Minimally invasive percutaneous pinning enables stable, plaster-free fixation of distal radius fractures with early functional recovery.
Dr. Anuraag Mohanty, Department of Orthopaedics, Medical College, Kalinga Institute of Medical Sciences, Bhubaneswar (kimsbhu), Odisha, India. E-mail: anuraag98@gmail.com
Aim & Background: Distal radius fractures are among the most frequently encountered bone injuries. Percutaneous pinning with a modified minimally invasive technique offers a less invasive alternative to conventional surgical interventions. This study aims to evaluate the early functional outcomes of this technique in managing distal radius fractures. Optimal management relies on precise anatomical alignment, minimal soft-tissue disruption, and prompt initiation of wrist rehabilitation. The objective is to assess the early functional outcomes of distal radius fractures treated with percutaneous pinning using a modified minimally invasive approach in adults.
Materials & Methods: A prospective study was carried out on 20 adult patients presenting with distal radius fractures. All patients underwent percutaneous pinning using a modified technique and were monitored over 6 months at Jajati Kesari Medical College and Hospital, Jajpur, Odisha. Functional recovery was evaluated postoperatively using Cooney’s adaptation of the Green and O’Brien scoring system.
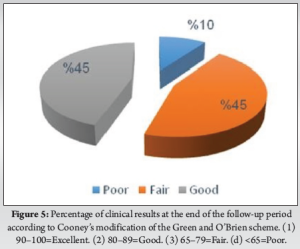
Results: Among the 20 participants, 9 (45%) demonstrated good functional outcomes, 9 (45%) had fair outcomes, and 2 (10%) had poor outcomes based on the Green and O’Brien scoring criteria.
Conclusion: The modified percutaneous fixation technique offers promising results in terms of fracture stabilization and early functional recovery. To confirm these findings, future research should be conducted with larger sample sizes.
Keywords: Distal radius fracture, percutaneous pinning, minimally invasive technique, fracture fixation, orthopedic outcomes.
Distal radius fractures are among the most common injuries encountered in the emergency department, particularly affecting the elderly population. The severity of these fractures is closely associated with the patient’s bone mineral density, which also significantly influences clinical outcomes [1]. These fractures typically occur within 3 cm of the radiocarpal joint and are usually closed, with the overlying skin remaining intact [2].
Despite appearing straightforward, distal radius fractures are often complex injuries. They may be accompanied by damage to adjacent ligamentous and cartilaginous structures, making prognosis variable and potentially leading to upper extremity dysfunction if not properly managed [3,4]. Therefore, an ideal treatment approach must ensure accurate anatomical restoration and stable fixation of the fracture fragments to minimize complications and preserve function [5].
Various treatment modalities are available. Non-operative management typically involves closed reduction followed by immobilization in a cast. Operative options include intrafocal pinning, non-spanning external fixation using a modified minimally invasive technique, spanning external fixation, arthroscopic-assisted procedures, and different forms of open reduction and internal fixation. The choice of surgical intervention often depends on the fracture configuration and the surgeon’s familiarity with the specific technique [6,7,8,9].
The modified minimally invasive technique is a contemporary approach that offers a less invasive alternative to traditional open surgery. It involves percutaneous insertion of pins to stabilize the fracture fragments during the healing process. In most percutaneous pinning techniques, Kirschner wires (K-wires) are inserted across the fracture site to maintain proper alignment and facilitate optimal bone healing [10].
This prospective study was carried out at Jajati Kesari Medical College and Hospital, Jajpur, Odisha, over a 12-month duration from April 2023 to March 2024. A total of 20 adult individuals diagnosed with distal radius fractures were recruited. The fractures included in the study encompassed both intra-articular and extra-articular, non-comminuted types. Classification was performed using the Frykman system, ranging from Type I to Type VIII [11]. The study used a consecutive sampling method over 12 months. Patients included were adults with extra-articular or minimally displaced intra-articular distal radius fractures who consented to operative management. In our government hospital setting, not all eligible patients opted for surgery, and hence, only those who were both eligible and willing were enrolled.
Inclusion criteria
- Patients with distal radius fractures
- Extra-articular displaced and intra-articular undisplaced fractures
- Adult patients (n = 20)
- A mean follow-up 6 months post-operative follow-up
- Functional outcomes were assessed using Green and O’Brien scoring system.
Exclusion criteria
- Neglected or old fractures
- Pathological fractures
- Pediatric age group
- Open (compound) fractures
- Associated carpal fractures
- Isolated distal radioulnar joint dislocations due to ligamentous injury
- Comminuted intra-articular fractures
- Previous fractures in the same region
- Concomitant neurological or vascular injury, or fractures elsewhere in the upper limb.
