Isolated ulna fracture with DRUJ injury requires skilful reduction and gentle manipulation.
Dr. Sukhmin Singh, Department of Orthopaedics, AIIMS Bilaspur - 174 001, Himachal Pradesh, India. E-mail: Sukhmin92@gmail.com
Introduction: Galeazzi fracture is known as the fracture of the distal end radius with distal radioulnar joint dislocation. Many patterns are described in literature which are equivalent but the distal ulna shaft fracture with distal radioulnar joint dislocation is rarely mentioned. We present a case report of this rare pattern.
Case Report: A 20-year-old male presented to our emergency department with complaints of pain and swelling over the left wrist. After initial assessment, radiographs of the wrist with forearm and hand were taken. Radiograph revealed a distant pattern of fracture which was distal 3rd of ulna shaft fracture with distal radioulnar joint dislocation. The patient was planned for operative intervention and open reduction internal fixation was done using a standard low contact dynamic compression plate and k-wire fixation for DRUJ. Postoperative DASH score after 18 months is 19.2. After 2-year follow-up, the patient has full range of motion at wrist without any pain and no arthritic changes.
Conclusion: With the ulna shaft fracture, DRUJ is usually not involved. Ulna shaft fracture with DRUJ dislocation is a rare injury which if promptly managed early with surgical intervention yields satisfactory results.
Keywords: Reverse galeazzi, DRUJ Dislocation, isolated ulna fracture
Injuries to the Galeazzi fractures, which involve a fracture in the middle to the distal third of the radius, along with dislocation or instability at the distal radioulnar joint (DRUJ), have been thoroughly studied for many years. The first documented case of a simple volar dislocation of the DRUJ was reported in 1777 by Desault, and since then, there have been only a few case reports on this specific type of injury, where the ulna is dislocated volarly without any fracture of the distal radius or ulna [1-4]. For the ulna to fully dislocate volarly, there must be either an ulnar styloid fracture or damage to the triangular fibrocartilage complex (TFCC). However, the majority of the rare case reports on DRUJ dislocation without associated radius fractures do not mention an ulnar styloid fracture. Sonohata et al. [4] in Japan reported a traumatic volar dislocation of the distal ulna with an avulsion fracture of the ulna styloid, marking this as the only documented case of such an injury. It is believed that many of these injuries to the DRUJ go undiagnosed and unreported due to the limitations of emergency department radiographs and the challenges in interpreting subtle injuries to the DRUJ [5-7]. A volar dislocation of the ulna typically happens when the forearm is in a highly supinated position, with the hand fixed in place. This type of injury has been reported in weightlifting, likely due to a supination injury with the hand stationary against the weight, and from falls or direct blows to the wrist. This makes sense because, during forearm supination at the DRUJ, the radius moves posteriorly and stretches out more than the ulna, which is the opposite during forearm pronation [8-14]. It’s important to understand the anatomy of the DRUJ and how changes in forearm position affect its stability. The radius of curvature of the sigmoid notch is greater than that of the ulna head, contributing only about 20% to the stability of the DRUJ. This shallow contact also allows for a wide range of motion in the joint during pronosupination [15-19]. At a neutral position, there’s about 60% of contact between the bones, but at the extremes of supination and pronation, this can drop to as little as 10%, illustrating the limited intrinsic stability of the joint when the wrist is highly supinated. Therefore, when the forearm is in a highly supinated position, the injury relies more on the soft tissues for stabilization, and damage to these tissues can result in a dislocation at the DRUJ. The main soft tissue stabilizer of the DRUJ is the TFCC, which is made up of deep and superficial fibers. The deep fibers are crucial for preventing dislocation of the bones from the palmar and dorsal sides during pronosupination, while the superficial fibers help in restraining rotation. The deep fibers attach to the ulnar fovea, and the superficial fibers connect to the ulnar styloid, playing key roles in the joint’s stability. There have been few cases reported in the literature of isolated intra-articular distal ulna fractures without associated distal radius fracture, and these were all managed surgically [18-20]. To our knowledge, this is the only reported case of a distal ulna fracture of this nature with dislocation of the DRUJ without a concomitant distal radius fracture. It was successfully managed surgically.
