In distal femur fracture treated with anatomical locking compression plate with anatomical reduction, rigid fixation, and early knee mobilization are the essential factors in achieving better outcome.
Dr. Arvind Kumar, Department of Orthopaedics, Parul Institute of Medical Sciences and Research, Parul University, P.O. Limda 391760, Tq. Vaghodia, Vadodara, Gujarat, India. E-mail: drakumar76@gmail.com
Introduction: Distal femur fractures are mostly caused due to vehicular injuries in the middle-aged population. Operative treatment has been preferred with open reduction and internal fixation in these fractures. Due to the availability of anatomical locking compression plates (LCPs), better results and improved functional outcomes have been observed. This study aims to observe the surgical outcome of distal femur fractures operated with an anatomical LCP.
Materials and Methods: A prospective study was carried upon 48 patients with 40 male and 8 female patients having fractures of the distal femur. The mean age of presentation was 40.6 years. Thirty of them had vehicular injuries and 18 had a history of fall. Open fractures were seen in 22 patients and associated ipsilateral limb injuries were seen in 16 and contralateral limb injuries were seen in 8 patients. The patients were treated with anatomical LCP. The lateral approach was used in all cases for my study.
Results: The mean follow-up in the present study was 6 months. All fractures were united with a mean union period of 18.2 weeks. At final follow-up, fixed flexion deformity was seen in 25% of the patients. There were 16 cases of infection with 2 being a superficial infection treated conservatively and 14 cases having a deep infection treated with debridement and antibiotics. 2 cases of nonunion, 4 cases of malunion and 4 cases of delayed union were observed. 16 cases develop joint stiffness. 16 cases also developed limb shortening and 10 had fixed flexion deformity and 8 had varus deformity. At the time of final follow-up through “SCHATZKER AND LAMBERT SCORING SYSTEM,” satisfactory outcomes were achieved in 50% (20.8%excellent and 29.2% good) of the patients.
Conclusion: Distal femur fracture treated with anatomical LCP needs careful anatomical reduction, rigid fixation and early knee mobilisation and weight bearing on signs of healing with an early presentation to the hospital from the time of injury were the essential factors in achieving better outcome for the patient.
Keywords: Distal femur anatomical plate, distal femur fracture, Schatzker and Lambert scoring system.
Fractures in the distal femur have posed considerable therapeutic challenges throughout the history of fracture treatment because they are usually comminuted, readily deformed because of muscle forces acting on the distal fragment, prone to result in functional impairment of the knee joint and ankle, because of injury to quadriceps system and often occur in elderly patients with osteoporosis. Distal femur fractures make up 6–7% of all femur fractures [1,2]. The most common high-energy mechanism of injury is a road traffic accident (53%) and the most common low-energy mechanism is a simple fall (33%) [3]. Treatment may vary from closed treatment with traction, application of cast brace following preliminary traction, open reduction and internal fixation with a variety of Implants [4]. Anatomical reduction of the articular surface, restoration of limb alignment, and early mobilisation have been shown to be effective ways of managing most distal femoral fractures [5]. Locking compression plate (LCP) has the advantage of the combination of compression platting, Locked platting and Bridge platting [6-8]. This reduces soft tissue damage and periosteal vessels are preserved. Therefore, it acts as a closed external fixator [9,10]. In this study, we are evaluating the results of distal femur fractures treated with distal femur anatomical LCP, their clinical, and radiological outcomes and complications.
The prospective study was carried out in the group of patients treated in the Department of Orthopaedics, Parul Sevashram Hospital, PIMSR, Parul University, Vadodara. 48 patients were included on the basis of inclusion and exclusion criteria from March 2021 to March 2024, after taking written and informed consent.
Inclusion criteria
- Patient aged 18 years and above
- The fractures of the distal femoral metaphyseal, metaphyseo-diaphyseal with or without intraarticular extension and distal third fractures of the femur
- Comminuted distal femur fracture
- Close fractures, fractures with Open Grade I wounds were also
Exclusion criteria
- Patients who don’t want to participate
- Patients under 18 years
- Patient medically unfit for surgery
- Fractures with open grades II and
Operative details
Under spinal/epidural anaesthesia, on a simple radiolucent operative table with the aid of image intensification in the supine position. A proximal thigh tourniquet was used. A small rolled towel is placed beneath the greater trochanter to improve the alignment of the leg by preventing external rotation. A bolster was kept under the knee to keep it in 30° flexion. After painting and draping of the limb, the tourniquet was inflated after elevating the limb for 5 min. Lateral/anterolateral approach was used for exposure of the fracture site. The lateral approach relies on an atraumatic elevation of the vastus lateralis from the lateral aspect of the distal femur, and a lateral arthrotomy for joint visualisation. Articular reduction and lateral plate application can both be achieved with the same approach. In addition, the the approach can be extended proximally as required. The approach can also be used without an arthrotomy if the articular surface is not fractured. Begin the skin incision in the mid-lateral line of the femoral shaft and curve it anteriorly over the lateral femoral condyle, towards the tibial tubercle. The proximal starting point for the skin incision depends on the most proximal extent of the fracture. Divide the iliotibial band (tract) in line with the skin incision. Incise the muscle fascia investing the vastus lateralis just anterior to the lateral inter-muscular septum and elevate the muscle fibers off the septum, working from distal to proximal. After adequate exposure and reduction fixation was achieved through a distal femur-locking anatomical plate. The goals of the first postoperative week were control of limb swelling, quadriceps muscle rehabilitation and active ankle motion. Antibiotics were continued till sutures were removed around in 10–12 days. Weight-bearing only was allowed until fracture consolidation. If stable fixation had not been obtained, a more cautious postoperative approach was followed, including the use of an externally controlled motion brace until healing was sufficient. All patients were followed up at 6-week intervals till signs of fracture union and subsequently at quarterly intervals. At the time of follow-up a thorough clinical evaluation was done for the severity of pain, healing of the wound, limb length discrepancy, deformity, knee range of motion and weight bearing, radiological signs of union were assessed. Implant status and status of the joint were also assessed on X-rays and accordingly, weight bearing was allowed. The results were rated on the basis of “SCHATZKER AND LAMBERT” scoring system for functional assessment as EXCELLENT, GOOD, FAIR and POOR results (SCHATZKER AND LAMBERT) (Table 1).

