In patients with recurrent patellar instability and normal bony anatomy, chronic medial patellofemoral ligament (MPFL) laxity may be the primary pathology. MRI plays a crucial role in identifying subtle signs of MPFL insufficiency–such as thinning, waviness, or elongation-guiding clinicians toward targeted soft-tissue interventions such as isolated MPFL reconstruction
Dr. Namdev Seth, Department of Radiodiagnosis, All India Institute of Medical Sciences, Gorakhpur, Uttar Pradesh, India. E-mail: namdevseth@gmail.com
Introduction: Recurrent patellar instability is generally attributed to bony anomalies such as trochlear dysplasia, patella alta, or increased tibial tuberosity–trochlear groove distance. However, some patients present with recurrent dislocations despite normal osseous anatomy.
Case Report: This case series presents three patients with recurrent patellar instability, where magnetic resonance imaging (MRI) findings revealed chronic medial patellofemoral ligament (MPFL) laxity as the primary abnormality. All cases showed thinning, elongation, or wavy contour of the MPFL without tears. Trochlear morphology, patellar height, and tibial tuberosity–trochlear groove distance were within normal limits. Secondary changes such as early chondromalacia and subchondral marrow edema were observed.
Conclusion: These cases underscore the importance of evaluating soft-tissue stabilizers, particularly the MPFL, when other anatomical parameters are unremarkable. MRI serves as a crucial tool for detecting MPFL laxity and guiding appropriate management, such as isolated MPFL reconstruction.
Keywords: Medial patellofemoral ligament laxity, recurrent patellar instability, trochlear dysplasia, magnetic resonance imaging knee, patella dislocation.
Patellar instability is a multifactorial condition, often attributed to structural abnormalities such as trochlear dysplasia, patella alta, and lateralized tibial tubercle positioning. However, some patients present with recurrent dislocations in the absence of these anatomical deformities. One frequently overlooked contributor in such cases is chronic laxity of the medial patellofemoral ligament (MPFL), a crucial soft tissue stabilizer of the patella. The MPFL accounts for up to 60% of the restraint against lateral patellar displacement, especially within the first 30° of knee flexion [1,2].
MRI has become the modality of choice for evaluating both osseous and soft-tissue structures of the knee [3]. This case series describes three patients with recurrent patellar instability in whom MRI revealed chronic MPFL laxity despite otherwise normal trochlear and patellar alignment.
Case 1
A 24-year-old male presented with recurrent episodes of the right patellar dislocation. There was no history of trauma, prior knee surgery, or congenital abnormalities. On physical examination, a positive patellar apprehension sign was noted. MRI of the right knee revealed mild lateral subluxation of the patella. The MPFL appeared attenuated and wavy but remained intact, without evidence of edema or tear. The tibial tuberosity-trochlear groove (TT-TG) distance was within normal limits, and no features of trochlear dysplasia or patella alta were identified. Subchondral marrow edema was noted in the medial femoral condyle. In addition, a small cartilage defect with associated marrow edema was seen in the medial patellar facet, consistent with early chondromalacia (Fig 1). These findings suggest that repetitive microtrauma due to MPFL laxity is contributing to the patient’s recurrent instability and early cartilage degeneration.