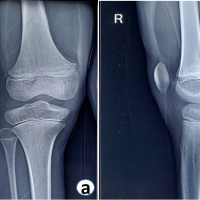
A 20-year-old male, presented to our emergency department with complaints of pain and loss of movement in his left wrist, following a fall on outstretched hand. There was no history of diabetes, hypertension, alcohol, and smoking. On examination, diffuse tenderness and swelling were present over the left wrist. No distal neurovascular deficit was noted. No other injuries were noted during the examination. Immobilization and analgesics were given in an emergency. Plain radiographs revealed distal 1/3rd shaft of ulna fracture with distal radioulnar joint dislocation (Fig. 1).
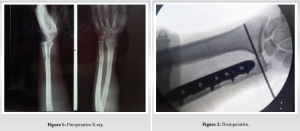 Radiographs of the elbow were also done which was normal The patient was prepared for operative intervention and necessary investigations were done. The subcutaneous approach was used and open reduction internal fixation was done using standard low-contact dynamic compression plate (Fig. 2). Distal radioulnar joint was reduced with the help of a pointed reduction clamp and a 2 mm k wire was inserted from ulna to radius. The challenge faced during this case was the reduction of radioulnar joint after ulna fixation. Radial deviation with traction and countertraction was done to reduce the DRUJ. We initially tried to reduce DRUJ first and fix the ulna afterward with holding the DRUJ using a reduction clamp but was not possible. So we fixed ulna first and reduced DRUJ later on. Postoperatively, the wrist was immobilized for 4 weeks. The K-wire was removed after 4 weeks. The gradual physiotherapy with wrist range of motion and grip strengthening exercises were started. Wrist range of motion was fully achieved in about 8 weeks and grip strength was also within preoperative status by 10 weeks. After that, all normal activities were allowed to patient which was done preoperatively by the patient. He was followed up at 2 weeks, 4 weeks, and then monthly thereafter. After 1 year of follow-up, the fracture has healed completely (Fig. 3) and had a satisfactory range of motion (Table 1). He was able to carry out his activities of daily living comfortably and his Disability of the Arm, Shoulder, and Humerus of the (DASH) [5] score was calculated to be 19.2.
Radiographs of the elbow were also done which was normal The patient was prepared for operative intervention and necessary investigations were done. The subcutaneous approach was used and open reduction internal fixation was done using standard low-contact dynamic compression plate (Fig. 2). Distal radioulnar joint was reduced with the help of a pointed reduction clamp and a 2 mm k wire was inserted from ulna to radius. The challenge faced during this case was the reduction of radioulnar joint after ulna fixation. Radial deviation with traction and countertraction was done to reduce the DRUJ. We initially tried to reduce DRUJ first and fix the ulna afterward with holding the DRUJ using a reduction clamp but was not possible. So we fixed ulna first and reduced DRUJ later on. Postoperatively, the wrist was immobilized for 4 weeks. The K-wire was removed after 4 weeks. The gradual physiotherapy with wrist range of motion and grip strengthening exercises were started. Wrist range of motion was fully achieved in about 8 weeks and grip strength was also within preoperative status by 10 weeks. After that, all normal activities were allowed to patient which was done preoperatively by the patient. He was followed up at 2 weeks, 4 weeks, and then monthly thereafter. After 1 year of follow-up, the fracture has healed completely (Fig. 3) and had a satisfactory range of motion (Table 1). He was able to carry out his activities of daily living comfortably and his Disability of the Arm, Shoulder, and Humerus of the (DASH) [5] score was calculated to be 19.2.

