Intramedullary nailing and MIPO offer superior functional recovery and fewer complications compared to external fixation or conservative management in the treatment of distal tibia shaft fractures.
Dr. Mansi Gupta, Department of Microbiology, Government Bundelkhand Medical College, Sagar, Madhya Pradesh, India. E-mail: mansi1890@gmail.com
Introduction: Distal tibia shaft fractures pose significant treatment challenges due to limited soft tissue coverage and suboptimal vascularity in the region. Selecting the most appropriate management strategy – whether surgical or conservative – remains a subject of ongoing debate, particularly in resource-limited settings.
Materials and Methods: A prospective observational study was conducted at a tertiary care center in central India between October 2022 and April 2024, involving 70 skeletally mature patients with distal tibial shaft fractures. Patients were managed either conservatively or through surgical interventions, including intramedullary nailing (IMN), minimally invasive plate osteosynthesis (MIPO), or external fixation. Clinical outcomes were assessed at 6 weeks, 3 months, 6 months, and 12 months post-treatment using the Modified Johner and Wruhs criteria. Radiological union, weight-bearing progression, pain severity, and complication rates were also evaluated.
Results: The majority of patients (92.9%) underwent surgical treatment, with IMN being the most frequently used modality (46.2%), followed by MIPO (30.8%) and external fixation (23%). Conservative management was employed in 7.1% of cases. At the 12-month follow-up, full weight-bearing was achieved in 83.3% of IMN, 80% of MIPO, and a variable proportion of external fixation patients. Radiological union with more than three cortices was observed in 90% of IMN and 75% of MIPO patients by 12 months. Overall, excellent-to-good functional outcomes were achieved in 78.6% of cases. Superficial and deep infections, as well as non-union, were more common with external fixation.
Conclusion: IMN and MIPO demonstrated superior functional and radiological outcomes compared to external fixation and conservative methods. IMN, in particular, provided faster recovery with fewer complications, making it the preferred modality in appropriately selected cases.
Keywords: Tibial fractures, fracture fixation, external fixators, conservative treatment.
Fractures involving the distal third of the tibial shaft remain a significant therapeutic challenge due to the unique anatomical and biomechanical characteristics of this region. The distal tibia, being subcutaneous with limited muscular coverage and poor vascularity, is highly susceptible to soft tissue complications, delayed union, and infections following injury or surgical intervention. These factors necessitate careful consideration of treatment approaches to optimize functional and radiological outcomes [1,2]. Distal tibial fractures may extend into the articular surface, often termed tibial pilon or plafond fractures, particularly when intra-articular involvement is present. The most common mechanism of injury is high-energy trauma, notably road traffic accidents, accounting for the majority of cases in developing countries. Other causes include falls from height and direct impact injuries. The severity of soft tissue involvement, particularly in open fractures, further complicates treatment planning, increasing the risk of infection and poor wound healing following open reduction and internal fixation [3]. Conservative management is generally reserved for low-energy, closed, and minimally displaced fractures, or in patients who are unfit for surgery. However, conservative methods may lead to prolonged immobilization and associated complications such as joint stiffness, malunion, and delayed weight bearing. Various surgical modalities have been developed, each with distinct advantages and limitations [4]. Intramedullary nailing (IMN) is commonly used for extra-articular or simple intra-articular fractures, offering a biologically favorable, minimally invasive technique with early mobilization potential [5]. Minimally invasive plate osteosynthesis (MIPO) aims to preserve periosteal blood supply and fracture hematoma while providing angular stability through locking compression plates, particularly useful in comminuted and metaphyseal fractures [6]. External fixation serves as a temporary or definitive measure in cases of open fractures with extensive soft tissue damage (Gustilo-Anderson Grade III), enabling stabilization while allowing wound care [7]. Despite these advancements, the complication rate for distal tibia fractures remains high, with reported rates of infection, malunion, and non-union ranging from 20% to 30%. There is still no definitive consensus on the optimal modality for distal tibia shaft fractures, particularly when intra-articular extension or soft tissue compromise is present [8]. Previous studies have evaluated the functional and radiological outcomes of individual techniques such as MIPO, IMN, or external fixation, often with varied results [9,10]. Given this context, the present study was conducted with the objective of analyzing and comparing the functional and radiological outcomes of distal tibia shaft fractures managed by conservative methods, IMN, MIPO, and external fixation in a tertiary care setting in central India. The goal was to identify the most effective modality in terms of union rates, pain relief, complication profile, and functional recovery using standardized outcome measures.
