Miss-a-nail technique is an alternative method of fixation of the neck of femur fracture without removing the nail, thus decreasing operative time and comorbidity to the patient.
Dr. Pramod Kumar, Department of Orthopaedics, Dr Baba Saheb Ambedkar Medical College and Hospital, New Delhi, India. E-mail: pramoddefineshere@gmail.com
Introduction: The neck of the femur fracture is more prevalent in the elderly, but can occur in young individuals due to high-energy trauma. Management of neck femur fracture with the femur interlocking nail in situ is a technically demanding case.
Case Report: A 24-year-old male with a femoral neck fracture in the presence of an in-situ femoral interlocking nail was successfully managed using the MISS-A-NAIL technique. The goal of the management was an anatomical reduction of the neck of the femur fracture without removing the in situ femur interlocking nail, getting a stable hold and fixation with the cannulated compression screw without getting in the way of the interlocking femur nail, and using a minimally invasive technique with only a 3–4 cm incision.
Conclusion: By providing a less invasive alternative to the traditional approach of removing interlocking nail and then fixing the neck of femur fracture, “Miss a nail technique” addresses the limitations of functional compromise associated with blood loss, neck of femur fracture displacement, iatrogenic fracture of the shaft femur, infections, and intra op complications related to nail removal.
Keywords: Neck of femur fracture, intramedullary nail, cannulated screw.
Neck of the femur fractures are most commonly seen in the elderly [1]. Still, it can also occur in young patients due to high-energy trauma, and also if comorbidities are present in young individuals [2-4]. The shaft of femur fractures is more common in young individuals due to high-energy trauma, and sedentary lifestyle workers, and can occur in the elderly with trivial trauma [5]. The isolated neck femur fractures are in young individuals managed with cannulated compression screws fixation, with the newer technique such as femoral neck system [6], and in the older age group, the hemiarthroplasty or total hip replacement can be availed, depending on the acetabulum anatomy. Combining ipsilateral femoral neck and shaft fractures is an uncommon type of fracture. The associated ipsilateral femoral neck fractures have been reported to occur in 10% of all femoral shaft fractures [7]. The classical treatment for femoral neck fractures in young individuals is generally open or closed reduction with cannulated or non-cannulated screw (CCS) fixation. Moreover, the treatment options for femoral neck fractures with ipsilateral shaft with a nail in situ can be (1) removal of the femoral interlocking nail and then fixation of the neck of the femur with cannulated compression screws and (2) Miss-a-nail technique with minimal incision described in this paper. There is no description of this technique, very limited literature, and only two case reports regarding the miss-a-nail technique; hence, this study was conducted to describe this technique and also its benefits.
This is a case of a 24-year-old male elsewhere had case femur shaft fracture with an intramedullary nail 1 year back. He again sustained an injury to the right hip and had a neck or femur fracture, and presented with that complaint for further management.
Clinical findings
The patient presented to us with complaints of pain and being unable to bear weight on his right lower limb. On examination, the right lower limb was found to be in flexion, abduction, and external rotation. There was a healed scar mark on the lateral aspect of the thigh. X-ray showed the neck of the femur fracture, which is marked with an arrow in the anteroposterior (AP) and lateral images, which is undisplaced as shown in (Fig. 1a-c), Garden classification type 2. As the patient is young, there is no sign of osteoporosis or sign of decreased bone density on X-ray.

Figure 1: Pre-operative image neck of femur fracture with the femur interlocking implant in situ in anteroposterior (AP) (a and b) and lateral images (c), arrow showing undisplaced neck of femur in both AP and lateral image.
Surgical technique
The goal of surgical treatment was to restore normal anatomic reduction of the neck of femur fracture without removing the femur interlocking nail and using the minimally invasive procedure with the help of 6.5 mm cannulated compression screws. Typically, a 2.0 mm threaded guide wire is inserted at angles of 100, 110, 120, or 130°, either anterior or posterior to the existing femoral nail. After drilling with a 4.5 mm cannulated drill bit, a 6.5 mm stainless steel CCS is placed along the guide wire’s path. During the guide wire insertion, it is often inevitable that the wire will contact the path of the nail or proximal locking screws due to limited space. Moreover, a worn-out guide wire may break at the thread runout when it makes contact with the nail or proximal screw path.
