Desmoplastic fibroma, though benign, is a rare and locally aggressive bone tumor that requires careful radiological and histopathological evaluation for accurate diagnosis and appropriate surgical management.
Dr. Indrajeet Kumar, Department of Orthopaedics. Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India E-mail: Indrajeet98ortho@rediffmail.com, Indrajeet98ortho@gmail.com
Introduction: Desmoplastic fibroma (DF) is a very rare, benign but aggressive bone tumor. It makes up <0.1% of all bone tumors and is often mistaken for other conditions, such as bone cysts or giant cell tumors. DF can occur in different bones, but it is uncommon in the proximal femur. Because it looks like other bone diseases on X-rays, diagnosing it correctly can be difficult. Proper treatment is needed to prevent it from coming back. However, due to its rarity, treatment recommendations are largely based on individual case reports, limiting the ability to establish standardized protocols.
Case Report: A 16-year-old boy had pain in his upper left thigh for 3 years. The pain was dull and got worse when he walked or put weight on his leg. X-rays showed a lytic lesion in his femur, which looked like a bone cyst. He underwent surgery where the lesion was scraped out, and bone grafting with a bio-composite was done along with dynamic hip screw fixation. Tests on the removed tissue confirmed DF. After surgery, he was gradually allowed to bear weight and was followed up for 3 years. While this case demonstrates a favorable outcome, it is important to acknowledge that individual responses to treatment may vary, and long-term recurrence risk remains uncertain.
Conclusion: Even though DF is benign, it can still cause problems if not treated properly. The retrospective nature of this report limits its ability to establish causality or determine the best treatment approach. Long-term follow-ups are necessary to make sure it does not come back. Further studies, including larger case series and comparative analyses, are needed to refine treatment strategies and assess long-term outcomes.
Keywords: Desmoplastic fibroma, bone tumor, femur, curettage, bone grafting, dynamic hip screw fixation.
Desmoplastic fibroma (DF) is an extremely rare, benign, yet locally aggressive bone tumor first described by in 1958 [1]. It accounts for <0.1% of all primary bone tumors and is characterized by abundant collagen deposition and fibroblastic proliferation [2]. DF can affect any skeletal site, but most commonly involves the mandible, femur, pelvis, radius, and tibia [3]. Due to its non-specific clinical presentation and radiographic resemblance to other lytic bone lesions, DF is often misdiagnosed as a bone cyst, giant cell tumor, or fibrous dysplasia [4]. The proximal femur is an unusual site for DF, with only a few reported cases in the literature [5,6]. Patients typically present with chronic pain and minimal functional impairment, making early diagnosis challenging [7]. Radiologically, DF exhibits a well-defined, expansile, lytic lesion with a “soap bubble” appearance and cortical thinning [8]. Histopathological examination is essential for a definitive diagnosis, distinguishing DF from more aggressive neoplastic conditions [9]. Although DF is benign, its high recurrence rate following inadequate resection necessitates a carefully planned surgical approach [10]. Treatment options include intralesional curettage, wide resection, and reconstruction depending on lesion size, location, and risk of recurrence [11]. We present a case of DF in the proximal femur of a 16-year-old male, successfully managed with extended curettage, bone grafting, bio-composite augmentation, and dynamic hip screw (DHS) fixation. This case highlights the diagnostic challenges, surgical management, and long-term outcomes of DF in the femur.
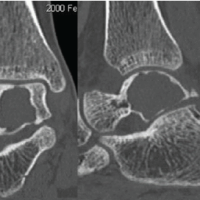
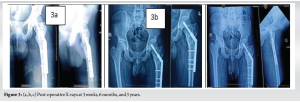
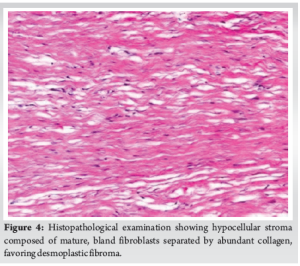
A 16-year-old male presented to the outpatient department with a 3-year history of persistent pain in the proximal left thigh, following a fall from height sustained at that time. He experienced gradually progressive pain, dull aching in character, non-radiating, aggravated on walking/weight bearing, relived after rest or taking analgesics. A physical examination revealed no evident abnormalities, with the exception of tenderness over the proximal thigh. Radiographic picture showed well-defined expansile lesion with thin cortex, multi-lobulated soap bubble appearance, with loss of corticomedullary differentiation, no periosteal reaction, extending from base of neck up to the proximal femur (Fig. 1). The whole-body skeletal survey did not show similar lesion elsewhere in the body. The initial diagnosis at admission was of a bone cyst, based on radiological evidence, that revealed a well-defined cortical rim was noted with soft tissues component within and lesion was approximately 29.4 × 36.6 mm on non-contrast computed tomography (CT) left femur (Fig. 2). The patient underwent extended curettage with Bone graft, bio composite augmentation and DHS fixation of left hip Joint (Fig. 1). Histological examination revealed hypocellular stroma composed of mature bland fibroblasts separated by abundant collagen without nuclear atypia. In addition, there was no necrosis (Fig. 4). Thus, based on the postoperative analyses and histological report, a diagnosis of DF was determined. The patient was advised to remain on bed – rest for 3 months, and then partial weight – bearing was allowed. The patient was followed up every month for the first 6 months, then every 3 months physically and radiologically (Fig. 5). At 3-year follow-up, there was no disability or local recurrence or distant metastasis (Fig.5).