Study design and setting
This study was a prospective observational investigation conducted at the Department of Orthopaedics, Government Bundelkhand Medical College, Sagar, Madhya Pradesh. The study duration extended from October 2022 to April 2024, and it aimed to assess and compare the functional and radiological outcomes of distal tibia shaft fractures treated using various modalities, including surgical and conservative approaches.
Sample size and participant selection
During the study period, a total of 82 patients presenting with distal tibial fractures were screened for eligibility. After excluding 12 patients who declined to participate or failed to meet inclusion criteria, 70 patients were enrolled in the final study cohort. Patients were included if they were skeletally mature and presented with a fracture involving the distal third of the tibia, including those with associated fibular fractures or malleolar involvement. Both closed and open fractures were considered, and all patients were required to provide informed written consent. Exclusion criteria included skeletally immature individuals, mid-shaft or proximal tibial fractures, pathological fractures, and unwillingness to participate.
Clinical evaluation and classification
A detailed history was recorded for each patient, including the mechanism of injury, comorbid conditions, and prior treatments. A thorough clinical examination was conducted, with special attention to the vascular and neurological status of the affected limb. Radiographic evaluation included anteroposterior and lateral X-rays of the tibia and ankle to assess the fracture pattern, comminution, displacement, and intra-articular extension. Open fractures were graded according to the Gustilo-Anderson classification.
Treatment modalities
Management strategies were selected based on the fracture characteristics, soft tissue condition, patient fitness for anesthesia, and surgeon’s clinical judgment. Patients were treated either conservatively or with surgical intervention. Conservative management was reserved for patients with stable, closed fractures or those who were unfit or unwilling for surgery. These patients were treated with above-knee cast immobilization and monitored with periodic clinical and radiological assessments. Surgical management included IMN, MIPO, or external fixation. IMN was performed under spinal anesthesia using a midline patellar tendon-splitting approach. After entry point creation and guidewire placement, sequential reaming was done followed by insertion of a pre-measured interlocking nail. Locking screws were placed proximally and distally to ensure stability. For MIPO, patients were positioned supine, and an anatomical locking compression plate was inserted submuscularly through a limited incision made on the medial side of the distal tibia. Closed reduction techniques were used wherever possible to minimize soft tissue disruption. Fixation was achieved using cortical and locking screws through stab incisions, and care was taken to preserve the periosteum and fracture hematoma. External fixation was applied in patients with 00III fractures or significant soft tissue damage. Delta frame constructs were used, involving the placement of Schanz pins on either side of the fracture connected through external rods and clamps to stabilize the limb. These were either definitive or temporary, with subsequent conversion to internal fixation after soft tissue recovery.
Post-operative care and follow-up
Post-operative care included analgesia, elevation of the limb, and suture removal around day 11. Weight-bearing was initiated based on radiographic evidence of union and patient tolerance. Typically, partial weight-bearing was started between 8 and 10 weeks in nailing and external fixator groups, and between 12 and weeks in the MIPO group. Patients were followed at 6 weeks, 3 months, 6 months, and 12 months post-treatment. At each visit, clinical evaluation included assessment of range of motion, deformity, limb length, gait, pain severity, and patient satisfaction. The radiological union was assessed through standard views, with outcomes categorized using the Modified Johner and Wruhs criteria. Delayed union was defined as a lack of radiographic union by 26 weeks, and non-union was considered if the union was not evident by 9 months.
Data analysis
Data were recorded in structured pro formas and entered into Microsoft Excel. Statistical analysis was performed using the Statistical Packages for the Social Sciences version 26. Descriptive statistics were used to summarize data. Categorical variables were presented as frequencies and percentages, while continuous variables were expressed as mean ± standard deviation. A P < 0.05 was considered statistically significant.
