The IlluminOss System implant offers a promising treatment solution for stabilization of pathologic fractures.
Miss. Summer Drees, The University of Toledo College of Medicine and Life Sciences, Toledo, Ohio, USA. E-mail: summer.drees@rockets.utoledo.edu
Introduction: This case report describes the management of a patient with renal cell carcinoma (RCC) who presented with an unstable distal humeral shaft fracture. Operative treatment is often palliative in such cases, as the median prognosis for RCC with metastatic bone disease is approximately 12 months.
Case Report: In this instance, internal fixation of the humeral fracture was achieved using the IlluminOss System (IS) implant, which provides minimally invasive and patient-specific bone stabilization.
Conclusion: At 1-year and 6 months follow-up, the patient reported good strength in the left arm and elbow, minimal pain, and an overall favorable recovery, demonstrating the potential utility of the IS implant for managing pathologic humeral fractures.
Keywords: Pathologic fracture, illuminOss implant, renal cell metastasis.
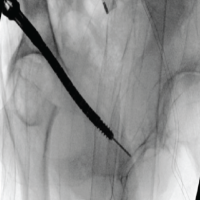
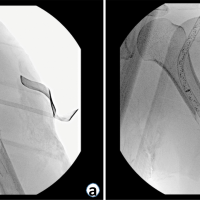
Renal cell carcinoma (RCC) accounts for more than 90% of renal cancers [1]. It arises from the tubular epithelial cells of the kidney and frequently metastasizes [2]. Common symptoms of RCC include a triad of hematuria, flank pain, and palpable abdominal mass; however, this triad is present in only 4–17% of cases [2]. Many patients are asymptomatic, and 20–30% of patients present with metastasis at the time of diagnosis [2]. The most common site of metastasis is the lung, followed by bone, which is involved in 20–35% of RCC cases [3]. Among the skeletal sites, the femur is the most common site of metastasis, followed by the humerus [1]. Patients with RCC and metastatic bone disease have a median survival of 12 months after diagnosis [4]. The treatment of pathologic fracture caused by metastatic bone disease is dictated by the patient’s overall prognosis and post-operative complications [5]. Management of pathologic fractures due to bone metastasis differs considerably from that of traumatic fractures. Operative intervention is often palliative and should be durable enough to outlast the patient’s expected survival [6]. For the operative treatment of humeral metastasis, modular prostheses, intra-medullary nails (IMN), or plates with cement are typically used [1,7]. This case highlights the surgical intervention for treating a pathologic fracture with an IlluminOss system (IS) implant. The IS is a patient-specific, intramedullary implant for bone stabilization that involves a balloon catheter being inserted into the intramedullary canal, being infused with a monomer, and finally being cured with light [8]. The ideal treatment of this distal-third left humerus fracture would have been an IMN to protect from possible future fractures [9,10]. Recent studies have suggested that there is minimal difference in the outcomes of IMN versus plate fixation (PF) of a pathological humeral shaft fracture. Both IMN and PF have risks and benefits that must be weighed when considering individual patient outcomes. IMN increases the risk of rotator cuff damage and limited shoulder mobility, whereas PF increases the risk of infection and non-union with a shorter implant length compared to IMN [11]. Here, we present a case detailing the use of the IS and PF to treat a pathologic distal-third left humerus fracture secondary to RCC metastasis. With the individual patient outcomes in mind, we elected to use a long PF method for several reasons. A primary concern of the patient was to maintain quality of life without loss of shoulder mobility, and an IMN would increase the risk of rotator cuff damage. In addition, the structural integrity of the proximal and distal humerus was another concern that could cause hardware failure (Fig. 1a). These factors supported the decision for PF, and the large, solitary lytic lesion with significant bone loss at the midshaft humerus supported the decision to use the IS and fill the lytic area. In addition, the IS allowed for drilling through the implant and immediate weight bearing. In the setting of compromised bone, such as this lytic lesion, it could permit less morbidity and better function than an isolated IMN or PF in isolation.