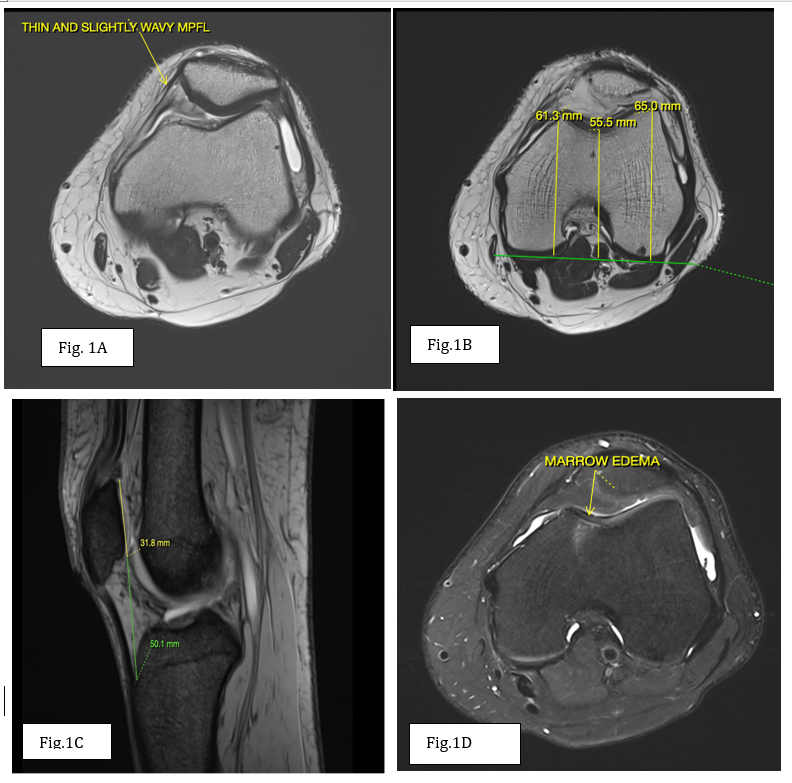
Figure 1 : (a) Axial T2 weighted image showing thinned and lax medial patello-femoral ligament. (b) Axial T2 weighted image showing normal trochlear depth i.e., >3 mm. (c) Sagittal T2 gradient echo sequence showing normal modified Insall-Salvati ratio<2 (d) Axial proton density fat suppressed image showing small cartilage defect with associated edema in medial patellar facet consistent with early chondromalacia-likely secondary to repetitive microtrauma.
Case 2
An 18-year-old female with a known history of congenital talipes equinovarus since birth presented with recurrent dislocations of the left patella, which had been occurring since childhood. MRI of the left knee showed a lateral trochlear inclination angle and trochlear groove depth within normal limits. The trochlear facet asymmetry ratio was >0.4, and the sulcus angle was borderline increased at <145°. There was no evidence of supratrochlear spur or prominence. The modified Insall–Salvati index was below 2, ruling out patella alta. The TT-TG distance measured approximately 14.5 mm, which is within the normal range. The MPFL appeared thin and wavy but was intact. Lateral patellar subluxation was present (Fig 2). These findings point toward a diagnosis of patellar instability due to soft tissue (MPFL) laxity in the absence of osseous dysplasia, likely influenced by the patient’s background of congenital limb deformity.
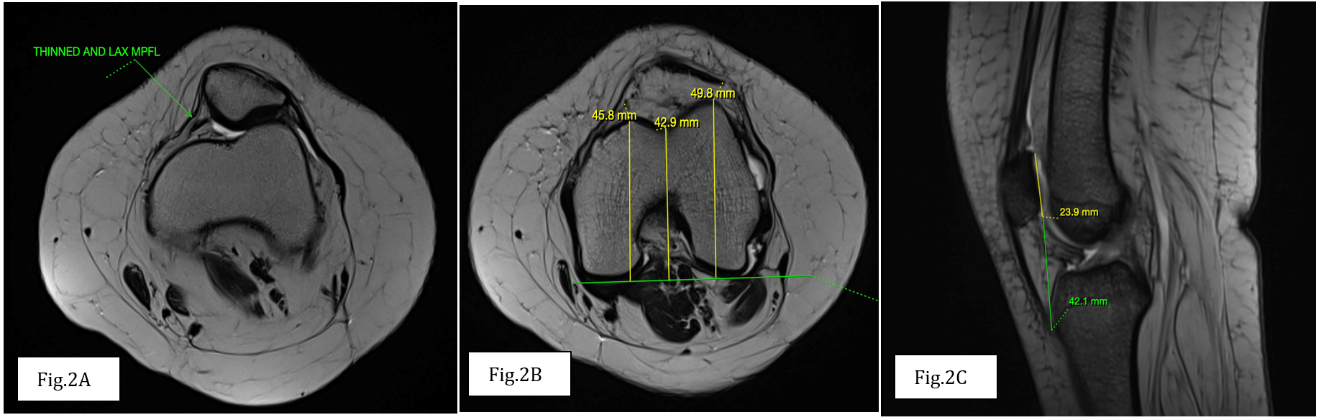
Figure 2: (a) Axial T2 weighted image showing thinned and lax medial patello-femoral ligament. (b) Axial T2 weighted image showing normal trochlear depth i.e., >3 mm. (c) Sagittal T2 gradient echo sequence showing normal modified Insall-Salvati ratio <2.
