This case illustrates that a chronic tear of the rectus femoris that has failed extensive conservative treatment may benefit from surgical debridement with primary tendon-to-tendon repair, allowing quick return to sport at pre-injury level.
Dr. Andrew S Cuthbert, Department of Orthopaedic Surgery, Virginia Commonwealth University School of Medicine, PO Box 980153 Richmond, VA 23298, United States. E-mail: andrew.cuthbert@vcuhealth.org
Introduction: Chronic tears of the rectus femoris (RF) are common injuries in sports involving sprinting and jumping; however, there is limited data on management and surgical indications. This holds particularly true with severe and recurrent injuries. Conservative treatment with rest and physical therapy (PT) or surgical management with excision versus repair are current options. We present a case of a chronic tear of the RF that failed extensive conservative management and subsequently underwent pseudotumor excision and direct tendon-to-tendon repair with successful return to sport.
Case Report: This case report describes a chronic injury to the indirect head of the RF in a 21-year-old softball player. The insidious onset was characterized by pain, edema, intramuscular hematoma, and decreased range of motion. The patient failed extensive conservative treatment, including 12 months of medication, PT, and activity modification. Surgical intervention and rehabilitation enabled the athlete to return to collegiate sport at the Division I level.
Conclusion: Surgical debridement with primary tendon-to-tendon repair of a chronic tear of the RF that fails conservative treatment may allow a quick return to sport at pre-injury level.
Keywords: Athletic injury, chronic rectus femoris tear, rehabilitation, sports medicine.
The rectus femoris (RF) is one of four quadriceps muscles with the vastus medialis, vastus intermedius, and vastus lateralis. It is unique among these muscles as it crosses both the hip and knee joints. Its biarthrodial nature makes the RF prone to injury, particularly when stressed with an eccentric load while tightly contracted. In non-kicking athletes, RF tears commonly occur when sprinting during both deceleration and the swing phase of acceleration. The majority of these injuries heal without complication following non-operative management [1,2]. Following clinical diagnosis of RF injury, grading the location and degree is difficult. Magnetic resonance imaging (MRI) is the most reliable diagnostic tool; however, determining the degree of injury may be challenged by hemorrhage, tendon retraction, scar tissue, and local edema [3]. Chronic injuries may be misdiagnosed; they are often accompanied by a firm nodule or mass within the proximal third of the thigh [4]. These factors, combined with the lack of data regarding injury prevalence and ideal management, contribute to a high potential for misdiagnosis and mistreatment of RF tears [5]. This case presents a chronic, partial-thickness tear of the indirect head of the RF with pseudotumor formation and associated lateral femoral cutaneous nerve (LFCN) symptoms in a Division I athlete managed surgically with scar excision, tendon-to-tendon repair, and LFCN neurolysis, resulting in complete healing and return to pre-injury level of play.
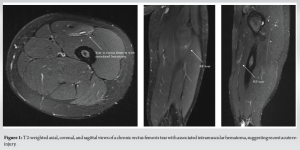
A healthy 21-year-old female collegiate softball player was participating in sprint conditioning in August of 2022 when she experienced quadriceps tightness and a tearing sensation in her left hip. She continued to play that fall season despite ongoing left thigh pain. Her injury was managed conservatively, guided by her athletic trainer and physical therapy (PT). She continued to have pain that worsened with running, lunging, and squatting, and was unable to play in the Spring 2023 season. After a summer of rest, she returned to school for fall conditioning but continued to have significant pain and sporadic ecchymosis over the left quadricep. She was unable to participate in sports. She presented to a sports medicine physician in September of 2023 and was diagnosed with hip pain secondary to a suspected labral tear. Her thigh soreness was attributed to iliotibial band syndrome and her quadriceps dysfunction to compensatory movements. She was again referred to PT. The patient progressed appropriately; an MRI arthrogram of the left hip was unremarkable. Weeks later, despite initial progress, the patient felt a tightening sensation in her left quadriceps. The pain and tearing sensation were akin to those she previously experienced, and she noticed a small mass in the proximal third of her thigh. She returned to her sports medicine physician. She had no ecchymosis or weakness with hip flexion but did have a palpable, small mass over her proximal quadriceps. This was confirmed on ultrasound; however, the extent and chronicity of the injury were not well characterized. She was diagnosed with a possibly chronic left quadriceps strain and instructed to continue PT. She sought a second opinion at our clinic. Physical examination showed a palpable mass over the left proximal thigh, significant pain with resisted hip flexion and knee extension, lateral thigh paresthesias, and a positive Tinel sign adjacent to the small mass. Her LFCN paresthesias were exacerbated by squatting. A non-contrast MRI of the left thigh (Fig. 1) revealed a partial thickness tear of the indirect head of the RF at the level of the proximal femoral diaphysis and an intramuscular hematoma, suggesting acute-on-chronic injury. The proximal origins of the RF tendon were intact. No other injury was noted.