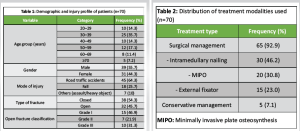
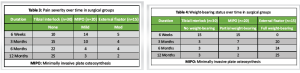
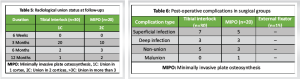
In this prospective observational study, we compared the functional outcomes of surgical and conservative management in patients with distal tibia shaft fractures. A total of 70 patients were enrolled in the study, with a predominance of males (55.7%) over females (44.3%). The age distribution was skewed toward younger adults, with 35.7% of patients falling within the 30–39 years age group. The majority of fractures were caused by road traffic accidents (64.3%), followed by falls (25.7%), and other causes, such as assault or heavy objects (10%). In terms of fracture type, 54.3% were closed fractures, while 45.7% were open fractures. Among the open fractures, Grade I was the most common (46.9%), followed by Grade III (31.3%) and Grade II (21.9%) (Table 1). Regarding the treatment modalities, a large proportion of patients (92.9%) underwent surgical management, with IMN being the most commonly used technique (46.2%). Other surgical interventions included minimally invasive percutaneous osteosynthesis (MIPO) in 30.8% and external fixator application in 23% of cases. Only 7.1% of patients received conservative management, reflecting the general preference for surgical intervention in these cases (Table 2). In terms of post-operative pain severity, the patients who underwent tibial interlock fixation experienced a gradual reduction in pain over time. At 6 weeks, 10 patients reported no pain, while 14 experienced mild pain and 5 had moderate pain. By 12 months, the majority of patients (25) had no pain, with only 3 reporting mild pain. Similar trends were observed in the MIPO and external fixator groups, although the incidence of pain was higher at the 6-week follow-up in these groups compared to the tibial interlock group (Table 3). Weight-bearing status also improved over time in all surgical groups. At 6 weeks, only 15 tibial interlock patients were able to bear partial weight, and no patients in the external fixator group could bear full weight. By 12 months, the vast majority of tibial interlock (25) and external fixator (25) patients were able to bear full weight. The MIPO group showed a similar improvement, with most patients bearing full weight by 12 months (Table 4). The radiological union was assessed at various follow-up points. At 3 months, 20 tibial interlock patients and 10 MIPO patients had a union in one cortex, while the remaining patients had a union in two or more cortices. By 12 months, union in at least one cortex was achieved in all patients, with more than half achieving union in two cortices in both groups (Table 5). Post-operative complications were noted in the surgical groups. The most common complications in the tibial interlock group were superficial infections (7 patients) and non-union (5 patients). In the MIPO group, 5 patients developed superficial infections, and 3 patients experienced non-union. No complications were reported in the external fixator group (Table 6). Finally, the final functional outcomes, assessed by the Johner and Wruhs criteria, showed a significant difference between surgical and conservative management. The tibial interlock group had the highest number of excellent (16) and good (10) outcomes, while the MIPO group also had a relatively high proportion of excellent outcomes (12). The external fixator group had a greater proportion of fair and poor outcomes compared to the other groups. Overall, surgical management led to a higher proportion of excellent and good outcomes (55%) compared to conservative treatment, which had only 7.1% of patients achieving good outcomes (Table 7).

Distal tibial shaft fractures are complex injuries due to the subcutaneous location of the tibia, poor vascularity, and the frequent involvement of soft tissues. These factors contribute to delayed healing, higher infection rates, and variable functional outcomes, regardless of the treatment modality used. The goal of management in such fractures is to achieve stable fixation, promote early mobilization, minimize complications, and restore limb function as close to normal as possible [11]. In the present study, most cases were attributed to road traffic accidents (64.3%), reflecting the high incidence of high-energy trauma in developing countries. This trend is consistent with previous literature, where motor vehicle accidents were identified as the predominant cause of distal tibial fractures [12]. Male predominance in our cohort (55.7%) also aligns with similar studies, likely due to increased exposure to outdoor activities and occupational hazards [12]. Surgical management was preferred in 92.9% of cases in this study, highlighting a clinical shift toward operative fixation even in borderline cases, largely due to improved surgical techniques and implants. Among surgical modalities, IMN was most commonly used (46.2%), followed by MIPO and external fixation. IMN was associated with better early functional recovery and fewer complications. These findings corroborate the results of Sagar et al., who found high union rates and excellent modified Lysholm scores following IMN using the suprapatellar approach [13]. MIPO, chosen in 30.8% of surgical cases, also demonstrated favorable outcomes in terms of pain reduction, radiological union, and restoration of function. This is supported by Illur et al. [14], who reported a mean AOFAS score of 84.45 and predominantly excellent to good results in patients treated with MIPO, attributing these outcomes to minimal disruption of periosteal blood supply and better preservation of soft tissues. Similarly, Kang et al. highlighted the