To resolve this issue, we replaced the threaded guide wire with a 2.5 mm Kirschner wire in our case, which allowed us to create a path away from the nail towards the femoral head without breaking upon contact with the nail or proximal locking screw. After reducing the femoral neck fracture, we observed space under the C-arm, with the anterior space visible in the lateral view and the inferior space in the AP view. This space allowed us to insert two K-wires, which were then checked under the C-arm (Fig. 2a-b). Shows two K-wires passed posterior to the nail and missing the nail, with the arrow marked. Afterward, the 2.5 mm Kirschner wire was removed, and the 2.0 mm threaded guide wire was inserted into the path created by the Kirschner wire. Two partially threaded 6.5 mm cannulated compression screws were then inserted, achieving fracture compression and reduction without disturbing the in situ nail, as shown in the post op image in (Fig. 3a-c) it shows post-op image neck of femur fracture in AP (3a, 3b) and lateral images (3c), with well-reduced neck of femur with CCS screw with femur interlocking nail in situ. This approach helped reduce operative time, blood loss, and fracture displacement while minimizing intraoperative and post-operative complications.
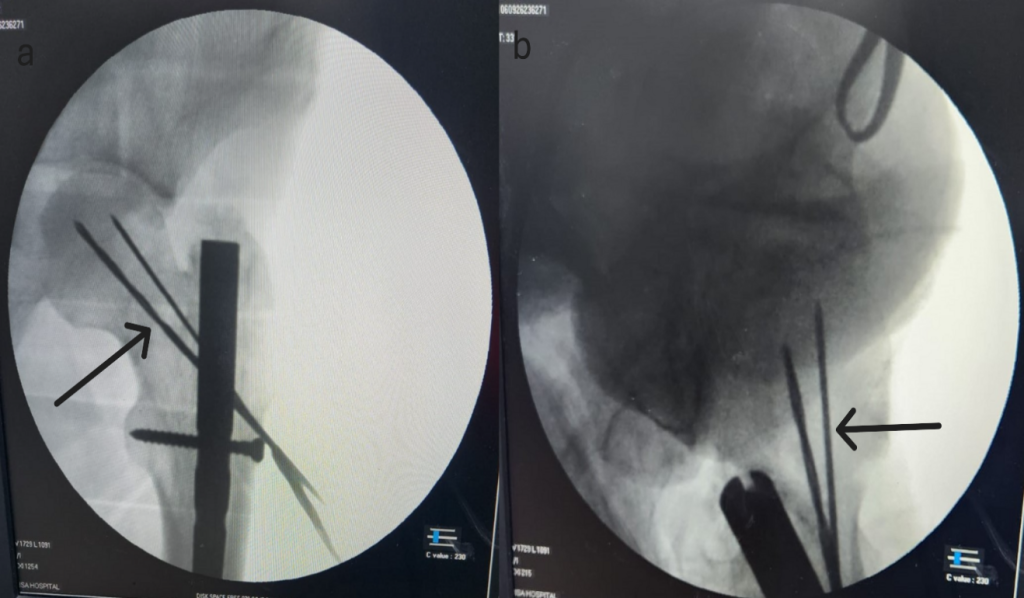
Figure 2: Intra-op image neck of femur fracture with the femur interlocking implant in situ in anteroposterior (a) and lateral images (b), arrow showing K-wire passed without disturbing the nail.
