The Sequential Rod Rolling (SRR) technique is a safe and effective technique to correct Lenke 2 curves and allows a significant amount of AVR derotation and angular correction. A comparative prospective study would be useful for a full evaluation of this technique.
Dr. Jérémie Nallet, Department of Pediatric Orthopaedics, CHU de Besançon Hôpital Jean Minjoz, Besançon 25030, France. E-mail:Jeremie.nallet@sfr.fr
Introduction: Many options have been described to restore balance and create stable fusion in severe adolescent idiopathic scoliosis (AIS), including preoperative gravity halo traction, posterior vertebral column resection, and three column osteotomies. Unfortunately, each of these comes with risks of excess bleeding or neurological injury. The sequential rod rolling (SRR) technique uses a short stiff rod to distract and derotate the main thoracic (MT) curve, followed by a second full length rod on the opposite side to distract and derotate the proximal thoracic (PT) curve and finally a short rod on the convexity of the PT to offer a controlled correction of rigid deformities. The aim of this investigation is to describe the technique, its indications, the rotational correction achieved, and the complications observed when it is used in the treatment of severe pediatric AIS.
Materials and Method: A retrospective study was carried out to include all patients treated with SRR to manage a Lenke 2 curve between 2006 and 2018, in whom a 3D EOS reconstruction was available. The primary objective of this study was to measure the derotation of the apical vertebra of the PT achieved by the sequential rod technique. The secondary objectives include defining the morbidity and complications observed.
Results: Sixteen patients with a mean age of 15 years were included. The mean pre-operative coronal angular deformity was 53° for the PT and 76° for the MT. The mean post-operative coronal angular deformity was 19° for the PT, 22° for the MT. The mean rotation preoperatively was 10° for the apical vertebra of the PT and 23° for the MT. The mean rotation postoperatively was 3° for the apical vertebra of the PT and 8° for the MT. Twelve patients had a 2-year post-operative follow-up. No proximal junctional kyphosis or complications were reported at the 2-year follow-up.
Conclusion: This data show that SRR achieves a mean coronal PT correction of 66% and 72% for the MT curve. The average derotation is 7° for the PT and 15° for the MT. No complications were encountered. The SRR technique for Lenke 2 type AIS seems to be a safe and effective technique.
Keyword: Adolescent idiopathic scoliosis, Lenke 2, rolling technique
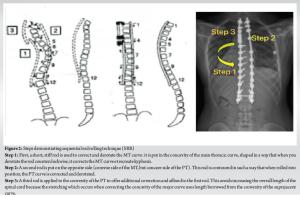
Adolescent idiopathic scoliosis (AIS) is a common diagnosis, affecting an estimated 3% of the adolescent population. Defined as a coronal deformity exceeding 10°, AIS is classified using the Lenke classification, which categorizes deformities into 6 groups and describes which motion segments should be fused during surgical correction [1]. A type 2 deformity is defined by a structural proximal thoracic (PT) minor curve with a main thoracic (MT) major curve. There are many options for correcting the deformity and creating the mechanical conditions amenable for fusion, including preoperative halo gravity traction, intraoperative traction or osteotomy [2-8]. Unfortunately, each of these comes with risks of prolonged inpatient stay, neurological injury, excess bleeding, or all three. The sequential rod rolling (SRR) technique was first described by Cotrel and Dubousset in 1993 [9]. SRR seeks to overcome the risk of correcting severe deformity by applying the corrective force to the spine through rotating the rods. Rod rolling preserves the overall length of the spinal column whilst correcting the deformities and does not require entry into the canal. This prevents stretching of neural elements and removes the opportunity for direct injury to the spinal cord; thus, it is associated with a lower risk of injury when compared to other corrective techniques [10]. In SRR, each curve is treated independently whilst preserving the final construct of 2 rods. The first step in SRR uses a short, stiff rod to correct and derotate the MT curve. This is followed by the second rod on the opposite side. This rod is contoured in such a way that when rolled into position, the PT curve is corrected and derotated. Finally, a third rod is applied to the convexity of the PT to offer additional correction and affixed to the first rod. This avoids increasing the overall length of the spinal cord because the stretching which occurs when correcting the concavity of the major curve uses length borrowed from the convexity of the suprajacent curve. Although the technique has been in use since the early 1990s, there have been no analyses which describe the results and complications associated with using SRR. The aim of this investigation is to describe the technique, its indications, the rotational correction achieved, and the complications observed when it is used in the treatment of severe Lenke type 2 AIS in a pediatric population.