Case 3
A 28-year-old male presented with anterior knee pain and a history of recurrent right patellar dislocation. There was no previous history of surgery or trauma. MRI of the right knee demonstrated a lateral trochlear inclination angle of 28° and trochlear groove depth >3 mm, both within normal limits. The trochlear facet asymmetry ratio exceeded 0.4, and the sulcus angle was approximately 150°, indicating a borderline increase. No supratrochlear spur or prominence was seen. The TT-TG distance measured 15.5 mm, and the modified Insall–Salvati index was <2, indicating no patella alta. The MPFL appeared intact but showed a slightly wavy contour, without signs of edema or discontinuity. Mild lateral patellar subluxation was also observed (Fig 3). These findings suggest chronic functional laxity of the MPFL as the primary cause of recurrent patellar instability in the absence of structural anatomical abnormalities.
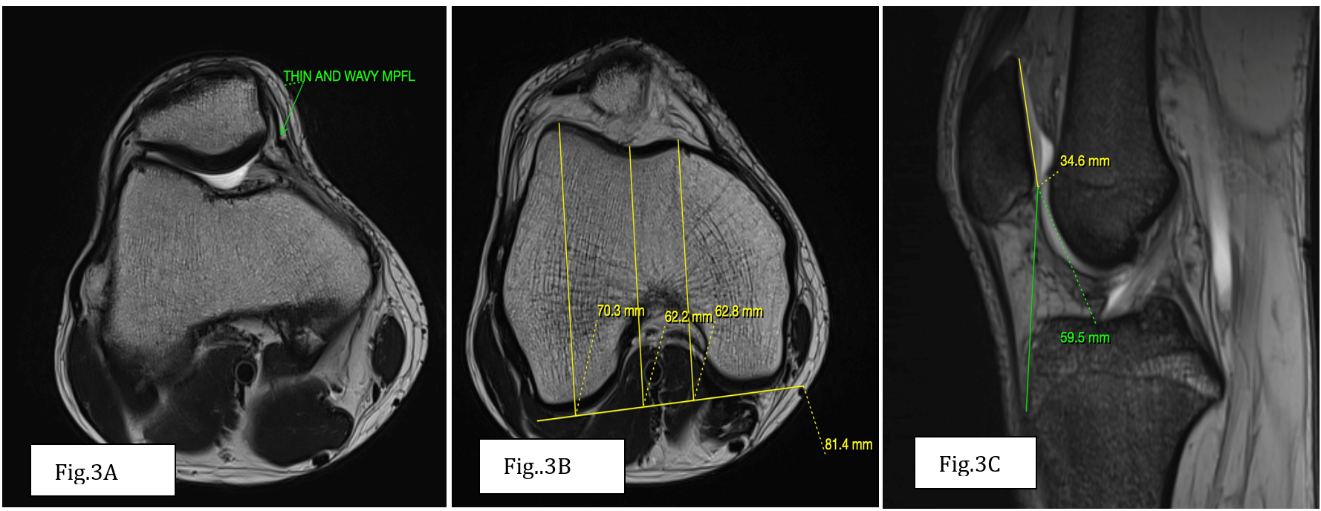
Figure 3: (a) Axial T2 weighted image showing thinned and wavy medial patello-femoral ligament. (b) Axial T2 weighted image showing normal trochlear depth i.e., >3 mm. (c) Sagittal T2 gradient echo sequence showing normal modified Insall-Salvati ratio <2.
This case series highlights patients with recurrent patellar instability attributable to MPFL laxity in the absence of classical anatomical abnormalities [4]. All patients demonstrated normal trochlear morphology, normal patellar height, and normal TT-TG distances (Table 1). The MPFL in each case was intact but appeared thinned, elongated, or wavy – signs of chronic laxity. MRI was instrumental in identifying these subtle soft-tissue alterations [5]. MPFL laxity should be considered when other causes are excluded. While trochlear dysplasia and bony malalignment remain dominant contributors to instability, this case series illustrates the importance of soft-tissue factors in surgical planning and patient management [6]. The MPFL functions as a passive stabilizer of the patella, particularly during early flexion. Its importance has been increasingly acknowledged in cases where classic risk factors such as trochlear dysplasia, patella alta, or increased TT-TG distance are absent [7]. In such scenarios, chronic MPFL insufficiency or laxity might result from repetitive stress, inherent ligamentous laxity, or subtle trauma. MRI evaluation can reveal the integrity and morphology of the MPFL, providing key diagnostic clues when gross anatomical structures appear unremarkable [8].