The patient is a 74-year-old female presenting with multiple significant comorbidities, including hypertension, hypercholesterolemia, chronic heart failure with preserved ejection fraction, type 2 diabetes mellitus, stage IIIb chronic kidney disease, non-alcoholic steatohepatitis cirrhosis, chronic obstructive pulmonary disease, obstructive sleep apnea, and obesity with a body mass index >40. She has a 24-year history of smoking, equivalent to a 33 pack-year history. In early 2024, the patient began experiencing worsening left humeral pain, which initially began as minor pain 2 years prior but progressively intensified. The assessment of pain was confounded by symptoms of cervical radiculopathy. Just over a year after the onset of symptoms, she presented to the emergency department (ED) with severe left arm and neck pain, worsened with movement of the left arm, causing pain to radiate up her neck. A computed tomography revealed an intramedullary mass with cortical erosion of the left humerus, raising suspicion for a neoplastic process. Magnetic resonance imaging confirmed a fracture of the left humerus. One week later, the patient sought further evaluation at another institution. Repeat imaging also revealed a 4 cm left renal mass. Two weeks later, additional imaging showed a 3 mm left lower lobe lung nodule. A biopsy confirmed the diagnosis of stage IV clear cell RCC with metastasis to the left humerus. Surgical intervention was decided for the patient, and she was placed into a Sarmiento brace until she could be cleared for surgery. One month after presenting to the ED, the patient underwent surgery for a displaced, unstable, pathologic distal humeral shaft fracture on the left side, shown in Fig. 1. The procedure involved the implantation of a synthes 3.5 mm extra-articular posterior distal humerus locking plate, with associated 3.5 mm cortical and locking screws, and an IS 15 × 220 mm photodynamic bone stabilization system. The plate was clamped in place during the reduction and confirmed with fluoroscopy. A guidewire was inserted to assess whether there was adequate space for the IS device. Upon confirmation, the IS balloon catheter was inserted, infused with a light-curable monomer, and then polymerized to achieve intramedullary stabilization [8]. 3.5 mm cortical screws were placed proximally and distally to secure the plate to bone for stabilization, and 3.5 mm locking screws were placed to complete fixation.
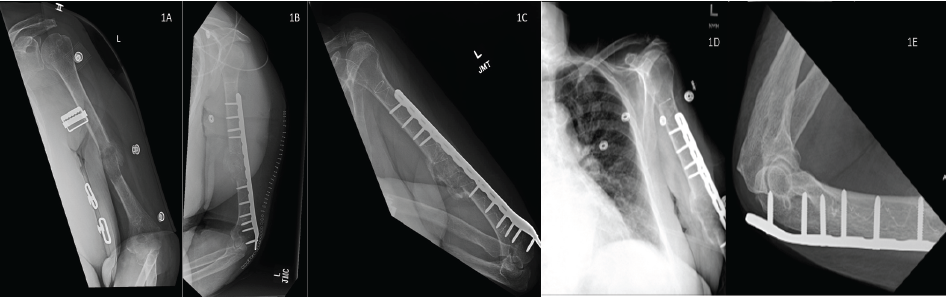
Figure 1: Left Humerus X-ray. (a) Anteroposterior X-ray of left humerus upon initial presentation to orthopedic clinic. (b) Lateral X-ray of left humerus several hours after surgical fixation, 2 weeks after image 1a. (c) Lateral X-ray of left humerus 6 months after surgical fixation. (d) Anteroposterior X-ray of the chest, including the left proximal to midshaft humerus, 1.5 years after surgical fixation. (e) Lateral X-ray of the left elbow, 1 year and 4 months after surgical fixation.
The surgery was successful, and the patient recovered well, reporting minimal pain with improvements in strength and motion in the left shoulder and elbow. Post-operative imaging, as shown in Fig. 1b, demonstrated increased bony callus at the fracture site, and the patient was instructed to continue load-bearing as tolerated for activities of daily living. One month following surgery, the patient began chemotherapy with intravenous nivolumab every 14 days and oral cabozantinib 40 mg daily. She tolerated the chemotherapy well, without any adverse reactions. At 6 months (Fig. 1c) and more than 1½ years later, the patient is doing very well in regard to the procedure, reporting good strength and motion in her left shoulder and elbow, with minimal pain. She continues weight-bearing as tolerated, and her overall recovery has been positive while she still undergoes treatment for metastatic RCC (Fig. 1d and e).