Surgical preparation
- Full clinical history including demographic details (name, age, sex)
- Written informed consent was obtained from all participants
- Clinical examination included inspection, palpation, assessment of range of motion, and neurovascular status
- All patients were deemed fit for regional or general anesthesia based on standard pre-operative investigations
- Patients were positioned supine, with the affected arm elevated and a tourniquet applied at 250 mmHg pressure.
Implants and instruments (Fig. 1)

- K-wires (generally 2.0 mm; 1.8 mm for smaller radii, 2.2 mm for larger radii)
- AO clamps (3.5 mm and 2.5 mm)
- 4.0 mm connecting rod.
Surgical technique

Following administration of anesthesia, the patient was positioned supine with the involved arm extended onto a side support (Fig. 2). The limb was aseptically prepared and draped. Traction was applied, and the fracture was manually reduced. The wrist was adjusted into slight volar flexion and ulnar deviation to facilitate alignment. Once an acceptable reduction was achieved, stabilization was performed using percutaneous K-wires.
The elbow was maintained at 90° flexion. Fracture alignment was confirmed under fluoroscopic guidance, capturing both anteroposterior and lateral views by rotating the C-arm around the wrist while maintaining a steady hand position.
K-wire Insertion: Three K-wires were used for osteosynthesis. In cases utilizing intramedullary techniques, K-wires were inserted manually with a chuck (T-handle), and the tips were bent appropriately.
- First intramedullary pin: This pin was inserted at the tip of the radial styloid, positioned between the first and second extensor compartments, slightly dorsal to the “volar line of Lewis.” The wire was directed into the radial diaphyseal canal, with its course maintained along the ulnar cortex. Gentle rotational movements were used for insertion, avoiding hammering to prevent damage, particularly in osteoporotic bone. The stabilizing effect of this method was initially documented by Benoist in 1995.
- Second intramedullary pin: The second wire was placed at the ulnar edge of the distal radius, between the third and fourth extensor compartments, close to Lister’s tubercle. This technique was consistent with the Kapandji method for intrafocal pinning. Special care was taken to prevent injury to the extensor pollicis longus tendon during placement.
- Optional additional pins: In select cases, additional bicortical K-wires were inserted based on fracture pattern and stability requirements.
Plaster immobilization was not used postoperatively, in line with the minimally invasive approach [12,13].
Post-operative care
- Post-operative radiographs were taken to assess reduction and fixation quality
- No casting was applied (a temporary splint was used for 3 days if necessary)
- Immediate active mobilization was encouraged
- Weekly pin site dressing (cleaning with Betadine and dry dressing) was done
- K-wires and Joshi’s clamp were removed in the outpatient department between 5 and 7 weeks post-surgery, once radiological signs of fracture consolidation were confirmed.
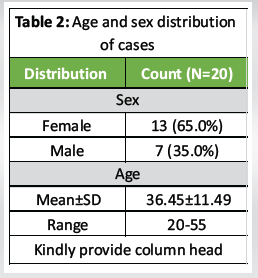
A total of 20 patients were included in the study, with a mean age of 36.45 ± 11.49 years (range: 20–55 years). The mean follow-up duration was 6 months. All patients underwent fracture stabilization using a percutaneous pinning method involving a modified minimally invasive approach.
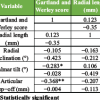
Post-operative radiographic assessment revealed an average radial height of 11.15 ± 1.31 mm, radial inclination of 22.40 ± 2.33°, and volar tilt of 10.95 ± 1.83°.
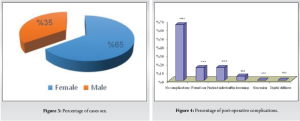
Physiotherapy was administered in 9 cases, accounting for 45% of the total. Fracture healing occurred, on average, within 40 days and was uneventful in most cases. However, complications were noted in a few patients: Three (15.0%) developed infections, another three (15.0%) had wound scarring, and one case (5.0%) showed signs of pin loosening. Post-operative clinical and radiological evaluations indicated no major joint restrictions or significant deterioration in radiographic parameters in the treated wrists [14] (Fig. 3).
Patients generally resumed normal wrist function approximately 1 week following surgery. Again, 45% (n = 9) of cases participated in physiotherapy. The age distribution of the patients remained consistent with a mean of 36.45 ± 11.49 years (range: 20–55) [15].