Forty-eight patients were included in this study. Closed, Open grade I injuries and polytrauma patients were included in this study. In our study patients were of age group between 21 and 70 years (Average age was 40.6 years). There was a male preponderance (5:1) in our study. The majority of the patients had a history of road traffic accidents or fall from height. In our study, we included both intraarticular and extraarticular fractures, among which 66.7% are intraarticular fractures (Fig. 1) and 33.3% are extraarticular fractures (Fig. 2). Both types of fractures are fixed with anatomical LCP (Fig. 3 and 4). In our study, there were 26 cases of closed injuries (54.2%) and 22 cases of open injuries (45.8%). In our study 38 (79.2%) patients were fixed as definitive treatment in the primary procedure and 10 (20.8%) patients were fixed as definitive treatment in the secondary procedure due to the presence of open injuries which was fixed with an external fixator in the primary procedure. In our study most common early complication was infection which was occurred in 16 patients (33.3%) in which 14 developed deep infection and 2 patients had superficial infection which was resolved within 10 days. Patients who had deep infections were treated with wound debridement before discharge. The average stay of hospitalization of our study was 18.8 days. The majority of the patients (58.3%) were mobilized from the knee joint with high sitting immediately after operative intervention rest all were given immobilisation splint for 4 weeks. All patients were discharged with non-weight-bearing. On long-term follow-up, 29.2% of patients (14 patients) had knee joint stiffness, 4 patients had malunion and 4 patients had delayed union. 2 patients had non-union on final follow-up. The average time of union in our study is 18.2 weeks. The majority of the fractures united between 15 and 20 weeks. In our study, 66.7% of patients (32) returned to their previous occupation while 12.5% of patients (6) had to change their occupation and 20.8% of patients (10) had unable to return their occupation. In our study, 32 patients had no complaints of pain, 8 had intermittent pain, 6 had pain with fatigue and 2 had pain with restricted function. In our study, only 2 patients had shortening >1.5 cm and 10 patients had fixed flexion deformity. The average degree of knee range of movement in our study was 100° (Fig. 5). 10 patients had <90° of range due to associated soft tissue injury and comminution at the fracture site. 66.7% (32) of our patients were able to walk without a limp and support on the final follow-up. 8 patients required some kind of support while walking. In our study, there were 50% satisfactory results (20.8% excellent, 29.2% good) and 50% unsatisfactory results (29.2% fair, 20.8% poor). In our study, out of a total of 48 patients, 26 (54.2%) patients had close fractures and 22 (45.8%) had open fractures (Gustillo-Anderson Gr-I type). Out of 26 (54.2%) close fractures, 8 patients had excellent results, 10 had good results, 6 had fair results, 2 had poor result at the final follow-up (Table 1). Out of 22 open fractures, 8 patients had poor results, 8 patients had fair result, 4 patients had good result, and 2 patients had excellent results.