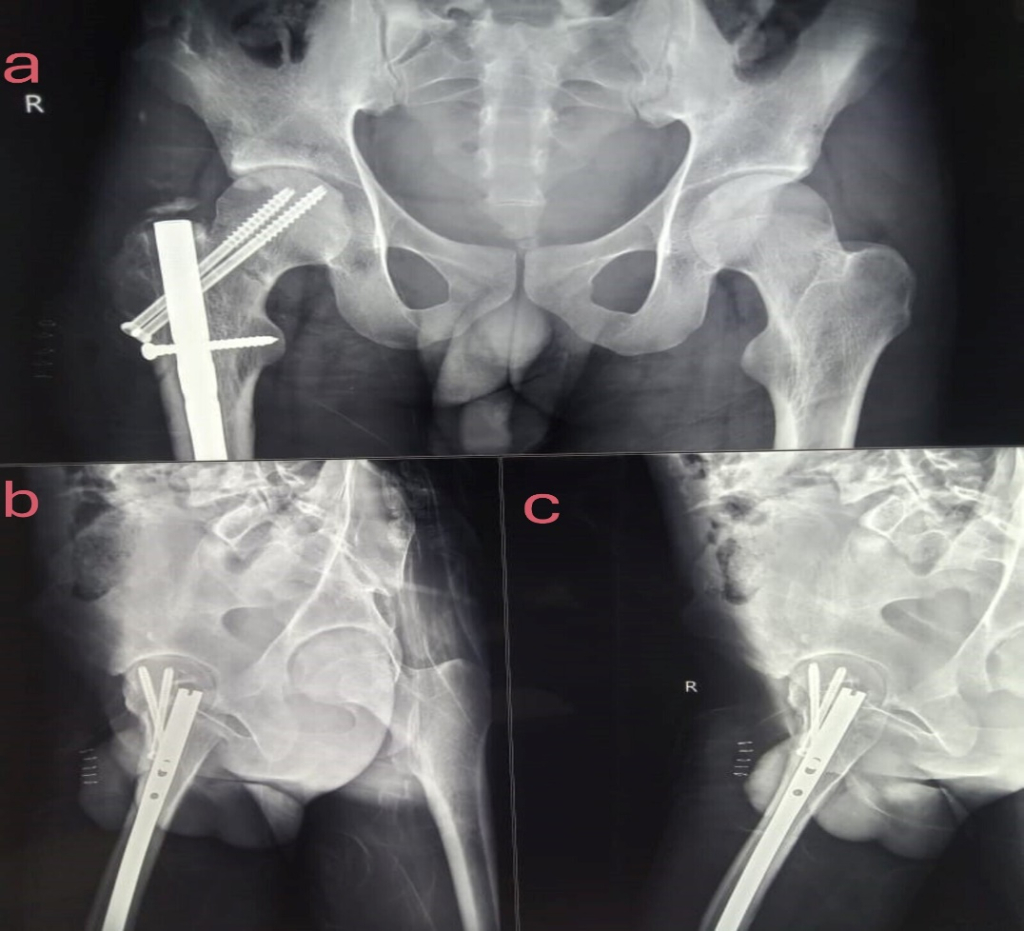
Figure 3: Post-op image neck of femur fracture in anteroposterior (a and b) and lateral images (c), with well-reduced neck of femur with cannulated screw screw with femur interlocking nail in situ.
Post-operative
The patient was allowed to sit, and knee bending was advised on the 1st post-operative day, and the Visual Analog Scale score was 3 (mild pain). On the 2nd post-operative day, in-bed turning, active quadriceps, hamstrings, and ankle pump were initiated, and on the 3rd postoperative day, he was allowed to mobilize without bearing weight. Using a walker, non-weight bearing was started. After being admitted to the hospital for 3 days, the patient was released. During his hospital stay, no other issues were observed. He was told to attend physiotherapy sessions after being released from the hospital, and several routine follow-up appointments were planned. However, after 1 month, the patient shifted to another country, and there was a loss of follow-up. After 3 months, we somehow made telephonic contact and asked about the condition. The patient was able to bear full weight and had only mild discomfort while walking. The Harris hip score was assessed through a call, which was 85, which showed a good result, and gait was normal, as was told by the patient. This was a limitation of the study as the patient was unable to follow up, and then he changed his number, and we could not get in contact. A computed tomography (CT) scan was not used to assess the screw placement as we want to make it cost-effective, which can even be used in rural areas, and screw placement was clearly visible in the X-ray, but CT can be used.
The management of femur neck fractures has evolved over the years, reflecting a change in techniques and a variety of techniques followed by various authors. It has witnessed a notable evolution, marked by a transition from traditional open-surgical techniques to more minimally invasive and innovative approaches. This progression has been driven by a deeper understanding of the complexities of these injuries and a continuous quest for improved functional outcomes and patient experiences.