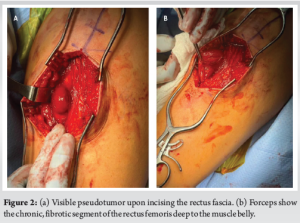
The patient had already failed over 1 year of conservative management and was entering her senior season. Surgical options were discussed; the patient elected to proceed with surgery with the goal of playing her final collegiate softball season. She was consented for left rectus tendon repair, scar excision, and LFCN neurolysis. In pre-operative holding, the pseudotumor was marked while the patient was performing a squat to accentuate the small mass. The incision was centered over this region and measured 10 cm in length. Dissection was performed over the anterior fascia. Branches of the LFCN were carefully dissected, and neurolysis was performed to mobilize the nerve branches away from the pseudotumor. Upon making the longitudinal anterior fascial incision, the pseudotumor was encountered on the deep surface of the quadriceps musculature (Fig. 2).
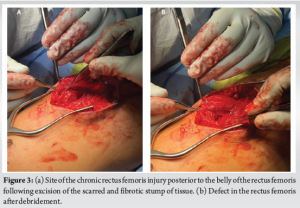
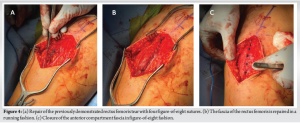
The fibrous mass was excised (Fig. 3) and deep tendon was repaired in side-to-side fashion with #2 Ethibond suture, allowing the prior mass to lay flat (Fig. 4). The wound was irrigated and #1 Vicryl was run along the anterior fascia (Fig. 4), taking care not to capture LFCN branches. Skin was closed in layered fashion. Dry dressings and knee brace were applied. Postoperatively, she was allowed to weight bear as tolerated in a total range of motion (TROM) brace locked in full extension.
The patient started PT 2 weeks post-operatively. The initial protocol allowed a range of motion from 0 to 30° and weight-bearing with the TROM locked in extension. Only isometrics or closed chain exercises were allowed, with no eccentric exercises. Range of motion was to progress 20° every 2 weeks. By 6 weeks, she participated in PT with no brace, and knee range of motion was 90°. At 8 weeks, she was liberalized from the brace and began jogging. Knee range of motion was 120°. Other activities included squats, reverse lunges, and box jumps. Her LFCN paresthesias with hip flexion were completely resolved. By 12 weeks, the patient was cleared to participate in softball training, including full sprints. She tolerated this progression well with normal expected soreness and was cleared for play 3 months post-operatively. She returned to the field, playing at an elevated level of performance statistically compared to her prior athletic seasons. She appeared in 40 games, starting seven and batting 0.429. She has no further problems in terms of weight training or recurrent neurologic symptoms.
Proximal RF tears may occur without a specific inciting event and present as a soft tissue mass in the anterior thigh [4]. Misinterpretation can lead to a prolonged healing process, missed athletic seasons, or inappropriate therapeutic treatments, resulting in suboptimal outcomes and recurrence [6]. Prompt and accurate diagnoses are essential given the rigorous training and demanding schedules athletes endure, as misdiagnosis can profoundly impact their careers [5]. Literature is limited regarding the management of chronic tears of the proximal RF at the musculotendinous junction. Avulsions of the RF are relatively rare injuries and constitute a minority of pelvic and hip injuries [7,8]. Of those injuries, few documented cases involve tears of the indirect and direct heads at the musculotendinous junction; even fewer involve chronic tears [7]. Due to the low incidence and general lack of data, there is no consensus on the management of chronic RF tears at the musculotendinous junction [8-10]. Severe and recurrent injuries present a varied prognosis, often leading to delayed return to sport and a heightened recurrence rate [11]. Wittstein et al. [8] described five collegiate athletes with chronic RF tears of the indirect head treated with delayed surgical excision. All patients had a significant reduction in pain post-operatively; however, four of the five athletes suffered residual symptoms, preventing a return to their pre-injury level of play. Those four athletes played sports requiring kicking; the athlete who returned to his previous level of play was a tight end. While these cases share similarities with the one presented, there are several crucial distinctions. In the described study, the athletes’ injuries were accurately diagnosed and treated accordingly. Surgical intervention entailed delayed excision versus repair and return to sport spanned a timeframe of 7–12 months. Conversely, our athlete’s situation involved misdiagnosis and a recurrent tear that presented as a pseudotumor. In addition, she experienced LFCN neuropraxia. Following primary repair and neurolysis, our athlete returned to sport at pre-injury level within a remarkably short rehabilitation period of 3 months, with no residual symptoms. The athlete’s symptom resolution and swift return to play are consistent with outcomes reported in a case series by Lempainen et al. [9]. Twelve athletes with chronic or recurrent RF tears were treated with debridement, primary tendon-to-tendon repair, and LFCN neurolysis. All athletes returned to pre-injury level of play within 2.5–4 months. While further data are required for a definitive conclusion, these findings indicate that optimal management of recurrent or chronic RF tears may involve debridement with primary tendinous repair. [12,13].
