Even common-looking hand swellings can mask rare nerve sheath tumors. MRI and USG may not yield definitive results. High clinical suspicion and nerve-preserving surgery followed by histopathology are essential for accurate diagnosis and good recovery.
Dr. Rohit Karthik, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: rohotron@gmail.com
Introduction: Schwannomas of the hand are uncommon, and those arising from the thenar motor branch are extremely rare. Their indolent nature and overlap with ganglion cysts often delay accurate diagnosis.
Case Report: A 40-year-old woman presented with a gradually progressive, painless thenar swelling, initially presumed to be a ganglion. Ultrasonography and magnetic resonance imaging failed to yield definitive findings. The mass was enucleated carefully. Histopathological examination confirmed schwannoma. The patient made a complete functional recovery.
Conclusion: Schwannomas in the thenar region may mimic ganglia. Imaging may not always be diagnostic. When symptoms suggest neural involvement, surgical exploration and biopsy are warranted to avoid misdiagnosis and preserve function.
Keywords: Thenar mass, schwannoma, median nerve, ganglion mimic, ultrasonography, magnetic resonance imaging, nerve-sparing surgery.
Hand swellings are a frequent concern in orthopedic and hand surgery clinics. The majority are ganglion cysts, often arising from the tendon sheath or joint capsule, and usually present as soft, fluctuant, mobile masses without neurological symptoms [1]. However, not all such swellings are benign ganglia. Schwannomas, the most frequent type of benign peripheral nerve tumors, arise from Schwann cells of the nerve sheath and account for <5% of hand tumors [2]. These tumors are slow growing and typically solitary, displacing rather than invading nerve fascicles [3]. They rarely occur in the motor branch of the median nerve and often present with minimal or no neurological symptoms initially [4]. Magnetic resonance imaging (MRI) is the imaging modality of choice for such soft tissue masses, but it may fail to provide a definitive diagnosis, especially in small or atypical tumors [5]. Ultrasonography(USG), though accessible and cost-effective, also has diagnostic limitations [6]. This case report presents a diagnostically ambiguous swelling in the thenar eminence – clinically and radiologically suggestive of a ganglion – but histologically confirmed to be a schwannoma.
A 40-year-old right-handed female patient presented with a painless swelling over her dominant hand’s thenar region for 1 year. She initially noticed a small, mobile lump that neither increased in size nor caused discomfort. Being a homemaker and tailor, she ignored it until she began experiencing subtle thumb clumsiness and occasional tingling over the thumb and index finger during sewing tasks. Physical examination revealed a firm, non-transilluminant, well-circumscribed mass measuring 3 × 2 cm in the thenar region (Fig. 1). It was mobile perpendicular to skin tension lines but fixed in the longitudinal plane. Tinel’s sign was positive over the swelling, with radiating paresthesia to the thumb and index finger, suggesting neural involvement. Thumb abduction and opposition strength were reduced, while the rest of the neurological examination was intact.

Ultrasonography demonstrated a hypoechoic lesion with well-defined margins and posterior enhancement, mimicking a typical ganglion (Fig. 2). However, there was no clear origin from a joint capsule or tendon sheath. MRI showed a T1 isointense and T2 hyperintense, encapsulated lesion (Fig. 3). Despite its homogeneity, there was no definitive nerve continuity or “target sign” to confirm a peripheral nerve origin [5,7]. Both radiologists and clinicians concurred that the findings were not pathognomonic of schwannoma.
Considering the presence of neurological symptoms and inconclusive imaging, surgical excision was planned. A longitudinal incision was made along the thenar crease. Intraoperatively, a pinkish yellow, encapsulated lesion was found arising eccentrically from the motor branch of the median nerve (Fig. 4). The tumor displaced the surrounding fascicles but did not invade them. Microsurgical dissection was employed to preserve the fascicles while excising the mass in toto (Fig. 5).
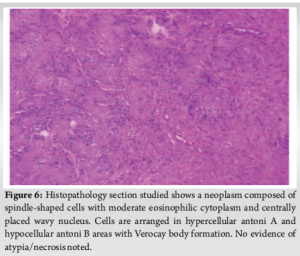
Histopathological analysis revealed biphasic Antoni A and B areas with Verocay bodies, confirming the diagnosis of schwannoma. Immunohistochemistry showed strong S-100 positivity (Fig. 6) [8].