Institutional research ethics board approval was obtained (REB no:1000074727). A retrospective radiographic analysis and case note review were carried out on pediatric patients treated for a Lenke 2 scoliosis with posterior spinal fusion by a single surgeon at a single institution using SRR. Inclusion criteria comprised age <18 years at the time of surgery, with an assessment with EOS radiography. The exclusion criteria comprised patients treated with other surgical techniques. Radiographic data were acquired using the EOS imaging system (EOS imaging SA, Paris, France). EOS produces biplanar anteroposterior and lateral X-ray images of the whole body in a standing position. The system was in use from 2009 in our institution. Using the STEREOS software, a 3D reconstruction of the T1 to the pelvis is created, which allows for automatic computation of the apical vertebrae rotation (AVR). Measurement of the AVR of the PT and MT, the coronal and sagittal angular deformity (using the Cobb method), sagittal alignment, pelvic tilt, and sacral slope were recorded preoperatively and postoperatively at 6 weeks and at final follow-up. Each measurement was made twice by a fellowship-trained spine surgeon independent of the operative team at different time points 2 months apart. Demographic data, details of the operative strategy, post-operative recovery, and complications were recorded. Distal adding-on was also recorded, as was proximal junctional kyphosis. Distal adding on was defined as a progressive increase in the number of vertebrae included within the primary curve distally combined with either an increase of more than 5 mm in the deviation of the first vertebra below the instrumentation from center sacral vertical line or an increase of more than 5° in angulation of the first disc below the instrumentation. Proximal junctional kyphosis was defined by two criteria: a proximal junctional sagittal Cobb angle ≥10° and at least 10°< the preoperative measurement [11].
Surgical technique
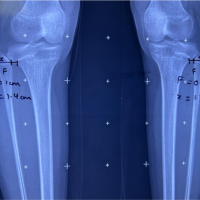
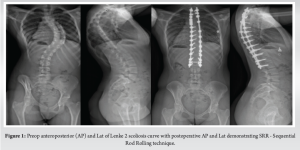
Intra-operative skull-femoral traction was used in all patients. Gardner-Wells tongs and distal femoral pins were placed, and traction was applied with 13lbs weight on the head and 26 lbs weight on the legs. After the exposure, uniaxial pedicle screws were inserted in all pedicles, with hooks at the upper instrumented vertebra. The SRR technique, when applied to Lenke 2 curves, utilizes a shorter stiff rod across the concavity of the MT curve, to apply focal distraction and derotation to the apex before placing a full-length rod on the contralateral side to achieve focal distraction and derotation of the upper thoracic curve. Finally, a short rod is placed on the convexity of the PT curve to restore a symmetric construct (Fig. 1 and 2).
Statistical analysis
Demographic data, including sex, age, and date of surgery, were recorded. For intrarater reliability analysis, all the 3D reconstructions have been done twice on month apart and reliability assessed with a Kappa correlation. A Wilcoxon Rank-sum test was carried out to compare the differences in pre- and post-operative angular deformity.