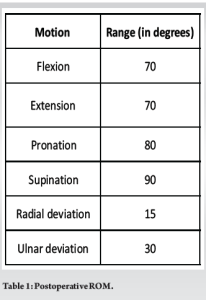
Isolated shaft of ulna fracture is a common finding in the emergency department encountered by the orthopedics team. Distal ulna fracture with distal radioulnar joint dislocation without involving radius is however a rare injury which is not described in literature. Ulna dislocation at the DRUJ is commonly associated with the radius fracture which is Galeazzi fracture pattern. In a Galeazzi fracture, the dislocation is typically dorsal. Reduction in such cases is blocked by many factors that include the extensor tendons, most commonly the extensor carpi ulnaris or the extensor digiti mini. Volar dislocations are rarely encountered which includes fracture fragments or the ulna dislocating through the volar capsule and implicated as block to reduction in irreducible Galeazzi fractures. In our case, the fragment was dislocated dorsally and distally increasing the ulnar variance. Surgeons should be aware of the potential blocks to reduction when evaluating these rare fractures. There are very few case reports of isolated distal ulnar dislocations without any fracture. Distal 1/3rd ulna shaft fractures with DRUJ dislocation without a distal radius fracture are rare, and there is sparse literature characterizing these fractures. To our knowledge, there is no case report of a similar nature is published. However, there are case reports with distal ulna styloid fractures with the size and pattern of the fracture different and transverse at the base of the styloid. Most ulnar fractures occur in concordance with distal radius fractures. Isolated ulna fractures are mainly due to a direct blow to the ulna and occur usually in the proximal region of the shaft without the involvement of the DRUJ. Rather than a transverse fracture at the base of the styloid like most ulnar styloid avulsions, our patient had a transverse fracture that was in the distal 1/3rd of the shaft with fracture fragments overlapping. This type of fracture pattern has a high probability of non-reduction and displacing with closed treatment. Reduction was tried in our case but wasn’t achievable and was planned for operative intervention. The pattern of injury was a true fracture-dislocation of the ulna as the TFCC remained attached to the distal ulnar fracture fragment. We believe this type of fracture-dislocation should always be managed with open-operative treatment to fully assess reduction of the ulnar fracture and the DRUJ [21]. The stability of the DRUJ returned once bony union of the fracture was achieved. Shortening and malrotation of the distal ulna with the widening of the DRUJ can lead to a more severe loss of forearm pronation and supination than more proximal ulnar shaft fracture. One case series published by Kang et al. [22] described isolated distal ulna fractures in 10 patients. The authors described 3 fracture types: type I being simple fractures of the distal ulna shaft, type II being comminuted fractures without involvement of the DRUJ, and type III being fractures with DRUJ instability. While similar to our patient, type III fractures in this case series did not extend through the ulnar head; instead, the fracture line exited in the DRUJ. The authors treated 3 type III fractures with tension bands having two-thirds good/excellent results and one-third poor results. The authors also hypothesized that disruption of the IM in these fractures led to DRUJ instability. If the fracture was more than 50% displaced on the original radiograph, then IM disruption is likely. The authors also recommended operative fixation for unstable fractures and more than 50% displacement or 15° of angulation. The difference in fracture pattern distinguishes our patient from the above case series. Only 66% had good or excellent results in this very small sample size, which shows that although not identical to our patient’s scenario, a clear preferred method of operative treatment has not been described for these distal wrist injuries. Most of the literature guiding the management of distal ulna fractures refers to ulnar styloid, ulnar shaft, or fractures associated with a distal radius fracture. To clarify the best time for surgery, fixation techniques, postoperative immobilization, postoperative rehabilitation schedules, and assess long-term complications of these kinds of fracture dislocations, more research would be required. The majority of the earlier studies on Galleazi fractures can be used to help direct the intra- and postoperative protocols. A brief timeline of our patient’s treatment course can guide future treatment plans for orthopedic surgeons who encounter similar fractures. The patient was immobilized in a long arm slab with the k-wire in place for the first 2 weeks. At 2 weeks, the sutures were taken out, and a short arm splint was placed with maintenance of the K-wire for another 4 weeks. The wire was removed at 6 weeks postoperatively. At 8 weeks, the patient regained almost all the movements with pronation of around 80 and supination of 60° At follow-up—now approximately 3 months after open reduction and internal fixation, the patient has ~160° of combined pronosupination compared with his contralateral extremities of 170°. Six months postoperatively, the patient has nearly equivalent pronosupination to his contralateral extremity, equivalent grip strength, and has returned to active daily life.
Isolated ulna fracture with DRUJ injury should be recognized as a reverse Galeazzi pattern with ulna fracture requiring gentle manipulation as chances of breaking the cortex while reducing the fracture are higher. Radial deviation with reducing fracture gently should be carried out to prevent any further damage to bone or soft tissue.
Reverse Galeazzi pattern should be treated surgically with radial deviation and reduction while preventing cortical comminution.