Chronic RF tears present unique challenges regarding return-to-play timelines. While uncomplicated, acute tears may be managed with a period of rest and rehabilitation (typically around 12 weeks), chronic tears may necessitate extended rehabilitation due to the cumulative effects of ongoing tissue damage and compensatory mechanisms. This case and the small body of existing literature suggest that operative intervention with primary tendon-to-tendon repair of chronic RF tears may allow return-to-sport at pre-injury level within 4 months. This phenomenon may be attributed to the surgical restoration of normal kinematic function of the RF, given its pivotal role in both the swing and foot strike phases.
Surgical management of a chronic tear of the RF with primary tendon-to-tendon repair can be successfully performed, leading to return to sport at pre-injury level. Surgical management should be considered in patients who fail conservative management or have recurrent injuries despite appropriate management.
References
- 1.Dalal S, Kotwal R, Chandratreya A. Operative versus conservative treatment of proximal rectus femoris avulsions: A systematic review with meta-analysis of clinical outcomes, complications and return to sports. J Clin Orthop Trauma 2021;15:83-92. [Google Scholar | PubMed]
- 2.Plastow R, Raj RD, Fontalis A, Haddad FS. Quadriceps injuries. Bone Joint J 2023;105-B:1244-51. [Google Scholar | PubMed]
- 3.Gyftopoulos S, Rosenberg ZS, Schweitzer ME, Bordalo-Rodrigues M. Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features. Am J Roentgenol 2008;190:W182-6. [Google Scholar | PubMed]
- 4.Temple HT, Kuklo TR, Sweet DE, Gibbons CL, Murphey MD. Rectus femoris muscle tear appearing as a pseudotumor. Am J Sports Med 1998;26:544-8. [Google Scholar | PubMed]
- 5.Mackala K, Michalik K, Makaruk H. Sports diagnostics-maximizing the results or preventing injuries. Int J Environ Res Public Health 2023;20:2470. [Google Scholar | PubMed]
- 6.Maffulli N, Del Buono A, Oliva F, Giai Via A, Frizziero A, Barazzuol M, et al. Muscle injuries: A brief guide to classification and management. Transl Med UniSa 2014;12:14-18. [Google Scholar | PubMed]
- 7.Ouellette H, Thomas BJ, Nelson E, Torriani M. MR imaging of rectus femoris origin injuries. Skeletal Radiol 2006;35:665-72. [Google Scholar | PubMed]
- 8.Wittstein J, Klein S, Garrett WE. Chronic tears of the reflected head of the rectus femoris: Results of operative treatment. Am J Sports Med 2011;39:1942-7. [Google Scholar | PubMed]
- 9.Lempainen L, Kosola J, Valle X, Puigdellivol J, Ranne J, Orava S, et al. Chronic and recurrent rectus femoris central tendon ruptures in athletes: Clinical picture, MRI findings, and results of surgical treatment. Orthop J Sports Med 2021;9:2. [Google Scholar | PubMed]
- 10.Park CK, Zlomislic V, Du J, Huang BK, Chang EY, Chang DG. Nonoperative management of a severe proximal rectus femoris musculotendinous injury in a recreational athlete: A case report. PM R 2018;10:1417-21. [Google Scholar | PubMed]
- 11.McAleer S, Macdonald B, Lee J, Zhu W, Giakoumis M, Maric T, et al. Time to return to full training and recurrence of rectus femoris injuries in elite track and field athletes 2010-2019; A 9-year study using the British athletics muscle injury classification. Scand J Med Sci Sports 2022;32:1109-18. [Google Scholar | PubMed]
- 12.Hotfiel T, Seil R, Bily W, Bloch W, Gokeler A, Krifter RM, et al. Nonoperative treatment of muscle injuries - recommendations from the GOTS expert meeting. J Exp Orthop 2018;5:24. [Google Scholar | PubMed]
- 13.Ema R, Sakaguchi M, Kawakami Y. Thigh and psoas major muscularity and its relation to running mechanics in sprinters. Med Sci Sports Exerc 2018;50:2085-91. [Google Scholar | PubMed]