At 3 months postoperatively, the patient had regained full strength in thumb opposition, abduction, and grip. There were no residual sensory deficits. Post-operative clinical testing of the median nerve showed complete restoration of motor and sensory function.
Schwannomas are slow-growing, benign tumors that most commonly involve major nerve trunks but rarely affect the hand, and even less frequently, the thenar region [2,4]. Their origin from the motor branch of the median nerve is especially uncommon, with fewer than 20 documented cases [9]. Clinically, these tumors may present without pain or neurological symptoms. However, even minor signs such as tingling or weakness in opposition – as in our case – should prompt suspicion. Tinel’s sign, though not specific, is a valuable clue in such soft tissue swellings [10]. Imaging is indispensable in evaluating hand tumors, but it has limitations. USG and MRI can suggest a diagnosis but not always confirm it. Schwannomas may appear homogenous and well-circumscribed, similar to ganglia, and nerve continuity may not always be demonstrable [5,6,11]. Our case underscores these limitations – imaging hinted at a benign lesion but failed to confirm its neural origin. A cautious clinician must interpret imaging in conjunction with history and examination to avoid diagnostic pitfalls. The hallmark of schwannoma is its eccentric position to the parent nerve and its ability to displace rather than invade fascicles. This property allows for complete surgical excision with nerve preservation if meticulous technique is followed [12]. Our patient recovered fully with no residual neurological deficit.
Even benign-looking swellings in the hand must be approached cautiously, especially when accompanied by neurological signs. Schwannomas can clinically and radiologically mimic ganglia. When imaging findings are inconclusive, surgical exploration and biopsy provide both diagnosis and cure. Early recognition and nerve-sparing excision yield excellent outcomes, as demonstrated in this case.
Not all hand swellings are ganglia. Subtle neurological signs should prompt suspicion of nerve sheath tumors. Even when MRI and USG fail to confirm the diagnosis, careful surgery and histopathology can ensure both diagnostic clarity and functional preservation.
References
- 1.Wang AA, Hutchinson DT. The volar wrist ganglion. J Hand Surg Am 2001;26:31-5. [Google Scholar | PubMed]
- 2.Knight DM, Birch R, Pringle J. Benign solitary schwannomas: A review of 234 cases. J Bone Joint Surg Br 2007;89:382-7. [Google Scholar | PubMed]
- 3.Phalen GS, Kendrick JI, Rodriguez JM. Neurilemmoma of the upper extremity. J Bone Joint Surg Am 1976;58:354-8. [Google Scholar | PubMed]
- 4.Adani R, Baccarani A, Guidi E, Tarallo L. Schwannomas of the upper limb: Diagnosis and treatment. Chir Main 2008;27:75-9. [Google Scholar | PubMed]
- 5.Beaman FD, Kransdorf MJ, Menke DM. Schwannoma: Radiologic-pathologic correlation. Radiographics 2004;24:1477-81. [Google Scholar | PubMed]
- 6.Pilavaki M, Chourmouzi D, Kiziridou A, Skordalaki A, Zarampoukas T, Drevelengas A. Imaging of peripheral nerve sheath tumors with pathologic correlation: Pictorial review. Eur J Radiol 2004;52:229-39. [Google Scholar | PubMed]
- 7.Oberle J, Kahamba J, Richter HP. Peripheral nerve schwannomas–An analysis of 16 patients. Acta Neurochir (Wien) 1997;139:949-53. [Google Scholar | PubMed]
- 8.Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors. 5th ed. Philadelphia : Mosby Elsevier; 2008. [Google Scholar | PubMed]
- 9.Rinker B, Effron C, Pu LL. Recurrent motor branch schwannoma: Case report and review. Microsurgery 2005;25:315-8. [Google Scholar | PubMed]
- 10.Kehoe NJ, Reid RP, Semple JC. Solitary benign peripheral-nerve tumours. Review of 32 years’ experience. J Bone Joint Surg Br 1995;77:497-500. [Google Scholar | PubMed]
- 11.Kim DH, Murovic JA, Tiel RL, Kline DG. Operative outcomes of 546 Louisiana state university health sciences center peripheral nerve tumors. Neurosurg Clin N Am 2004;15:177-92. [Google Scholar | PubMed]
- 12.Donner TR, Voorhies RM, Kline DG. Neural sheath tumors of major nerves. J Neurosurg 1994;81:362-73. [Google Scholar | PubMed]