The only previous management for femur neck fracture with an interlocking nail for femur shaft fracture in situ was the removal of the interlocking nail and then CCS fixation for femur neck fractures described by many authors.
We described a minimally invasive technique without removing the nail. There is not much learning curve, just proper preo-perative planning, X-ray, CT scan to know which direction to aim for CCS placement, and all done under C-arm.
Kow et al. [8] described a somewhat similar technique but did not give the description and details of the procedure, and a similar case report was published by Sanjay and Arun [9] but was of a single case and did not give much description of miss-a-nail technique.
Oh et al. [10] described a reverse miss-a-nail technique in which they provisionally fixed the neck femur with K-wires and inserted a nail, and then fixed the neck of the femur fracture, which is opposite of what we have described but follows the same principles of avoiding the path and fixing the fractures.
Hence, by describing this technique, we planned to raise awareness about this technique, and it can be used with minimal invasive and without much compromise to patients, and the removal of the nail, cost-effective, limited c-arm shots are required, as we are not removing the nail, and one can perform this procedure as day care.
The main goal of this treatment was an anatomical reduction of neck of femur fracture and cannulated compression screw fixation with the nail in situ with a minimally invasive procedure. “Miss a nail” technique is not only a good option but can also prevent prolonged hospital stay, early rehabilitation, and early return to work without causing a lot of discomfort to patients. Hence, we want to raise awareness regarding this technique, which can prevent intraoperative blood loss or any complications related to removing the femur nail.
Limitations
As this is a technical description, no comparisons were made, and it was described in only one patient, as this is a rare case, and we did not find another similar case. There was also a loss of follow-up of the patient as the patient shifted outside the country, so any details given were through a call, which was later lost as well.
Being a less invasive alternative to the traditional approach of removing the interlocking nail and then fixing the neck of the femur fracture, “Miss a nail technique” addresses the limitations of functional compromise associated with blood loss and short operative time.
References
- 1. Moon A, Gray A, Deehan D. Neck of femur fractures in patient’s aged more than 85 years-are they a unique subset? Geriatr Orthop Surg Rehabil 2011;2:123-7. [Google Scholar]
- 2. Thoors O, Mellner C, Hedström M. Good clinical outcome for the majority of younger patients with hip fractures: A Swedish nationwide study on 905 patients younger than 50 years of age. Acta Orthop 2021;92:292-6. [Google Scholar]
- 3. Singaravadivelu V, Kartheesan G, Vignesh S. Unstable fracture neck of femur in young adults: Management with cannulated cancellous screws augmented with medial buttress plate. J Orth Joint Surg 2019;1:1-4. [Google Scholar]
- 4. Pauyo T, Drager J, Albers A, Harvey EJ. Management of femoral neck fractures in the young patient: A critical analysis review. World J Orthop 2014;5:204-17. [Google Scholar]
- 5. Protzman RR, Burkhalter WE. Femoral-neck fractures in young adults. J Bone Joint Surg Am 1976;58:689-95. [Google Scholar]
- 6. Davidson A, Blum S, Harats E, Kachko E, Essa A, Efraty R, et al. Neck of femur fractures treated with the femoral neck system: Outcomes of one hundred and two patients and literature review. Int Orthop 2022;46:2105-15. [Google Scholar]
- 7. Wolinsky PR, Johnson KD. Ipsilateral femoral neck and shaft fractures. Clin Orthop Relat Res 1995;318:81-90. [Google Scholar]
- 8. Kow RY, Abdul-Aziz A, Low CL. Miss-a-nail technique for neck of femur screw fixation: It is easier said than done. Malays Orthop J 2020;14:96-7. [Google Scholar]
- 9. Sanjay N, Arun HS. Miss-a-nail technique for neck of femur fracture – a case report. J Clin Biomed Sci 2020;???:???. [Google Scholar]
- 10. Oh CW, Kim JW, Oh JK, Apivatthakakul T, Park KH, Hong W. “Reverse miss-a-nail technique” of reconstruction nailing for successful fixation of the ipsilateral femoral neck and shaft fracture. Arch Orthop Trauma Surg 2021;141:959-69. [Google Scholar]