References
- 1.Mikic ZD. Galeazzi fracture-dislocations. J Bone Joint Surg 1975;57:1071-80. [Google Scholar | PubMed]
- 2.McMurray D, Muralikuttan K. Volar dislocation of the distal radio-ulnar joint without fracture: A case report and literature review. Injury Extra 2008;39:352-5. [Google Scholar | PubMed]
- 3.Wesely MS, Barenfeld PA, Bruno J. Volar dislocation distal radioulnar joint. J Trauma 1972;12:1083-8. [Google Scholar | PubMed]
- 4.Sonohata M, Mine H, Tsuruta T, Mawatari M. Traumatic volar dislocation of the distal ulna with a fracture of the ulna styloid. Hand Surg 2012;17:383-6. [Google Scholar | PubMed]
- 5.Mittal R, Kulkarni R, Subsposh SY, Giannoudis PV. Isolated volar dislocation of the distal radioulnar joint: How easy to miss! Eur J Emerg Med 2004;11:113-6. [Google Scholar | PubMed]
- 6.Dameron TB. Traumatic dislocation of the distal radio-ulnar joint. Clin Orthop Relat R 1972;83:55-63. [Google Scholar | PubMed]
- 7.Francobandiera C, Maffulli N, Lepore L. Distal radio-ulnar joint dislocation, ulna volar in a female body builder. Med Sci Sports Exerc 1990;22:155-8. [Google Scholar | PubMed]
- 8.Rose-Innes AP. Anterior dislocation of the ulna at the inferior radio-ulnar joint; case reports with a discussion of the anatomy of rotation of the forearm. J Bone Joint Surg Br 1960;42B:515-21. [Google Scholar | PubMed]
- 9.Kumar A, Iqbal MJ. Missed isolated volar dislocation of distal radio-ulnar joint: A case report. J Emerg Med 1999;17:873-5. [Google Scholar | PubMed]
- 10.Stuart PR, Berger RA, Linscheid RL, An KN. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg Am 2000;25:689-99. [Google Scholar | PubMed]
- 11.Ekenstam F, Hagart CG. Anatomical studies on the geometry and stability of the distal radioulnar joint. Hand Clin 1987;3:41-50. [Google Scholar | PubMed]
- 12.Hagert CG. The distal radioulnar joint. Hand Clin 1987;3:41-50. [Google Scholar | PubMed]
- 13.Kleinman WB. Stability of the distal radioulnar joint: Biomechanics, pathophysiology, physical diagnosis, and restoration of function-what we have learned in 25 years. J Hand Surg Am 2007;32:1086-106. [Google Scholar | PubMed]
- 14.Xu J, Tang JB. In vivo changes in lengths of the ligaments stabilizing the distal radioulnar joint. J Hand Surg Am 2009;34:40-5. [Google Scholar | PubMed]
- 15.Pidgeon TS, Crisco JJ, Waryasz GR, Moore DC, DaSilva MF. Ulnar styloid base fractures cause distal radioulnar joint instability in a cadaveric model. Hand 2018;13:65-73. [Google Scholar | PubMed]
- 16.Sammer DM, Chung KC. Management of the distal radioulnar joint and ulnar styloid fracture. Hand Clin 2012;28:199-206. [Google Scholar | PubMed]
- 17.Hagert CG. Distal radius fracture and distal radio-ulnar joint-anatomical considerations. Handchir Mikrochir Plast Chir 1994;26:22-6. [Google Scholar | PubMed]
- 18.Jakab E, Ganos DL, Gagnon S. Isolated intra-articular fracture of the ulnar head. J Orthop Trauma 1993;7:290-2. [Google Scholar | PubMed]
- 19.Solan MC, Rees R, Molloy S, Proctor MT. Internal fixation after intra-articular fracture of the distal ulna. J Bone Joint Surg Br 2003;85:279-80. [Google Scholar | PubMed]
- 20.Goikoetxea X, Garmilla I, Etxebarria I, Careaga M. Isolated intraarticular fracture of the distal ulna: A rare injury related to airbag deployment. J Orthop Trauma 2006;20:292-4. [Google Scholar | PubMed]
- 21.Seitz WH Jr., Papandrea RF. Fracture and dislocation of the wrist. In: Bucholz BW, Heckman JD, editors. Rockwood and Green’s Fractures in Adults. Philadelphia, PA: Lippincott Williams and Wilkins; 2001. p. 771-907. [Google Scholar | PubMed]
- 22.Kang HJ, Shim DJ, Yong SW, Yang GH, Hahn SB, Kang ES. Operative treatment of isolated distal ulnar shaft fracture. Yonsei Med J 2002;43:631-6. [Google Scholar | PubMed]