year-old right-handed male presented with a longstanding history of recurrent right shoulder dislocations. His first episode occurred 14 years ago while playing shuttle badminton. The shoulder dislocated anteriorly but spontaneously reduced. Since then, he experienced dislocations every 6–8 months, all of which he managed independently. Despite the frequency of dislocations, the patient did not seek medical consultation due to the self-limiting nature of each episode. However, over the past year, he developed increased apprehension and fear of dislocation during routine movements, prompting clinical evaluation.
Clinical examination
- Apprehension test: Positive
- Relocation-release test: Positive
- Anterior drawer test: Negative
- Rotator cuff testing: Negative
- SLAP tear and Biceps testing: Negative
The findings pointed toward anterior instability without signs of rotator cuff pathology or SLAP involvement.
Radiological workup
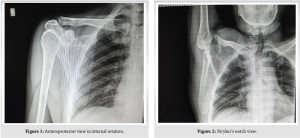
X-ray evaluation
Anteroposterior (AP) view in internal rotation (Fig. 1), and Stryker’s notch view (Fig. 2) revealed the presence of a Hill-Sachs lesion.
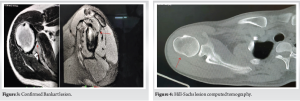
MRI findings
- Confirmed Bankart lesion (Fig. 3)
- No evidence of a rotator cuff tear
- Hill-Sachs lesion evident without engagement (Fig. 4)
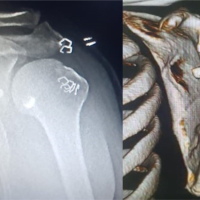
CT 3D reconstruction
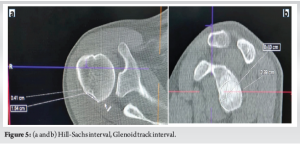
- Hill-Sachs interval = 15.4 mm + 4.2 mm = 19.6 mm (Fig. 5)
- Glenoid Track = (0.83 × D) – d = 20.7 mm (Fig. 5)
- Hill-Sachs interval < Glenoid track = Non-engaging, on-track Hill-Sachs lesion.
Glenoid track (20.7mm) > Hill track interval (19.6mm).
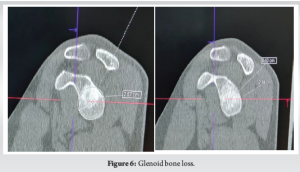
Glenoid bone loss
CT imaging revealed a bone loss of 8%, significantly below the critical threshold of 25%, further favoring a soft tissue repair approach (Fig. 6).
Diagnosis
Chronic post-traumatic anterior shoulder instability of the right shoulder associated with:
- Bankart lesion
- On-track Hill-Sachs lesion
- Glenoid bone loss <25%
Surgical intervention
Procedure Performed: Arthroscopic Bankart Repair with Remplissage
Anesthesia: General
Positioning: Left lateral decubitus with traction
Portals used
- Posterior-superior (primary viewing)
- Anterior (working)
- Lateral
- Posterior-inferior (accessory)
Remplissage
The Hill-Sachs defect was debrided and prepared. Two suture anchors were placed into the lesion, and incorporating the posterior capsule and infraspinatus tendon closed the defect.
Bankart repair
The anteroinferior labrum was reattached using suture anchors placed at 3, 4, and 5 o’clock positions on the glenoid rim (Fig.7, 8).

Post-operative course
The patient was immobilized in a shoulder brace for 4 weeks, followed by a structured rehabilitation program. At 3-month follow-up, he regained nearly full range of motion with no episodes of instability or apprehension during shoulder movements.