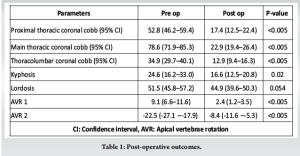
Thirteen females and three males were included in the analysis. The mean age at the operation was 14, 6 years old (range 11–18 years). The mean pre-operative MT was 76.4° ( range 57°–103°). The mean pre-operative PT curve was 53.1° (range 31°–69°). The median number of vertebral levels fused was 13 (IQR 13–14). Mean follow-up was 29 months (range: 2 weeks–64 months), and 12 patients were followed >2 years. A total of 102 SterEOS 3D reconstructions were performed. The Kappa value was 1 for the assessment of Cobb angle and 0.94 for the average vertebrae rotation. The post-operative mean MT curve was 23° (range 10°–33°). The mean post-operative PT was 22° (range, 1°–31°). At the last follow-up the mean MT curve was 21° (range 8°–43°) and the mean PT was 23° (range 0°–30°). AVR was recorded as a positive value if the vertebral body is rotated toward the right. Thoracic major curves are typically associated with positive AVR, whereas upper thoracic curves are associated with negative AVR. Preoperatively, the mean AVR was 23° toward the right (standard deviation [SD] = 7.4; range 8°–36°) for the MT and 10° toward the left (SD = 5.2; range 4°–17°) for the PT. Postoperatively, the mean AVR was 8° toward the right (SD = 5.5; range 0°–17°) for the MT and 3° toward the left (SD = 2.12; range 0°–8°) for the PT. At the last follow-up, the AVR for the MT was 5° toward the right (SD = 5.4°; range 0°–14°) and 4° toward the left for the PT (SD = 3°; range 1°–12°). The mean postoperative Cobb angle correction was 54° (P < 0.005) for the MT and 34° (P < 0.005) for the PT on immediate postoperative images and was 55° (P < 0.005) for the MT and 30° (P < 0.005) for the PT at the last follow-up. The mean post-operative AVR correction was 15° (P < 0.005) for the MT and 7° (P < 0.005) for the PT on immediate post-operative images and was 18° (P < 0.005) for the MT and 6° (P < 0.005) for the PT at the last follow-up (Table 1 and 2). The mean pelvic incidence was 51.1° preoperatively (range: 32.5–66.9) and 52.5° (range: 46.7–58.3°) postoperatively (P = 3.69). On closer analysis, it was noted that 2 patients increased their pelvic incidence by 11° and 1 patient by 6°. In the present study, no neurologic post-operative complications have been reported. There was no adding on, and no proximal junction kyphosis noticed at the last follow-up.

The aim of our study was to describe the ability of the SRR technique to correct the rotation of the AVR in Lenke 2 curves, and the complications observed. The data show that there is a significant change in the AVR and coronal Cobb angle after surgical correction of scoliosis, with a low incidence of complication. The data show a mean coronal PT correction of 66%, and 72% for the MT curve. The average derotation was 7° for the PT and 15° for the MT. To our knowledge, this is the only study in the literature that describes the SRR with the benefit of 3D reconstruction to assess AVR after the correction of Lenke 2 type AIS. The advantage of the analysis of 3D EOS reconstruction is the repeatability of vertebral rotation measurement. This is because of the referential system, which is based on each patient’s individual bilateral acetabular center line, which is not modified by the surgical correction. Furthermore, the accuracy of EOS has been investigated by several authors [12-14] who report that the measurement of angular and rotational deformity in scoliosis patients is precise, with intrarater reliability reaching 0.97 in one instance [13]. In the present study, intrarater reliability reached 1, supporting these previous findings. The AVR corrected by 70% in the PT curve and 65% in the MT, which was a slightly higher than the correction observed by others [15-17]. The coronal Cobb angle was corrected by 66% in the PT and 72% for the MT, which exceeds the correction found in the literature [18,19]. Our study did show some outliers in the correction of the AVR. Postoperatively, 7 patients (43%) had a residual AVR exceeding 10° (range 10°–17°). Although the reason for this is not clear from these data, all of these patients had an important pre-operative vertebrae rotation, more than 25° (range, 25°–36°) for a mean AVR of 10°. Furthermore, there is an improvement in AVR from the postoperative assessment to final follow-up of 3° (P = 0.57), and a slight loss of correction for the PT of 2° (P = 0.22), although those results failed to reach statistical significance. Three cases (18.7%) showed an increase in pelvic incidence postoperatively, 2 by 11°, and 1 by 6°. Out of these 3 patients, 2 had a low PI preoperatively (33.9° and 45.6°). A reasonable hypothesis could be that these patients adapt their PI to maintain a postural alignment [20]. In these cases, the PI changed most significantly in those patients with the largest observed deformities, for the first patient the Cobb angle was 51° for the PT and 85° for the MT, and 63° and 85° for the second patient. This observation has already been highlighted in the study of Skalli et al. [21] and recently by Manzetti et al. [22] in 2025 that the pelvic incidence is not a static parameter as a traditional belief but can change postoperatively. In a single case, the pre-operative PI was measured as 65.6° which increased to 76° despite surgery. No explanation presents itself to explain this; the patient was 12 years old at surgery and had 51° of lumbar lordosis between L1 and L5 and 58° between L1 and S1. Postoperatively, the LL was reduced to 36° with the lumbosacral lordosis remaining unchanged at 59°. It may be that surgery reduced the LL, requiring an increase in PI to maintain overall sagittal alignment. Although we found that the SRR technique was quite powerful in terms of correction, this study has some limitations. The number of patients is limited due to the infrequent presentation of severe Lenke 2 curves; this does not allow generalizable conclusions to be drawn. Second, the methodology is retrospective without a control group. A randomized controlled design study, including clinical scores, would be necessary for full assessment of this technique compared to other techniques like translation or direct derotation.
