Arthroscopic resection and meniscal balancing effectively treat symptomatic discoid meniscus while preserving knee function and preventing long-term joint degeneration.
Dr. Kuru Parvir, Department of Orthopaedics, FMHS SGT University, Budhera District, Gurugram, Haryana, India. E-mail: kpsingla9697@gmail.com
Introduction: Discoid meniscus is a congenital anomaly, most commonly affecting the lateral compartment of the knee, characterized by an abnormally thick, disc-shaped meniscus. While many individuals are asymptomatic, others experience knee pain, swelling, and mechanical symptoms such as locking or clicking. These symptoms often arise due to tears or altered mechanics associated with the discoid shape. Advanced imaging, particularly magnetic resonance imaging (MRI), is crucial for diagnosing discoid meniscus and assessing associated tears, as traditional X-rays offer limited diagnostic value. Surgical intervention, typically through arthroscopy, is often required for symptomatic cases to remove damaged tissue while preserving functional meniscal structures, preventing long-term joint degeneration. This case report discusses the management of a symptomatic discoid lateral meniscus in a 28-year-old male patient.
Case Report: A 28-year-old male presented with a 6-month history of intermittent bilateral knee pain, swelling, and mechanical symptoms exacerbated by physical activities such as running and jumping. Physical examination revealed joint line tenderness and positive McMurray and Apley grind tests on both knees. X-rays suggested a discoid meniscus, with widened joint space and changes in the femoral condyle and tibial plateau. MRI confirmed a complete discoid lateral meniscus with a central tear. The patient underwent arthroscopic resection of the symptomatic portion of the meniscus and meniscal balancing to preserve as much healthy tissue as possible. Postoperatively, the patient reported significant symptom relief, returning to daily activities and sports within 3 months. At 1-year follow-up, there were no signs of recurrent tears or degenerative changes.
Conclusion: Arthroscopic resection and meniscal balancing are effective techniques for treating symptomatic discoid meniscus, enabling the removal of damaged tissue while preserving functional meniscus for long-term joint health. Early diagnosis, advanced imaging, and focused post-operative rehabilitation contribute to favorable outcomes, including the restoration of knee function and return to sports activities.
Keywords: Discoid meniscus, arthroscopic management, meniscal resection, knee surgery, magnetic resonance imaging, knee pain, mechanical symptoms, joint preservation, sports rehabilitation.
The meniscus plays a critical role in knee joint function, acting as a cushion and stabilizer during weight-bearing activities. A discoid meniscus is a congenital anomaly, most commonly affecting the lateral compartment of the knee, characterized by a thicker, disc-shaped meniscus. Although many individuals remain asymptomatic, others experience significant knee pain, swelling, and mechanical symptoms such as locking or clicking, often due to tears or abnormal knee mechanics [1,2]. Diagnosing a discoid meniscus can be challenging, as traditional radiographic techniques may not provide definitive evidence. Advanced imaging modalities, particularly magnetic resonance imaging (MRI), are essential for accurately assessing meniscal morphology and detecting associated injuries [3]. Surgical intervention is often required for symptomatic patients, with arthroscopy being the preferred approach due to its minimally invasive nature and the ability to preserve meniscal tissue [4]. This case report discusses the clinical course of a symptomatic discoid meniscus in a 28-year-old male patient, detailing the diagnostic process, surgical management through arthroscopic resection and balancing, and the favorable outcomes achieved. Through this case, we aim to highlight the importance of early diagnosis and effective treatment strategies in managing discoid meniscus to restore knee function and enhance quality of life.
Patient Information
A 28-year-old male presented with a 6-month history of intermittent bilateral knee pain (R>L), swelling, and mechanical symptoms, including locking and a “clunking” sensation. The patient reported that symptoms were exacerbated by physical activities such as running and jumping. There was no history of significant trauma to the knee.
Clinical findings
Physical examination revealed joint line tenderness on the lateral side of the right knee. The McMurray test was positive, eliciting pain and a palpable click over the lateral joint line. The Apley grind test also reproduced the patient’s symptoms. Similar findings on the left side.
Diagnostic assessment
With the correlation of clinical symptoms, the patient initially advised X-rays, but while X-rays are not definitive for diagnosing a discoid meniscus, they can show indirect signs suggestive of the condition. Here are the findings in detail:
- Widened joint space: A wider joint space on the lateral side may indicate abnormal meniscal shape or pathology (Fig. 1).