advantages of MIPO in achieving reliable union and maintaining alignment with low complication rates [15]. External fixation was primarily used in open fractures with significant soft tissue damage. Although it facilitated early stabilization, complications such as pin tract infections and delayed union were more frequent. Our findings align with those of Giannoudis et al., who noted prolonged union times and higher complication rates with external fixation, especially in high-grade open fractures [16]. Similarly, Joveniaux et al. suggested that external fixation should be reserved for severe soft tissue injuries or as a temporary stabilization measure, as it was associated with poorer functional scores and higher rates of malunion and infection compared to internal fixation [2]. The radiological union was assessed using cortical bridging. At 12 months, 90% of IMN cases and 75% of MIPO cases achieved union in more than three cortices, supporting the biological advantages of both methods. This finding is in agreement with Li et al. [17], who found comparable union times among IMN, MIPO, and external fixation groups, but reported higher implant-related complications in plating and anterior knee pain in nailing. Regarding functional outcomes, excellent-to-good results were seen in 78.6% of all patients, with IMN and MIPO outperforming other methods. These outcomes are similar to those reported by Leonard et al., who demonstrated favorable results with early minimally invasive fixation in complex fractures [18]. The present study demonstrates that IMN and MIPO offer superior outcomes in terms of pain relief, earlier weight-bearing, radiological union, and fewer complications. Conservative treatment and external fixation are better reserved for selective cases, particularly those with comorbidities or severe soft tissue injuries. However, individual patient factors, fracture morphology, and resource availability should guide the final treatment decision.
Limitations
This being a single-center study, the findings may not be broadly generalizable. However, the patient cohort represents a varied demographic reflective of typical cases managed at tertiary care facilities in the region. Nevertheless, multicentric trials are warranted to enhance external validity. As an observational study, treatment allocation was not randomized but guided by clinical criteria, which may introduce selection bias. Nonetheless, this approach mirrors real-world clinical practices and may enhance clinical applicability. The conservative management group was small, reflecting its limited indication in distal tibial shaft fractures. This limits the statistical strength of comparative analysis and outcome interpretation for this subgroup. The heterogeneity of fracture patterns (closed/open, simple/comminuted, intra-articular) adds variability to outcomes. The 12-month follow-up may not sufficiently capture late complications, such as post-traumatic arthritis, hardware failure, or long-term functional status. Future studies should include longer-term surveillance. Potential confounders such as comorbidities (diabetes, smoking), body mass index, and rehabilitation adherence were not controlled in the analysis, which may have influenced outcomes. Prospective studies with matched or stratified designs are recommended. Blinding of patients and assessors was not possible due to treatment visibility, potentially introducing performance and assessment bias. To reduce variability, a standardized scoring protocol and consistent assessors were used. Cost analysis, including implant cost, hospitalization, and rehabilitation, was not performed but is an important consideration for policy-making, especially in low-resource settings. Although open injuries were recorded, a detailed classification of soft tissue severity (e.g., Gustilo-Anderson subtypes) was not consistently applied in outcome analysis. The inclusion of structured grading systems is recommended in future studies. The radiological union was assessed using standard criteria (bridging of three cortices), but the interobserver agreement was not evaluated. In addition, advanced imaging, such as computed tomography was not routinely employed to assess non-union.
Distal tibial shaft fractures present significant management challenges due to the anatomical and biomechanical characteristics of the region. In this prospective observational study, IMN and MIPO demonstrated superior outcomes in terms of early pain resolution, faster radiological union, improved weight-bearing progression, and lower complication rates compared to external fixation and conservative treatment. IMN, in particular, was associated with the most favorable functional results. While external fixation remains a valuable option in managing high-grade open fractures with extensive soft tissue damage, and conservative treatment has a role in selected low-risk patients, surgical fixation should be considered the preferred strategy for most distal tibia shaft fractures. Treatment choice should, however, remain individualized based on fracture pattern, soft tissue status, and patient-specific factors.
Distal tibial shaft fractures require a carefully tailored approach due to their subcutaneous location and high risk of complications. This study reinforces that IMN and MIPO provide better functional and radiological outcomes compared to external fixation or conservative treatment. Surgical fixation allows earlier mobilization, faster union, and fewer complications when soft tissue conditions permit. Clinicians should prioritize individualized treatment planning based on fracture configuration, patient condition, and available resources.