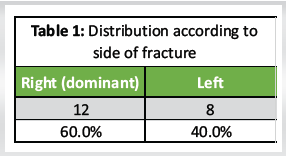
Out of the 20 cases, 12 involved the right wrist and 8 involved the left, but all patients were right-handed (Table 1). The cohort included 7 males (35.0%) and 13 females (65.0%) diagnosed with distal radius fractures (Table 2 and Fig. 4).
Seven patients experienced post-operative complications (Table 3):
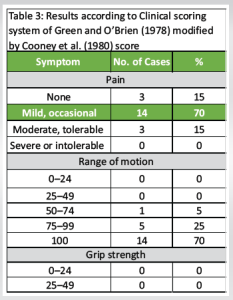
3 (15.0%) cases suffered from wound scar managed by local cream
3 (15.0%) cases suffered from wound infection managed by daily dressing with intravenous antibiotics (Fig. 5)
1 (5.0%) case suffered from pin loosening, managed by wires removal and replaced by a cast. The mean time of radiological union was 8 weeks (Fig. 6 and Table 4).
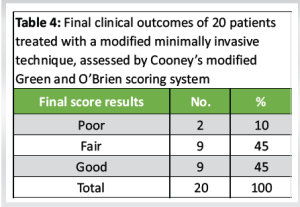

Our study demonstrated that modified minimally invasive percutaneous K-wire fixation resulted in predominantly good to fair functional outcomes at a mean follow-up of 6 months in adult patients with extra-articular or minimally displaced intra-articular distal radius fractures. This directly addressed the study objective of assessing early functional recovery without post-operative immobilization. The observed low complication rate, absence of plaster use, and early mobilization outcomes validate this method as a viable option for specific fracture patterns.
These findings are consistent with contemporary orthopedic literature. Tariq et al. (2023), in a meta-analysis of randomized controlled trials, found that while volar locking plates may offer slightly improved functional scores in the early post-operative phase, long-term outcomes (beyond 6 months) are statistically comparable to those achieved with percutaneous K-wire fixation [16]. Similarly, Mirarchi et al. (2021) emphasized that minimally invasive techniques in distal radius fractures can preserve soft-tissue integrity and yield equivalent mid-term function without the additional risks associated with open plating [17].
Our method structurally aligns with the principles of the minimally invasive reduction and osteosynthesis system (MIROS), which combines intramedullary and bicortical stabilization through a hybrid construct. Patel et al. (2024) demonstrated that MIROS fixation in 80 adult patients with Frykman I and II distal radius fractures led to early radiological union, immediate mobilization, and a low incidence of pin migration or soft-tissue complications, all achieved without post-operative plaster [18]. Dhanda et al. (2024), in a prospective comparative analysis, found that MIROS provided faster rehabilitation and fewer complications when compared with conventional wrist-spanning external fixators, further reinforcing the clinical utility of this configuration [19].
Importantly, the benefits of MIROS extend beyond adult distal radius fractures. In a pediatric setting, Gyllenborg et al. (2022) conducted a randomized controlled longitudinal study evaluating MIROS for displaced forearm fractures in children. The results demonstrated effective stabilization, improved cosmetic outcomes, reduced implant irritation, and favorable long-term functional results compared to standard methods [20]. This cross-demographic applicability supports the stability and versatility of the MIROS concept.
Despite these strengths, our study has limitations. It is a single-center, non-randomized analysis with a limited sample size and only a mean follow-up duration of 6 months. These factors restrict the ability to detect late-onset complications such as loss of reduction or post-traumatic arthritis. Moreover, the absence of a comparator arm prevents direct evaluation against other fixation modalities.
Future multicenter randomized trials with extended follow-up and cost-benefit analysis are warranted to validate the broader applicability and long-term outcomes of this technique, particularly in comparison with volar plating and conservative treatment.
Percutaneous fixation of distal radius fractures using three Kirschner wires introduced intramedullary, bicortically, or in combination provides effective stabilization and satisfactory reduction, particularly in extra-articular fracture types. The stability achieved is further enhanced by the use of an AO clamp and connecting rod, eliminating the need for post-operative plaster immobilization. Early mobilization is facilitated, and in our study, physiotherapy was required in 9 cases (45%). Overall, this modified minimally invasive technique demonstrates promising results in achieving stable fixation with minimal invasiveness and supports early functional recovery.
MIROS-based percutaneous fixation allows stable, plaster-free treatment of select distal radius fractures with early return of function. It is particularly useful in scenarios where implant costs or surgical invasiveness are limiting factors.
