Inferior Hip Dislocation is a very rare condition and is to be treated as an emergency. Closed reduction is a successful treatment and consideration of pelvic organ injury status is a must
Dr. Nikhil Relwani, Department of Orthopaedics, Maharishi Markandeswar Institute of Medical Sciences and Research, Maharishi Markandeswar Deemed University, Ambala, Haryana - 133207, India. E-mail: drnikhilrelwani@gmail.com
Introduction: Inferior hip dislocation, also known as luxatio erecta femoris, is a rare condition where the femoral head dislocates downward from the acetabulum, typically due to high-energy trauma, such as motor vehicle accidents or falls. We describe a case of Inferior hip dislocation managed by closed reduction.
Case Report: A case of inferior dislocation of the hip is described. The case involves a 60-year-old male patient who was brought to the emergency department following a fall from height with pain and externally rotated left lower limb with 70° flexion at left hip joint and 90° flexion at left knee joint. Patient was thoroughly examined and vitally stabilized, followed by X-ray of pelvis with bilateral hips. The X-ray was suggestive of an inferior dislocation of the left hip. Closed reduction under short-duration general anesthesia was done. Adequate reduction was achieved and the patient was followed up.
Conclusions: Inferior dislocation of the hip is a rare dislocation of the hip. Treatment with closed reduction under anesthesia is an easy and safe method.
Keywords: Hip dislocation, luxatio erecta femoris, closed reduction.
Inferior dislocation of the hip, also known as luxatio erecta femoris or infracotyloid dislocation, is a rare and distinct subtype of anterior hip dislocation. It is most often associated with high-energy trauma and typically presents in the setting of significant force applied to a flexed, abducted hip [1]. Most hip dislocations are caused by high-energy mechanisms, with inferior dislocations accounting for approximately 5% of all traumatic hip dislocations [2]. These injuries are uncommon but frequently occur in association with fractures of the femoral head or neck [3]. The mechanism often involves axial loading, such as during falls from a height, leading to a characteristic position of the femur—typically nearly perpendicular to the spine—on radiographs [4]. One of the earliest descriptions of this injury emphasized its unique clinical and radiographic presentation [5]. Though most cases occur in adults, pediatric presentations have also been reported, reinforcing the need for awareness across age groups [6]. This dislocation pattern is often misclassified, and its recognition is crucial for appropriate management [7]. The term luxatio erecta reflects the abnormal vertical orientation of the femur seen in these cases [8]. Isolated traumatic hip dislocations, including the inferior subtype, can present management challenges and may be associated with long-term functional limitations [9]. Radiographic evaluation remains essential, with findings typically showing a dislocated femoral head and the long axis of the femur angled sharply relative to the spine [10].
A 60-year-old male patient was brought to the emergency room following an alleged history of a fall from 10 feet height following which the patient sustained injury to the left hip. Patient was conscious, oriented, and vitally stable (Glasgow Coma Scale- 15/15, blood pressure- 130/90 mm of Hg, Pulse- 88 bpm, respiratory rate- 20/min, SpO2– 99% on room air). The patient was thoroughly examined in the emergency room for any other systemic injuries. The patient was lying supine with left hip in 70° flexion, left knee in 90° flexion, and left lower limb in external rotation (Fig.1).
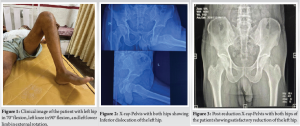
Patient was given intravenous analgesics and fluid support and shifted to the X-ray room, where X-ray revealed an inferior hip dislocation left side (Fig. 2).
The patient was taken to the emergency operation theatre and closed reduction under short-duration general anesthesia was done by giving sustained traction toward the head, followed by gradually extending the thigh with internal rotation at the hip joint. Following reduction Left lower limb was immobilized using a long knee immobilizing brace. Patient was taken to the X-ray room and reduction was confirmed (Fig. 3).
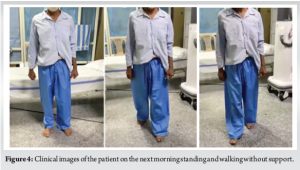
Patient was admitted and IV analgesics were given. Ultrasound of the abdomen and pelvis was done to rule out any internal organ injury, which was noted as normal. The patient was allowed full weight bearing and independent ambulation on the next morning and discharged (Fig. 4). Patient came for follow-up at 2 weeks, 1 month, 3 months, and 6 months. The patient continued to ambulate unassisted without any pain or limp. X-rays done were reported normal.