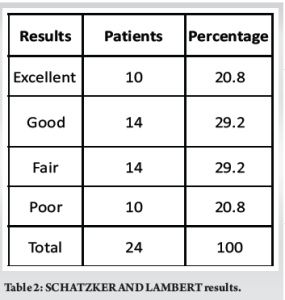
Fractures of the distal femur commonly involve a major weight-bearing joint (66.7%- intraarticular fractures) and henceforth result in functional impairment. To preserve a normal knee function, it is a must to maintain a normal mechanical axis, ensure joint stability and restore the full range of motion which is achieved by anatomical reduction and stable fixation. Open reduction internal fixation (ORIF) with LCP and closed reduction internal fixation (CRIF) with distal femur nail are two common surgical approaches for treating distal femur fractures. ORIF with LCP is ideal for complex, intra-articular, or comminuted distal femur fractures where precise anatomic reduction is needed, but it carries higher risks of infection and soft-tissue complications. CRIF with Distal Femur Nail is preferable for extra-articular or simple metaphyseal fractures, offering a minimally invasive approach with faster recovery but less control over complex fracture patterns. In our study, out of a total of 48 patients, 26 (54.2%) patients had close fractures and 22 (45.8) patients had open fractures out of which, 6 (25%) as compared with Vishwanath et al. [8] study 50 patients out of 22 (44%) open injuries and 28 (56%) closed fracture. No intra-operative complications were encountered in any of the patients. The most common early complication was an infection which occurred in 16 (33.3%) patients; in which 14 developed deep infections which required wound debridement as a secondary procedure and sensitive antibiotics, and 2 had superficial infection which was resolved within 10 days. Out of 16 infected cases, 12 cases were from open fractures and 4 from closed fractures. Our incidence of infection rate was comparable with other series such as Yeap and Deepak [9] (36.4%) but was significantly more as compared to Sabarisree [10] (8.3%), Vishwanath et al. (10%). The incidence of loss of movement is also huge in our study (33.3%). This is mainly due to the comminution of fractures and open injuries. Open injuries (45.8%) required multiple surgeries for soft tissue healing and late mobilization of the knee joint which result in reduced knee movements or fixed flexion deformity or extensor lag. The incidence of non-union in our study was 4.2% (2 cases) which is unusual to occur as compared to other studies of non-union. Malunion occurs in 8.4% (4 cases) as compared with the series of Yeap and Deepak (9.1%). In our study, no case of implant loosening or failure was found. The mean time for union in our study is 18.2 weeks (range of 15–20 weeks). The rate of union in our study was 95%. Partial weight bearing was started in our study at an average period of 14.2 weeks and full weight bearing was started at an average period of 17.7 weeks. In our study 66.7% (32) patients resume their previous occupation while 12.5% (6) patients had to change their occupation and 20.8% (10) patients were unable to resume their occupation. 32 (66.7%) of our patients were able to walk normally without limp and support, 8 (16.7%) with limp and 8 (16.6%) walks with the help of cane or crutches. 10 (21%) patients developed fixed flexion deformity. The incidence of fixed flexion deformity was slightly higher as compared to Sabarisree 3 (12.5%). It is mainly associated with the patients who don’t follow postoperative advice for physiotherapy or the patients who were having injury to the quadriceps mechanism. Using “SCHATZKER and LAMBERT ” 10 (20.8%) patients had excellent results, 14 (29.2%) cases had good results, and 14 (29.2%) cases had fair results. There were 10 (20.8%) cases with poor results in our study (Table 2). In Yeap and Deepak. study, there were 4 (36.4%) excellent results, 4 (36.4%) good results, 2 (18.2%) fair results, and 1 (9%) was a failure.
Distal femur fracture treated with anatomical LCP needs careful anatomical reduction, rigid fixation, early knee mobilization and weight bearing on signs of healing were the essential factors in achieving better outcome for the patient.
Anatomical LCP is a reliable surgical technique for treating Distal Femur Fractures, providing stable fixation and enabling early mobilization. This method achieves favourable functional outcomes, with good to excellent results even for complex or comminuted fractures.
References
- 1.Martinet O, Cordey J, Harder Y, Maier A, Buhler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury 2000;31 Suppl 3:C62-3. [Google Scholar | PubMed]
- 2.Crist BD, Rocca GJ, Murtha YM. Treatment of acute distal femur fractures. Orthopaedics 2008;31:681-90. [Google Scholar | PubMed]
- 3.Colling C, Wiss D. Rockwood and Green’s Fracture in Adults. 7th ed., Vol. 2. United States: Lippincott Williams and Wilkins; 2010. p. 1719-51. [Google Scholar | PubMed]
- 4.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Google Scholar | PubMed]
- 5.Ahmad M, Nanda R, Bajwa AS, Candal-Couto J, Green S, Hui AC. Biomechanical testing of locking compression plates: Is distance between bone and implant significant? J Bone Joint Surg 2007;88-B:401. [Google Scholar | PubMed]
- 6.Muller M, Allgoewer M, Schneider R, Willenegger H. Manual Der Osteosynthese AOTechnik. 3rd ed. Berlin, New York: Springer Verlag; 1992. [Google Scholar | PubMed]
- 7.Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma 2004;18:488-93. [Google Scholar | PubMed]
- 8.Vishwanath C, Harish K, Gunnaiah KG, Kumar C. Surgical outcome of distal femur fracture by locking compression plate. Int J Orthop Sci 2016;2:233-9. [Google Scholar | PubMed]
- 9.Yeap EJ, Deepak AS. Distal femoral locking compression plate fixation in distal femoral fractures: Early results. Malays Orthop J 2007;1:12-7. [Google Scholar | PubMed]
- 10.Sabarisree M, Jyothiprasanth M, Babu S, Sunku N. A study on functional outcome of comminuted supracondylar fracture femur treated by plating with fibular bone grafting. J Bone Rep Recomm 2017;3:5. [Google Scholar | PubMed]