Recurrent anterior shoulder dislocation is a common and potentially disabling condition, especially among young, active individuals involved in overhead sports or manual labor. The glenohumeral joint, owing to its wide range of motion and relatively shallow glenoid cavity, is inherently unstable and predisposed to dislocation. The anterior variant accounts for over 90% of shoulder dislocations [15,16]. In the presented case, the patient experienced his first dislocation at age 22 during shuttle badminton – an activity that inherently places stress on the shoulder through repeated overhead motions [17]. His decision to manage each subsequent episode through self-reduction reflects a common patient behavior – underestimating the severity of joint instability when symptoms resolve spontaneously. Unfortunately, this often results in progressive damage to the soft tissue and bony stabilizers of the joint, as seen here [18]. Repeated dislocations lead to capsulolabral damage (Bankart lesion), osseous defects on the posterolateral humeral head (Hill-Sachs lesion), and potentially glenoid bone loss. This triad dictates both the chronicity and complexity of shoulder instability [19]. Without appropriate intervention, such patients develop mechanical instability but also functional impairment, avoidance behavior, and even arthropathy over time [20]. One of the pivotal concepts in modern shoulder stabilization surgery is the “glenoid track” model, which refines our understanding of Hill-Sachs lesions by distinguishing them as “on-track” or “off-track” depending on their potential to engage with the glenoid rim during abduction and external rotation. This radiological insight allows for tailored interventions. In this case, the Hill-Sachs lesion was on track and non-engaging, meaning it was unlikely to cause Re-dislocation in a stable glenoid environment [21]. The glenoid bone loss was quantified at 8%, well below the critical 25% threshold typically associated with poor outcomes following soft tissue-only repairs [22]. Thus, the decision to proceed with an arthroscopic Bankart repair was both rational and evidence-based. However, even non-engaging Hill-Sachs lesions can become clinically relevant when combined with soft-tissue laxity or subtle capsular deficiency. To add an extra layer of biomechanical security, especially considering the patient’s history of frequent dislocations and athletic background, a remplissage procedure was incorporated. This technique, first described by Purchase et al., involves filling the Hill-Sachs defect with the posterior capsule and Infraspinatus tendon, effectively converting the intra-articular defect into an extra-articular one. Studies have shown that this dual procedure significantly reduces recurrence without significantly limiting external rotation [23]. Furthermore, by selecting an arthroscopic approach, the surgical team minimized invasiveness, reduced soft tissue trauma, and allowed for better visualization and access to both anterior and posterior structures [24]. The use of multiple portals, including an accessory poster inferior one, also ensured optimal anchor placement and suture management. The post-operative rehabilitation protocol was crucial. Immobilization allowed for capsulolabral healing, while structured physiotherapy helped restore range of motion and muscle balance [25]. At 3 months post-operative, the patient achieved excellent functional recovery, with no signs of instability or apprehension – an outcome supported by the literature on remplissage-augmented Bankart repair. Finally, this case also emphasizes a larger clinical and psychosocial insight: Patient education and early orthopedic consultation are essential in preventing chronic joint instability. Many patients, especially those who are young and athletic, may delay care, normalize their symptoms, or self-treat without realizing the long-term consequences.
In patients with long-standing anterior shoulder instability, thorough clinical and radiological evaluation is key to formulating a surgical plan. Arthroscopic Bankart repair with remplissage remains a reliable solution for non-engaging Hill-Sachs lesions with minimal glenoid bone loss. Early recognition and intervention can significantly improve outcomes and quality of life.
Early identification and thorough evaluation of bony and soft-tissue defects are essential in patients with recurrent shoulder dislocation. The on-track/off-track concept offers a practical, imaging-based framework to guide surgical decision-making. In patients with minimal glenoid bone loss and a non-engaging Hill-Sachs lesion, arthroscopic Bankart repair with remplissage provides a stable, motion-preserving solution with excellent functional outcomes. Prompt intervention can prevent further joint damage and restore quality of life, especially in active individuals.