- Squared-off femoral condyle: The lateral femoral condyle can appear more squared-off instead of rounded, which is typical in normal anatomy
- Cupped tibial plateau: The lateral tibial plateau may have a more concave appearance, reflecting changes associated with the discoid meniscus
- Elevated fibular head: An elevated position of the fibular head may occur due to altered mechanics in the knee
- Flattened tibial eminence: The tibial eminence may appear flattened, indicating changes in the knee’s morphology.
These findings, combined with clinical symptoms, lead to MRI for a definitive diagnosis. MRI of the bilateral knee was performed, revealing a thickened and disc-shaped lateral meniscus consistent with a complete discoid meniscus. There was evidence of a meniscal tear and associated mild chondral changes [5] (Fig. 2).
Diagnosis
Based on clinical findings and MRI results, the patient was diagnosed with a symptomatic complete discoid lateral meniscus with a tear.
Pre-operative planning
The decision was made to proceed with arthroscopic surgery to resect the symptomatic portion of the discoid meniscus and perform meniscal balancing to restore normal knee function.
Procedure
- Anesthesia and positioning: The patient was placed under general anesthesia and positioned supine with the knee in a standard arthroscopic position
- Arthroscopic portal placement: Standard anterolateral and anteromedial portals were established for arthroscopic access
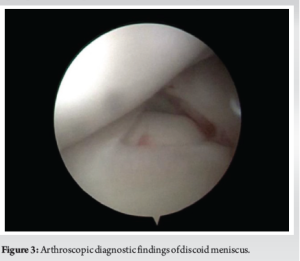
- Diagnostic arthroscopy: Initial diagnostic arthroscopy confirmed the presence of a complete discoid lateral meniscus with a central tear. The meniscus was thickened and covered a larger portion of the tibial plateau than normal (Fig. 3).
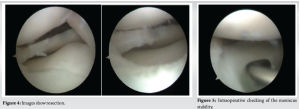
- Resection and balancing: Using a motorized shaver and meniscal scissors, the central portion of the discoid meniscus was resected to remove the torn and symptomatic tissue. Care was taken to preserve as much peripheral meniscal tissue as possible to maintain its function. The remaining meniscus was then reshaped to mimic the normal crescent shape, ensuring the meniscal rim was balanced and stable (Fig. 4).
- Assessment of stability: The stability of the reshaped meniscus was assessed with a probe to ensure that no residual mechanical symptoms would occur. The knee was cycled through a range of motion to confirm smooth movement without catching or locking (Fig. 5).
Post-operative care
Postoperatively, the patient was placed in a knee brace and instructed to weight-bear as tolerated. A structured rehabilitation program was initiated, focusing on a range of motion exercises and progressive strengthening. Emphasis was placed on quadriceps and hamstring strengthening to support knee stability.
Outcome and follow-up
Early post-operative period: The patient reported significant improvement in symptoms within the first few weeks postoperatively. At the 2-week follow-up, the patient demonstrated a good range of motion with minimal pain and no mechanical symptoms. The swelling was minimal, and the surgical wounds were healing well.
Mid-term follow-up: At 3 months postoperatively, the patient had returned to normal daily activities without pain or mechanical symptoms. Physical examination revealed a full range of motion and no joint line tenderness. The patient was able to participate in light sports activities.
Long-term follow-up: At 1-year follow-up, the patient reported a complete resolution of pre-operative symptoms. MRI performed at this time showed a well-preserved lateral meniscus with a normal configuration and no evidence of recurrent tears or degenerative changes. The patient had returned to full sports participation and expressed high satisfaction with the surgical outcome [6].
Arthroscopic resection and balancing
The case demonstrates that arthroscopic resection and balancing are effective for treating symptomatic discoid meniscus. This approach allows for the removal of the symptomatic portion of the meniscus while preserving as much functional meniscal tissue as possible. Studies such as those by Good et al. (2007) and Ahn et al. (2010) support the use of arthroscopic techniques for discoid meniscus, showing favorable outcomes in terms of knee function and patient satisfaction [1,2].