References
- 1.Thompson JH, Koutsogiannis P, Jahangir A. Tibia fractures overview. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/nbk513267 [Last accessed on 2023 Jul 31]. [Google Scholar | PubMed]
- 2.Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, et al. Distal tibia fractures: Management and complications of 101 cases. Int Orthop 2010;34:583-8. [Google Scholar | PubMed]
- 3.Bister V, Lenkkeri T, Parkkinen M, Lindahl J. Intra-articular distal tibial fractures cause a major burden to individual patients and also stresses the public health care system. Injury 2022;53:2888-92. [Google Scholar | PubMed]
- 4.Raju K, Smith TO, Hing CB, Solan MC, Nielsen DM. Surgical versus conservative interventions for treating tibial shaft fractures in adults. Cochrane Database Syst Rev 2018;2018:CD011095. [Google Scholar | PubMed]
- 5.Kashyap S, Ambade R, Landge S, Salwan A. Impact of surgical timing on fracture healing in tibial shaft injuries: A comparative review of intramedullary nailing techniques. Cureus 2024;16:e70978. [Google Scholar | PubMed]
- 6.Andalib A, Sheikhbahaei E, Andalib Z, Tahririan MA. Effectiveness of minimally invasive plate osteosynthesis (MIPO) on comminuted tibial or femoral fractures. Arch Bone Jt Surg 2017;5:290-5. [Google Scholar | PubMed]
- 7.Hannigan GD, Pulos N, Grice EA, Mehta S. Current concepts and ongoing research in the prevention and treatment of open fracture infections. Adv Wound Care (New Rochelle) 2015;4:59-74. [Google Scholar | PubMed]
- 8.Tamburini L, Zeng F, Neumann D, Jackson C, Mancini M, Block A, et al. A review of tibial shaft fracture fixation methods. Trauma Care 2023;3:202-11. [Google Scholar | PubMed]
- 9.Polat A, Kose O, Canbora K, Yanık S, Guler F. Intramedullary nailing versus minimally invasive plate osteosynthesis for distal extra-articular tibial fractures: A prospective randomized clinical trial. J Orthop Sci 2015;20:695-701. [Google Scholar | PubMed]
- 10.Elnewishy A, Elkholy M, Hamada A, Salem M. Comparing minimally invasive percutaneous plate osteosynthesis with interlocking intramedullary nail fixation for the management of adult extra-articular distal tibial fractures: A comprehensive systematic review and meta-analysis. Cureus 2023;15:e49214. [Google Scholar | PubMed]
- 11.Vasantharaman R, Devendran R, Ashok L. Outcome analysis of distal tibial fractures managed by open reduction internal fixation using plate osteosynthesis. Int J Sci Stud 2019;6:142-5. [Google Scholar | PubMed]
- 12.Mwafulirwa K, Munthali R, Ghosten I, Schade A. Epidemiology of open tibia fractures presenting to a tertiary referral centre in Southern Malawi: A retrospective study. Malawi Med J 2022;34:118-22. [Google Scholar | PubMed]
- 13.Sagar BV, Nandi SS, Kulkarni SR, Bagewadi R. Functional outcomes of tibia fractures treated with intramedullary interlocking nails by suprapatellar approach: A prospective study. Cureus 2023;15:e40485. [Google Scholar | PubMed]
- 14.Illur V, Patil RS, Shah J, Chaudhary N, Bhosale V. Functional outcome of distal tibia fracture treated with locking compression plate using minimally invasive percutaneous plate osteosynthesis technique (MIPPO): A prospective study. Int J Orthop Sci 2019;5:980-4. [Google Scholar | PubMed]
- 15.Kang H, Song JK, Rho JY, Lee J, Choi J, Choi S. Minimally invasive plate osteosynthesis (MIPO) for mid-shaft fracture of the tibia (AO/OTA classification 42): A retrospective study. Ann Med Surg (Lond) 2020;60:408-12. [Google Scholar | PubMed]
- 16.Giannoudis VP, Ewins E, Taylor DM, Foster P, Harwood P. Clinical and functional outcomes in patients with distal tibial fracture treated by circular external fixation: A retrospective cohort study. Strategies Trauma Limb Reconstr 2021;16:86-95. [Google Scholar | PubMed]
- 17.Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A. Treatment of distal tibial shaft fractures by three different surgical methods: A randomized, prospective study. Int Orthop 2014;38:1261-7. [Google Scholar | PubMed]
- 18.Leonard M, Magill P, Khayyat G. Minimally-invasive treatment of high velocity intra-articular fractures of the distal tibia. Int Orthop 2009;33:1149-53. [Google Scholar | PubMed]