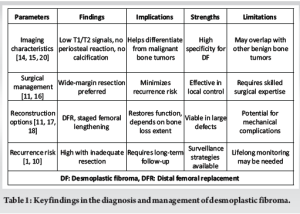
DF of the bone is an extremely rare benign tumor with locally aggressive behavior [12]. Despite its benign nature, DF poses significant challenges in diagnosis and management due to its potential for extensive bone destruction and high recurrence rates following inadequate resection [13]. As this is a single case report, definitive causal relationships cannot be established; however, our aim is to highlight key clinical and surgical considerations that may inform future cases. The present case underscores the importance of accurate imaging, histopathological confirmation, and appropriate surgical intervention in managing DF of the distal femur [9]. The imaging characteristics of DF have been extensively studied to aid in differentiation from other bone lesions [12]. Zhang et al. analyzed clinical and imaging features in 20 patients with DF, revealing that the tumor predominantly affects the metaphysis of long bones, particularly the femur, ilium, and tibia. Their study classified DF into four imaging types: Cystic expansile destruction, osteolytic destruction, mixed destruction, and paraosseous destruction [14]. Notably, DF typically exhibits low signals on T1- and T2-weighted magnetic resonance images, lacks periosteal reaction, and demonstrates no calcification, which helps distinguish it from malignant bone tumors [14,15]. While these findings provide valuable diagnostic insights, it is important to recognize that rare cases may present atypically, necessitating careful clinical correlation. Fludeoxyglucose positron emission tomography (FDG PET)/CT and bone scintigraphy have also proven useful in assessing DF activity. Zhang et al. described two cases of DF, one in the distal femur and another in the ninth rib, both demonstrating increased FDG uptake and Technetium-99m Methylene Diphosphonate(99 uptake. These findings suggest that PET/CT may help identify metabolically active regions within the tumor, guiding surgical planning and postoperative surveillance [15]. However, given the retrospective nature of this report, it is difficult to determine the precise role of advanced imaging in predicting outcomes, and further studies are needed to validate these findings. Various surgical strategies have been proposed for DF management, with wide-margin resection being the preferred approach to minimize recurrence risk [16]. The use of distal femoral replacement (DFR) as a salvage procedure following DF resection has been successfully demonstrated in prior reports. Torres-Lugo et al. described a case where a patient with a DF initially misdiagnosed as fibrous dysplasia underwent wide excision and subsequent DFR, achieving restoration of anatomy and function. The successful application of DFR underscores its viability as a reconstructive option in cases where significant bone loss precludes traditional bone grafting techniques [17]. Although our case demonstrates a favorable outcome, it is essential to recognize that surgical decision-making must be tailored to individual patient factors, and generalizing conclusions from a single case should be approached with caution. Alternative reconstruction techniques have also been explored. Stevens et al. reported a rare case of DF in the femoral midshaft presenting with a pathological fracture. The patient was managed with en bloc excision and acute shortening, followed by gradual femoral re-lengthening using an intramedullary skeletal kinetic distractor. This approach preserved the native joint articulation and achieved excellent long-term functional outcomes [18]. Such innovative techniques highlight the importance of individualized treatment planning in DF cases. Despite surgical advancements, recurrence remains a significant concern. Xu et al. reported a case where DF was treated with wide resection, achieving disease-free status at a 1-year follow-up [19]. However, longer-term surveillance is essential, as recurrences have been documented even years after initial treatment. Publication bias remains a potential concern, as successful or unusual cases are more likely to be reported, while cases with suboptimal outcomes may be underrepresented in the literature. In addition, focusing on rare cases should not detract from the importance of recognizing and managing more common bone tumors. DF’s non-specific imaging findings may delay diagnosis, emphasizing the need for histopathological evaluation in suspicious cases (Table 1).
DF of the bone remains a rare but challenging tumor requiring a multimodal approach for optimal management. Advances in imaging have improved diagnostic accuracy, while evolving surgical techniques provide better reconstructive options. While this report adds to the existing literature, it is important to recognize the inherent limitations of single-case observations. Future research should focus on developing novel adjuvant therapies to reduce recurrence rates and exploring less invasive surgical approaches to minimize morbidity. In addition, addressing potential publication bias by systematically analyzing both successful and unsuccessful treatment outcomes will provide a more balanced understanding of DF management. Long-term multicenter studies are needed to establish standardized treatment protocols and improve patient outcomes.
Desmoplastic fibroma of the femur is often misdiagnosed due to its non-specific clinical and radiological presentation. Extended curettage with bone grafting and internal fixation can provide good functional outcomes while minimizing recurrence. Early recognition and appropriate surgical intervention are key to preventing complications and preserving limb function.