References
- 1.Mantovani M, Trevisan M, Cassini M. Percutaneous osteosynthesis with Kirschner wires and Joshi clamp for unstable extra-articular fractures of the distal radius. J Hand Surg 2009;46:26-39. [Google Scholar | PubMed]
- 2.Benoist LA, Freeland AE. Buttress pinning in the unstable distal radial fracture. A modification of the Kapandji technique. J Hand Surg Br 1995;20:82-96. [Google Scholar | PubMed]
- 3.Bucholz RW, Heckman JD, Court-Brown CM, Tornetta P. Rockwood and Green’s Fractures in Adults. 7th ed. Washington, DC: Williams and Wilkins; 2009. [Google Scholar | PubMed]
- 4.Canale ST, Beaty JH. Campbell’s Operative Orthopaedics. 11th ed. United States: Mosby; 2007. [Google Scholar | PubMed]
- 5.Cooney WP 3rd, Dobyns JH, Linscheid RL. Complications of Colles’ fractures. J Bone Joint Surg Am 1980;62:613-9. [Google Scholar | PubMed]
- 6.Frykman G. Fracture of the distal radius including sequelae--shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand 1967;Suppl 108:3. [Google Scholar | PubMed]
- 7.Gofton W, Liew A. Distal radius fractures: Nonoperative and percutaneous pinning treatment options. Orthop Clin North Am 2007;38:175-85. [Google Scholar | PubMed]
- 8.Green DP, O’Brien ET. Open reduction of carpal dislocations: Indications and operative techniques. J Hand Surg Am 1978;3:250-65. [Google Scholar | PubMed]
- 9.Grewal R, Perey B, Wilmink M, Stothers K. A randomized prospective study on the treatment of intra-articular distal radius fractures: Open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation, and external fixation. J Hand Surg Am 2005;30:764-72. [Google Scholar | PubMed]
- 10.Handoll HH, Vaghela MV, Madhok R. Percutaneous pinning for treating distal radial fractures in adults. Cochrane Database Syst Rev 2007;3:CD006080. [Google Scholar | PubMed]
- 11.Joshi N, Desai PC, Dhukia RK, Shetty A, Sharma KM, Singh M. Prospective study on outcome in management of distal radius fracture by closed reduction and percutaneous 5 K-wire fixation. Int J Orthop Sci. 2021;7(3):572–577. [Google Scholar | PubMed]
- 12.Ibrahim T, Ghaleb M, Saleh A. Modified percutaneous pinning technique for distal radius fractures: Outcomes in a tertiary center. Injury 2023;54:155-62. [Google Scholar | PubMed]
- 13.Tzioupis C, Pape HC. Minimally invasive reduction and osteosynthesis techniques (MIROS) for fractures: Current evidence and future trends. Eur J Trauma Emerg Surg 2019;45:979-87. [Google Scholar | PubMed]
- 14.Lim HC, Yoon YC, Lee IS. Reliability and responsiveness of wrist scoring systems in patients after distal radius fracture surgery. J Hand Surg Glob Online 2020;2:115-22. [Google Scholar | PubMed]
- 15.Yoo JH, Choi Y, Lee SU. Comparison of percutaneous pinning and volar plating in extra-articular distal radius fractures: A matched cohort analysis. J Orthop Surg Res 2022;17:58. [Google Scholar | PubMed]
- 16.Tariq MA, Ali U, Uddin QS, Altaf Z, Mohiuddin A. Comparison between volar locking plate and kirschner wire fixation for unstable distal radius fracture: A meta-analysis of randomized controlled trials. J Wrist Surg 2023;13:469-80. [Google Scholar | PubMed]
- 17.Mirarchi AJ, Nazir OF. Minimally invasive surgery: Is there a role in distal radius fracture management? Curr Rev Musculoskelet Med 2021;14:95-100. [Google Scholar | PubMed]
- 18.Patel V, Tilavat A, Patel T, Patel P, Patel V, Pandya B, et al. Miros fixation in distal end radius fractures. Int J Sci Res 2024;13:71-4. [Google Scholar | PubMed]
- 19.Dhanda M, Singh LL, Mazumder P, Jaiswal S. A comparative and prospective analysis of extraarticular distal radius fractures fixed with minimally invasive reduction osteosynthesis(MIROS) vs ligamentotaxis with wrist joint spanning external fixator(WJSEF) Int J Acad Med Pharm 2024;6:401-4. [Google Scholar | PubMed]
- 20.Gyllenborg L, Karbo T, Wong C. Testing a new method of osteosynthesis of forearm fractures in children; A prospective randomized controlled longitudinal study. J Child Orthop 2022;16:88-97. [Google Scholar | PubMed]