Diagnostic challenges
MRI is essential for diagnosing discoid meniscus, as it provides detailed images of meniscal morphology and associated pathology. In this case, MRI was crucial for identifying the complete discoid meniscus and the associated tear, guiding the surgical approach [5,7]
Importance of meniscal preservation
Preserving meniscal tissue is critical for maintaining knee biomechanics and preventing degenerative changes. Meniscal balancing aims to reshape the discoid meniscus to a more normal configuration, which helps distribute the load more evenly across the joint and reduces the risk of osteoarthritis. Research by Ahn et al. (2010) highlights the importance of meniscal preservation in improving long-term outcomes [2,6].
Rehabilitation and long-term outcomes
A structured rehabilitation program is essential for optimal recovery post-surgery. Early mobilization and progressive strengthening help restore knee function and prevent complications. Long-term follow-up is crucial to monitor for recurrence of symptoms and degenerative changes. This case showed that with proper surgical technique and post-operative care, patients can achieve excellent long-term outcomes, including the return to full sports participation [4,6].
Other management options
Non-surgical management may be appropriate for asymptomatic or mildly symptomatic discoid meniscus. This includes activity modification, physical therapy, and anti-inflammatory medications. However, for symptomatic cases, surgical intervention is often necessary to relieve symptoms and restore knee function. Future advancements in biological therapies, such as platelet-rich plasma and stem cell injections, hold potential for enhancing meniscal healing and regeneration, possibly reducing the need for surgical intervention in select cases [8-10].
This case underscores the importance of a thorough clinical evaluation and advanced imaging in diagnosing a discoid meniscus, particularly when symptoms are present. Arthroscopic resection and balancing emerged as effective surgical strategies for treating symptomatic discoid menisci, allowing for the removal of damaged tissue while preserving as much healthy meniscal structure as possible. The positive post-operative outcomes observed in this patient suggest that such approaches can lead to successful restoration of knee function and patient satisfaction. Continued emphasis on rehabilitation and monitoring is essential to ensure optimal long-term results. Future research may explore non-surgical management options and innovative biologic therapies to enhance meniscal healing and minimize the need for surgical intervention.
Early diagnosis and appropriate surgical intervention can lead to significant improvement in symptoms and long-term functional outcomes in patients with symptomatic discoid meniscus.
References
- 1.Good CR, Green DW, Griffith MH, Valen A. Arthroscopic resection of the symptomatic discoid lateral meniscus in children: A minimum 2-year follow-up. J Pediatr Orthop 2007;27:810-4. [Google Scholar | PubMed]
- 2.Ahn JH, Lee SH, Yoo JC, Lee SJ, Ha HC. Arthroscopic meniscal repair in the lateral discoid meniscus of children: Mid-term and long-term outcomes. J Bone Joint Surg 2010;92:2565-72. [Google Scholar | PubMed]
- 3.Lee DH, Lee JH, Kim TH. Magnetic resonance imaging findings of discoid lateral meniscus tear: Evaluation of the extent of tear and type of tear pattern. Skeletal Radiol 2007;36:935-41. [Google Scholar | PubMed]
- 4.Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus. Clin Orthop Relat Res 1975;201:57-62. [Google Scholar | PubMed]
- 5.Samoto N, Kozuma M, Tokuyasu K, Takeuchi T, Fukubayashi T. The radiological findings of the discoid meniscus: Comparative analysis between plain radiographs, MRI, and arthroscopic findings. Knee Surg Sports Traumatol Arthrosc 1996;4:190-3. [Google Scholar | PubMed]
- 6.Werner BC, Yang S. The role of meniscal preservation in the treatment of symptomatic discoid lateral meniscus. Orthop J Sports Med 2015;3:2325967114568041. [Google Scholar | PubMed]
- 7.Vangsness CT. Platelet-rich plasma: A promising new treatment for joint injuries. Am J Sports Med 2014;42:1259-64. [Google Scholar | PubMed]
- 8.Zayni M, Debieux P. Platelet-rich plasma in the management of meniscal tears: Systematic review and meta-analysis. Int Orthop 2015;39:993-9. [Google Scholar | PubMed]
- 9.Anderson D, Blanke J. Stem cells for meniscal regeneration: A promising area of research. Orthop J Sports Med 2008;6:2325967118764681. [Google Scholar | PubMed]
- 10.Kim JY, Lee SH. The use of stem cells in meniscal repair and regeneration: A review of the literature. Knee Surg Sports Traumatol Arthrosc 2019;27:3851-39. [Google Scholar | PubMed]