References
- 1.Jaffe H.L. Tumours and tumorous conditions of the bones and joints. In: Lea, Febiger, editors. Lea and Febiger; Philadelphia: 1958. pp. 298–303. [Google Scholar | PubMed]
- 2.Zhang LL, Yang HL, Li XF, Yuan J. Desmoplastic fibroma of ilium. Orthop Surg 2011;3:216-8. [Google Scholar | PubMed]
- 3.Woods TR, Cohen DM, Islam MN, Rawal Y, Bhattacharyya I. Desmoplastic fibroma of the mandible: A series of three cases and review of literature. Head Neck Pathol 2015;9:196-204. [Google Scholar | PubMed]
- 4.Nedopil A, Raab P, Rudert M. Desmoplastic fibroma: A case report with three years of clinical and radiographic observation and review of the literature. Open Orthop J 2013;8:40-6. [Google Scholar | PubMed]
- 5.Ishizaka T, Susa M, Sato C, Horiuchi K, Koga A, Kumazawa F, et al. Desmoplastic fibroma of bone arising in the cortex of the proximal femur. J Orthop Sci 2021;26:306-10. [Google Scholar | PubMed]
- 6.Gong YB, Qu LM, Qi X, Liu JG. Desmoplastic fibroma in the proximal femur: A case report with long-term follow-up. Oncol Lett 2015;10:2465-7. [Google Scholar | PubMed]
- 7.Tanwar YS, Kharbanda Y, Rastogi R, Singh R. Desmoplastic fibroma of bone: A case series and review of literature. Indian J Surg Oncol 2018;9:585-91. [Google Scholar | PubMed]
- 8.Abu Alnasr AA, Sulaiman SR, Abu Alnasr AA, Qari Y, Al Arabi RM. Successful treatment of a case of desmoplastic fibroma: A case of unusual lesion. Cureus 2021;13:e17857. [Google Scholar | PubMed]
- 9.Gong LH, Liu WF, Ding Y, Geng YH, Sun XQ, Huang XY. Diagnosis and differential diagnosis of desmoplastic fibroblastoma by clinical, radiological, and histopathological analyses. Chin Med J (Engl) 2018;131:32-6. [Google Scholar | PubMed]
- 10.Yokouchi M, Ueno Y, Nagano S, Shimada H, Nakamura S, Setoguchi T, et al. Extended curettage and heat ablation for desmoplastic fibroma of the distal femur with a 12-year follow-up period: A case report. Oncol Lett 2014;8:1103-6. [Google Scholar | PubMed]
- 11.Kinoshita H, Ishii T, Kamoda H, Hagiwara Y, Tsukanishi T, Orita S, et al. Successful treatment of a massive desmoplastic fibroma of the ilium without surgery: A case report with long-term follow-up. Case Rep Orthop 2020;2020:5380598. [Google Scholar | PubMed]
- 12.Sferopoulos NK. Periosteal desmoplastic fibroma of the tibia in a 3-year-old child. Eur J Orthop Surg Traumatol 2015;25:1233-8. [Google Scholar | PubMed]
- 13.Razavipour M, Akhlaghi H, Abdollahi A. Overcoming diagnostic challenges in desmoplastic fibroma of the scapula: A rare case report. Oxf Med Case Rep 2023;2023:omad057. [Google Scholar | PubMed]
- 14.Zhang ZZ, Cao L, Zhong ZW, Guo Z, Wu HZ, Wu WJ, et al. Clinical and imaging features of desmoplastic fibroma of bone for correct diagnosis and differentiation. Curr Med Imaging 2022;18:1093-8. [Google Scholar | PubMed]
- 15.Zhang J, Nian S, Bai Y, Dong A. FDG PET/CT and bone scintigraphy in desmoplastic fibroma of the bone. Clin Nucl Med 2022;47:878-81. [Google Scholar | PubMed]
- 16.Rui J, Guan W, Gu Y, Lao J. Treatment and functional result of desmoplastic fibroma with repeated recurrences in the forearm: A case report. Oncol Lett 2016;11:1506-8. [Google Scholar | PubMed]
- 17.Torres-Lugo NJ, Beatón-Comulada D, Colón-Miranda R, Bibiloni-Lugo JP, Ramírez N, Bibiloni-Rodríguez J. Distal femoral replacement as a salvage treatment after desmoplastic fibroma resection. Arthroplast Today 2022;16:39-45. [Google Scholar | PubMed]
- 18.Stevens J, Moin S, Salter D, Patton JT. Desmoplastic fibroma: A rare pathological midshaft femoral fracture treated with resection, acute shortening, and re-lengthening: A case report. JBJS Case Connect 2019;9:e0022. [Google Scholar | PubMed]
- 19.Xu Y, Wang Y, Yan J, Bai X, Xing G. Desmoplastic fibroma of the femur with atypical image findings: A case report. Medicine (Baltimore) 2018;97:e13787. [Google Scholar | PubMed]
- 20.Siddiqui HK, Khan SA, Aijaz A, Qureshi MB. Unraveling the challenges in the diagnosis and management of desmoplastic fibroma of the mandible-a case report. BMC Oral Health 2024;24:256. [Google Scholar | PubMed]