Table 1: Summary of clinical and MRI findings in three cases of recurrent patellar dislocation Without trochlear dysplasia
Identifying MPFL laxity is essential not only for diagnostic clarity but also for guiding appropriate surgical interventions. Procedures like isolated MPFL reconstruction have shown favorable outcomes in well-selected cases [9]. Failure to address this subtle soft-tissue pathology might lead to persistent instability even after bony realignment surgeries. Hence, radiologists and clinicians must be aware of the visual markers of MPFL laxity, such as thinning, elongation, or waviness on MRI [10].
This case series underscores that MPFL laxity, even in the absence of bony deformities, can be a significant and independent cause of recurrent patellar instability. MRI is an indispensable tool for identifying this subtle soft-tissue pathology. Recognition of MPFL morphological changes–such as thinning, waviness, and elongation–can guide clinicians toward more targeted, soft-tissue–focused interventions like isolated MPFL reconstruction. Greater radiologic awareness of this entity can improve diagnostic accuracy and treatment outcomes.
Isolated MPFL laxity can cause patellar instability even in the absence of classical bony abnormalities. MRI can reveal subtle ligamentous insufficiency and should be considered essential in evaluating such patients.
References
- 1. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19-26. [Google Scholar] [PubMed]
- 2. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee 2003;10:215-20. [Google Scholar] [PubMed]
- 3. Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: Injury patterns and assessment of risk factors. Radiographics 2010;30:961-81. [Google Scholar] [PubMed]
- 4. Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 2005;13:510-15. [Google Scholar] [PubMed]
- 5. Kramer J, White LM, Recht MP. MR imaging of the extensor mechanism. Semin Musculoskelet Radiol. 2009 Dec;13(4):384-401. doi: 10.1055/s-0029-1242191. Epub 2009 Nov 4. PMID: 19890805. [Google Scholar] [PubMed] [CrossRef]
- 6. Escala JS, Mellado JM, Olona M, Giné J, Saurí A, Neyret P. Objective patellar instability: MR-based quantitative assessment of potentially associated anatomical features. Knee Surg Sports Traumatol Arthrosc 2006;14(3):264–72. [Google Scholar] [PubMed]
- 7. Tanaka MJ, Chahla J, Farr J 2nd, LaPrade RF, Arendt EA, Sanchis-Alfonso V, et al. Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2537-2550. doi:10.1007/s00167-018-5266-y [Google Scholar] [PubMed] [CrossRef]
- 8. de Oliveira V, de Souza V, Cury R, Camargo OP, Avanzi O, Severino N, Fucs P. Medial patellofemoral ligament anatomy: is it a predisposing factor for lateral patellar dislocation? Int Orthop. 2014 Aug;38(8):1633-9. doi: 10.1007/s00264-014-2357-3. Epub 2014 May 11. PMID: 24817023. [Google Scholar] [PubMed] [CrossRef]
- 9. Balcarek P, Walde TA, Frosch S, Schüttrumpf JP, Wachowski MM, Stürmer KM, et al. Patellar dislocations in children, adolescents and adults: a comparative MRI study of medial patellofemoral ligament injury patterns and trochlear groove anatomy. Eur J Radiol. 2011 Sep;79(3):415-20. doi: 10.1016/j.ejrad.2010.06.042. Epub 2010 Jul 16. PMID: 20638212. [Google Scholar] [PubMed] [CrossRef]
- 10. Straume-Næsheim TM, Randsborg PH, Mikaelsen JR, Årøen A. Medial patellofemoral ligament reconstruction is superior to active rehabilitation in protecting against further patella dislocations. Knee Surg Sports Traumatol Arthrosc. 2022 Oct;30(10):3428-37. doi: 10.1007/s00167-022-06934-3. Epub 2022 Mar 28. PMID: 35347375; PMCID: PMC9464184. [Google Scholar] [PubMed] [CrossRef]