These findings suggest that the SRR (Sequential Rod Rolling) technique is a safe and effective technique to correct Lenke 2 curves and allows a significant amount of AVR derotation and angular correction. A comparative prospective study would be useful for a full evaluation of this technique.
SRR (Sequential Rod Rolling) technique is a safe and effective technique to correct Lenke 2 curves and allows a significant amount of AVR derotation and angular correction.
References
- 1.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;83:1169-81. [Google Scholar]
- 2.Kato S, Debaud C, Zeller RD. Three-dimensional EOS analysis of apical vertebral rotation in adolescent idiopathic scoliosis. J Pediatr Orthop 2017;37:e543-7. [Google Scholar]
- 3.Ould-Slimane M, Hossein Nabian M, Simon AL, Happiette A, Julien-Marsollier F, Ilharreborde B. Posterior vertebral column resection for pediatric rigid spinal deformity. Orthop Traumatol Surg Res 2020;108:102797. [Google Scholar]
- 4.Lewis ND, Keshen SG, Lenke LG, Zywiel MG, Skaggs DL, Dear TE, et al. The deformity angular ratio: Does it correlate with high-risk cases for potential spinal cord monitoring alerts in pediatric 3-column thoracic spinal deformity corrective surgery? Spine (Phila Pa 1976) 2015;40:E879-85. [Google Scholar]
- 5.Bridwell KH, Kuklo TR, Lewis SJ, Sweet FA, Lenke LG, Baldus C. String test measurement to assess the effect of spinal deformity correction on spinal canal length. Spine (Phila Pa 1976) 2001;26:2013-9. [Google Scholar]
- 6.Patel A, Ruparel S, Dusad T, Mehta G, Kundnani V. Posterior-approach single-level apical spinal osteotomy in pediatric patients for severe rigid kyphoscoliosis: Long-term clinical and radiological outcomes. J Neurosurg Pediatr 2018;21:606-14. [Google Scholar]
- 7.Wang XB, Lenke LG, Thuet E, Blanke K, Koester LA, Roth M. Deformity angular ratio describes the severity of spinal deformity and predicts the risk of neurologic deficit in posterior vertebral column resection surgery. Spine (Phila Pa 1976) 2016;41:1447-55. [Google Scholar]
- 8.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:2040-8. [Google Scholar]
- 9.De Giorgi G, Stella G, Becchetti S, Becchetti S, Martucci G, Miscioscia D. Cotrel-Dubousset instrumentation for the treatment of severe scoliosis. Eur Spine J 1999;8:8-15. [Google Scholar]
- 10.Sud A, Tsirikos AI. Current concepts and controversies on adolescent idiopathic scoliosis: Part I. Indian J Orthop 2013;47:117-28. [Google Scholar]
- 11.Tambe AD, Panikkar SJ, Millner PA, Tsirikos AI. Current concepts in the surgical management of adolescent idiopathic scoliosis. Bone Joint J 2018;100-B:415-24. [Google Scholar]