Inferior dislocation of the hip is an uncommon orthopedic emergency, accounting for less than 10% of all hip dislocations and typically resulting from high-energy trauma such as falls from height or road traffic accidents. Yeganeh et al. (2022) presented a case of a 60-year-old man with an inferior hip dislocation successfully managed with closed reduction, emphasizing the rarity of the condition and the importance of early recognition and reduction [1]. Jain et al. (2015) described a similar mechanism of injury, where the femoral head is driven anteroinferiorly toward the obturator foramen due to a force acting on the femur while the hip is flexed and abducted [2]. Their case also involved successful closed reduction and highlighted the importance of recognizing the atypical limb positioning that can lead to diagnostic confusion. Hani et al. (2015) reported a traumatic obturator-type hip dislocation and reinforced that prompt diagnosis and immediate reduction are essential for favorable outcomes [3]. Aggarwal et al. (2012), in a case series, underscored the need for post-reduction imaging to confirm concentric reduction and exclude intra-articular fragments [4]. Their work also suggested that most inferior dislocations could be managed conservatively if diagnosed early and if no associated fractures are present. Tekin et al. (2016) described a case of inferior dislocation after a fall from height and emphasized the significance of early intervention in preventing complications [5]. The earliest description of this dislocation subtype was by Mauck and Anderson (1935), who referred to it as “infracotyloid dislocation” and detailed the mechanism, clinical appearance, and management principles, which still hold relevance [6]. Kiel and Genova (2021) reported a pediatric case of inferior dislocation in a 16-year-old, managed nonoperatively with good recovery, and highlighted that inferior dislocations can occur across all age groups [7]. Rico and Barquet (1982) referred to this pattern as “luxatio erecta femoris” and provided radiographic evidence showing the femoral shaft in an extended and abducted position, which remains a classic diagnostic clue [8]. Yang et al. (1991) investigated long-term outcomes of traumatic hip dislocations and noted that even with anatomical reduction, avascular necrosis (AVN) of the femoral head can occur, particularly if reduction is delayed beyond six hours [9]. Dreinhöfer et al. (1994) echoed similar concerns, reporting AVN in approximately 10% of cases during long-term follow-up and emphasizing the importance of timely reduction and extended monitoring [10]. In summary, inferior hip dislocation remains a rare but clinically important condition. Recognition of its mechanism, immediate closed reduction, post-reduction imaging, and long-term vigilance for AVN are crucial for optimal outcomes.
Inferior hip dislocation is a rare type of hip dislocation and can be treated with close reduction with a good prognosis.
A case of hip dislocation is to be treated as an emergency. As it is an injury caused by a high-energy trauma, thorough systemic examination and ruling out associated injuries is a must.
References
- 1.Yeganeh A, Tavakoli N, Soleimani M, Taheri SN, Cheraghiloohesara S. Inferior hip dislocation in a 60-year-old man; A case report. Arch Acad Emerg Med 2022;10:e17. [Google Scholar | PubMed]
- 2.Jain S, Haughton BA, Grogan RJ. Inferior dislocation of the hip: A case report and literature review. J Orthop Surg (Hong Kong) 2015;23:123-6. [Google Scholar | PubMed]
- 3.Aggarwal S, Kumar V, Bhagwat KR, Shashikanth VS, Ravikumar HS. Inferior dislocation of the hip: A case series and literature review. Chin J Traumatol 2012;15:317-20. [Google Scholar | PubMed]
- 4.Tekin AC, Cabuk H, Büyükkurt CD, Dedeoglu SS, Imren Y, Gürbüz H. Inferior hip dislocation after falling from height: A case report. Int J Surg Case Rep 2016;22:62-5. [Google Scholar | PubMed]
- 5.Mauck HP, Anderson RL. Infracotyloid dislocation of the hip. J Bone Joint Surg 1935;17:1011-3. [Google Scholar | PubMed]
- 6.Kiel J, Genova R. Inferior hip dislocation in a 16 year old. Am J Emerg Med 2021;46:798.e1-3. [Google Scholar | PubMed]
- 7.Hani R, Kharmaz M, Berrada MS. Traumatic obturator dislocation of the hip joint: A case report and review of the literature. Pan Afr Med J 2015;21:55. [Google Scholar | PubMed]
- 8.Rico JI, Barquet A. Luxatio erecta of the hip. A case report and review of the literature. Arch Orthop Trauma Surg (1978) 1982;99:227-9. [Google Scholar | PubMed]
- 9.Dreinhöfer KE, Schwarzkopf SR, Haas NP, Tscherne H. Isolated traumatic dislocation of the hip. Long-term results in 50 patients. J Bone Joint Surg Br 1994;76:6-12. [Google Scholar | PubMed]
- 10.Yang RS, Tsuang YH, Hang YS, Liu TK. Traumatic dislocation of the hip. Clin Orthop Relat Res 1991;265:218-27. [Google Scholar | PubMed]