Renal metastasis to the bone is a serious and relatively common complication of RCC, accounting for an estimated 20–35% of RCC metastases [3]. Pathologic fractures due to RCC often present insidiously, and any suspicious bone lesion in a patient without a history of trauma should be investigated further for signs of malignancy. Pathologic fractures due to metastasis are becoming a more significant clinical challenge as advancements in cancer therapy extend patient survival. Their increased frequency in the setting of prolonged survivorship highlights the ongoing need for both effective preventative measures and durable treatment options [7]. Surgical fixation with the IS photodynamic bone stabilization system in combination with extra-articular plating was shown to be effective in this patient over the course of several months. This approach allowed for both internal and external fixation, which may reduce the risk of loosening or osteolysis that could compromise the repair. The standard method for fixation of a humeral fracture due to metastasis involves locking titanium screws, although other groups have been exploring the indications for using IS in pathologic fractures [8].
The IS photodynamic bone stabilization system uses a small conforming balloon attached to a catheter that is placed into the medullary canal. After correct placement, the balloon is filled with a light-curable monomer that hardens after exposure to a specific wavelength of light. The hardened monomer then provides intramedullary stabilization similar to an IMN. Indications for use include fixation of “traumatic, fragility, pathological, and impending pathological fractures of the humerus, radius, and ulna” in skeletally mature patients. The IS is not intended for use in pediatric populations, whereas a relative contraindication would include IS use alone for treatment of completed pathological fractures without a secondary form of fixation [12,13]. One recent study demonstrated that surgery is the preferred treatment for malignant bone tumors, regardless of the patient’s prognosis [14]. Surgical intervention in pathological fractures may even be recommended with multiple known bony metastatic lesions, as survival rates are similar to single metastatic bone lesions [15]. Surgical planning for bone metastasis should always take into consideration the patient’s life expectancy, the origin of the neoplasm, whether this metastasis is restricted to the bone, the number of metastatic sites, and available chemotherapy and radiation options. Radiation therapy is the primary treatment for metastatic bone cancer, whereas surgery may be used to improve stabilization and facilitate fixation of pathologic fractures, ultimately enabling a better quality of life for the patient [7,16]. In this 74-year-old patient, the symptoms of vague humeral pain with possible cervical radiculopathy persisted in her left proximal humerus for months before a diagnosis was made. The symptoms were not mentioned in the documentation until the patient presented to the ED. She did not have a diagnosis of RCC until receiving a complete workup following the ED presentation, around the time the metastatic bone lesion was noted. Ideally, this patient would have received diagnostic imaging closer to the onset of the arm pain, but there is no indication that the patient sought treatment for the pain until it became severe. Earlier disclosure of the pain could have detected malignancy and decreased the risk of pathologic fracture with appropriate interventions. A recent study of 344 patients published in 2020 showed that overall survival was 19 months and 57 months for patients classified as poor and intermediate to good prognosis, respectively [17]. This supports the decision to pursue surgical fixation of a fracture due to metastasis if it aligns with the desires of the patient and improves quality of life, as in this case. In a clinical trial on behalf of IlluminOss, it was suggested that use of IS alone was better suited for impending fractures, while use of IS with additional plating could be a better option for completed pathological fractures [13]. The IS shows promise for improving traditional surgical approaches to pathologic fractures, such as in this case, where speed of recovery and complications need to be minimized before starting treatment of the primary pathology, such as RCC in this case. More research is needed to determine if the data shown in the clinical trial can be replicated and how the use of IS can improve patient outcomes in the setting of pathological fracture.
RCC is a cancer that commonly has the sequelae of bone metastasis and pathologic fractures. This case report details the treatment of a patient who presented with a left humeral fracture of the distal third of the bone resulting from undiagnosed RCC. The fracture was successfully treated with the IS implant for stabilization of the bone. This system offers a treatment for stabilization of pathologic fractures where the deterioration of the bone causes traditional fracture treatments to be less successful.
This case highlights a promising treatment, the IlluminOss System (IS) implant, for a pathological humeral fracture. IS is a patient-conforming method, allowing for the necessary bone stability to repair the fracture.