References
- 1.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Google Scholar]
- 2.Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: From “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy 2014;30:90-8. [Google Scholar]
- 3.Boileau P, O’Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am 2012;94:618-26. [Google Scholar]
- 4.Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: An indicator of significant bone loss. Arthroscopy 2004;20:169-74. [Google Scholar]
- 5.Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB. Arthroscopic stabilization in patients with an inverted pear glenoid: Results in patients with bone loss of the anterior glenoid. Am J Sports Med 2007;35:1276-83. [Google Scholar]
- 6.Yamamoto N, Itoi E. Concept of glenoid track. JSES Int 2015;19:1-6. [Google Scholar]
- 7.Balg F, Boileau P. The Instability Severity Index Score: A simple pre-operative score to select patients for arthroscopic or open shoulder stabilization. J Bone Joint Surg Br 2007;89:1470-7. [Google Scholar]
- 8.Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs “remplissage”: An arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy 2008;24:723-6. [Google Scholar]
- 9.Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu RK, Bernhardson A, et al. The Hill-Sachs lesion: Diagnosis, classification, and management. J Am Acad Orthop Surg 2012;20:242-52. [Google Scholar]
- 10.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: A long-term end-result study. J Bone Joint Surg Am 1978;60:1-16. [Google Scholar]
- 11.Dickens JF, Owens BD, Cameron KL, Kilcoyne KG, Rue JP. Return to play and recurrent instability after in-season anterior shoulder instability: A prospective multicenter study. Am J Sports Med 2014;42:2842-50. [Google Scholar]
- 12.Shaha JS, Cook JB, Song DJ, Rowles DJ, Bottoni CR, Tokish JM. Redefining “critical” bone loss in shoulder instability: Functional outcomes worsen with “subcritical” bone loss. Am J Sports Med 2015;43:1719-25. [Google Scholar]
- 13.Hurley ET, Montgomery C, Jamal MS, Shimozono Y, Ali Z, Pauzenberger L, et al. Return to sport after the Latarjet procedure for anterior shoulder instability: A systematic review and meta-analysis. Am J Sports Med 2021;49:3125-31. [Google Scholar]
- 14.Calvo E, Granizo JJ, Fernández-Yruegas D. Criteria for surgical treatment of anterior shoulder instability. J Bone Joint Surg Br 2005;87:677-83. [Google Scholar]
- 15.Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res 2002;400:65-76. [Google Scholar]
- 16.DeLong JM, Jiang K, Bradley JP. Posterior instability of the shoulder: A systematic review and meta-analysis of clinical outcomes. Am J Sports Med 2015;43:1805-17. [Google Scholar]
- 17.Bockmann B, Jost B, Hodler J, Gerber C. Chronic posttraumatic anterior shoulder instability: Results of the Bankart-Bristow procedure. J Shoulder Elbow Surg 1998;7:157-63. [Google Scholar]
- 18.Provencher MT, Ghodadra NS, LeClere L, Solomon DJ, Romeo AA. Anatomic approach for arthroscopic glenoid reconstruction. Arthroscopy 2010;26:e27-30. [Google Scholar]
- 19.Cho NS, Yoo JH, Rhee YG. Management of an engaging Hill-Sachs lesion: arthroscopic remplissage with Bankart repair versus Latarjet procedure. Knee Surg Sports Traumatol Arthrosc 2016;24:3793-800. [Google Scholar]
- 20.Ialenti MN, Mulvihill JD, Feinstein M, Zhang AL, Feeley BT. Return to sport after shoulder stabilization procedures: A systematic review. Am J Sports Med 2016;44:3146-55. [Google Scholar]
- 21.Shin SJ, Kim RG, Jeon YS, Kwon TH. Critical value of posterior glenoid bone loss that leads to recurrent instability after arthroscopic posterior Bankart repair. Am J Sports Med 2017;45:1975-81. [Google Scholar]
- 22.Garcia GH, Liu JN, Wong A, Degen RM, Kelly JD. Outcomes of the Latarjet procedure in contact versus noncontact athletes. Orthop J Sports Med 2016;4:2325967116674472. [Google Scholar]
- 23.Millett PJ, Braun S, Gobezie R, Pacheco IH. The Hill-Sachs lesion: Diagnosis, classification, and management. J Am Acad Orthop Surg 2009;17:602-13. [Google Scholar]
- 24.Shibata H, Gotoh M, Mitsui Y, Yamada T, Higuchi F, Nagata K. Clinical outcomes of arthroscopic Bankart repair for shoulder instability with bone loss: Comparison with outcomes for patients without bone loss. J Shoulder Elbow Surg 2015;24:380-6. [Google Scholar]
- 25.Cho NS, Cha SW, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: Results according to the severity of glenoid bone loss. Arthroscopy 2011;27:904-12. [Google Scholar]