References
- 1. Casadei R, Drago G, Di Pressa F, Donati D. Humeral metastasis of renal cancer: Surgical options and review of literature. Orthop Traumatol Surg Res 2018;104:533-8. [Google Scholar] [PubMed]
- 2. Bahadoram S, Davoodi M, Hassanzadeh S, Bahadoram M, Barahman M, Mafakher L. Renal cell carcinoma: An overview of the epidemiology, diagnosis, and treatment. G Ital Nefrol 2022;39:2022-vol3. [Google Scholar] [PubMed]
- 3. Umer M, Mohib Y, Atif M, Nazim M. Skeletal metastasis in renal cell carcinoma: A review. Ann Med Surg (Lond) 2018;27:9-16. [Google Scholar] [PubMed]
- 4. Damron TA, Mann KA. Fracture risk assessment and clinical decision making for patients with metastatic bone disease. J Orthop Res 2020;38:1175-90. [Google Scholar] [PubMed]
- 5. Tsukamoto S, Kido A, Tanaka Y, Facchini G, Peta G, Rossi G, et al. Current overview of treatment for metastatic bone disease. Curr Oncol 2021;28:3347-72. [Google Scholar] [PubMed]
- 6. Wolanczyk MJ, Fakhrian K, Adamietz IA. Radiotherapy, bisphosphonates and surgical stabilization of complete or impending pathologic fractures in patients with metastatic bone disease. J Cancer 2016;7:121-4. [Google Scholar] [PubMed]
- 7. Anract P, Biau D, Boudou-Rouquette P. Metastatic fractures of long limb bones. Orthop Traumatol Surg Res 2017;103:S41-51. [Google Scholar] [PubMed]
- 8. Zoccali C, Attala D, Pugliese M, Di Uccio AS, Baldi J. The IlluminOss® photodynamic bone stabilization system for pathological osteolyses and fractures of the humerus: Indications, advantages and limits in a series of 12 patients at 24 months of minimum follow-up. BMC Musculoskelet Disord 2021;22:63. [Google Scholar] [PubMed]
- 9. Griggers JI, Alcantar S, Gonzalez MR, Lozano-Calderon SA. Postoperative complications of intramedullary nailing for impending and pathologic fractures of the humerus due to bone metastases-a systematic review of the literature. J Surg Oncol 2025;131:932-41. [Google Scholar] [PubMed]
- 10. Colello MJ, Hunter MD, Tanner SL, Porter SE. Intramedullary nail fixation for the treatment of pathologic humeral shaft fractures. Orthopedics 2020;43:e389-98. [Google Scholar] [PubMed]
- 11. Chen BK, Tai TH, Lin SH, Chen KH, Huang YM, Chen CY. Intramedullary nail vs. Plate fixation for pathological humeral shaft fracture: An updated narrative review and meta-analysis of surgery-related factors. J Clin Med 2024;13:755. [Google Scholar] [PubMed]
- 12. IlluminOss Photodynamic Bone Stabilization System: Surgical Technique Guide – Humerus, Radius and Ulna. IlluminOss, Inc.; 2019. Available from: https://illuminoss.com/uploads/nuggets/5eaa859f7ee3385fc186902b/2019-All/forearm/surgical-technique-pdf. Accessed September 4, 2025. [Google Scholar] [PubMed]
- 13. Terek RM, IlluminOss Study Group, McGough R, Fabbri N, Cheung F, Brigman B, et al. IlluminOss photodynamic bone stabilization system improves pain and function in the treatment of humeral metastatic disease. Bone Joint J 2024;106-B:1485-92. [Google Scholar] [PubMed]
- 14. Hashimoto K, Nishimura S, Ito T, Kakinoki R, Goto K. Efficacy of surgical intervention in treating pathological fractures of the upper extremity: A retrospective case series. Cureus 2024;16:e71273. [Google Scholar] [PubMed]
- 15. Cappellari A, Trovarelli G, Crimì A, Pala E, Angelini A, Berizzi A, et al. New concepts in the surgical treatment of actual and impending pathological fractures in metastatic disease. Injury 2023;54 Suppl 1:S31-5. [Google Scholar] [PubMed]
- 16. Cirstoiu C, Cretu B, Iordache S, Popa M, Serban B, Cursaru A. Surgical management options for long-bone metastasis. EFORT Open Rev 2022;7:206-13. [Google Scholar] [PubMed]
- 17. Voog E, Campillo-Gimenez B, Elkouri C, Priou F, Rolland F, Laguerre B, et al. Long survival of patients with metastatic clear cell renal cell carcinoma. Results of real life study of 344 patients. Int J Cancer 2020;146:1643-51. [Google Scholar] [PubMed]