Bilateral anterior shoulder dislocation (BASD) is a rare clinical entity. Prompt diagnosis with radiography, timely closed reduction, and tailored rehabilitation can yield excellent outcomes in seizure-related BASD.
Dr. Vejaya Kumar, Department of Orthopaedics, Vinayaka Mission’s Medical College and Hospital, Vinayaka Mission’s Research Foundation (Deemed to be University), Karaikal, India. E-mail: dr.vejay87@gmail.com
Introduction: Bilateral anterior shoulder dislocation (BASD) is an exceptionally rare clinical entity, especially when associated with epileptic seizures. Seizure-related shoulder dislocations are predominantly posterior due to the forceful contraction of internal rotator muscles; anterior dislocations following seizures are unusual and typically result from secondary trauma during a convulsive collapse.
Case Report: This case report describes a 32-year-old male with a known history of epilepsy who presented with simultaneous BASDs immediately after a generalized tonic-clonic seizure. Clinical examination revealed the classic signs of anterior dislocation, including loss of normal shoulder contour, squared-off appearance (Epaulet sign), and humeral heads palpable anteriorly in the deltopectoral grooves. Radiographs confirmed bilateral subcoracoid anterior dislocations without associated fractures. The patient was successfully treated with closed reduction under intravenous sedation using the Kocher’s maneuver, followed by immobilization and structured rehabilitation. At 1 year of final follow-up, functional outcomes were excellent, with full pain-free range of shoulder motion and no instability episodes.
Conclusion: For uncomplicated BASD cases, closed reduction with prompt immobilization and physiotherapy remains the mainstay of management. Control of the underlying seizure disorder is crucial to prevent recurrence. This report adds to the limited literature on this rare presentation, emphasizing diagnostic challenges, management strategies, and outcomes associated with BASD in the context of epilepsy.
Keywords: Bilateral anterior, shoulder dislocation, bilateral anterior shoulder dislocation, seizure, closed reduction.
Shoulder dislocation is the most frequently encountered large‑joint dislocation, accounting for nearly 45–50% of all dislocations. The vast majority is unilateral and anterior [1,2]. Bilateral involvement raises concern for an unusual injury mechanism, and when it occurs, is more commonly posterior, often induced by violent involuntary muscle contractions during seizures or convulsions. Bilateral anterior shoulder dislocations (BASD), by contrast, are distinctly uncommon and usually associated with significant trauma, sports injuries, or occasionally seizures.
Patients presenting after seizures may not recall the trauma or fall, rendering the diagnosis difficult. Delay in recognition can result in chronic dislocation, functional impairment, and higher complexity in management. We present a rare case of simultaneous BASD in a middle‑aged male following an epileptic seizure, treated successfully with closed reduction and immobilization.
A 32‑year‑old male was brought to the emergency department with complaints of pain and inability to move both shoulders after an episode of generalized tonic–clonic seizure at home. The patient was a known epileptic on irregular antiepileptic therapy. There was no preceding trauma, electrocution, or substance use.
On examination, both shoulders demonstrated loss of normal contour with a characteristic squared‑off appearance (Epaulets sign) (Fig. 1).

Figure 1: Clinical presentation showing the patient lying supine with both upper limbs held in abduction and external rotation after a seizure episode, illustrating the classic attitude in Bilateral Anterior shoulder dislocation.
The arms were held in mild abduction and external rotation with a visible sulcus along the lateral shoulder. Palpation revealed anterior prominence of both humeral heads in the deltopectoral groove (Fig. 2).

Figure 2: Close-up of the right shoulder, showing loss of normal deltoid contour. The examiner’s finger points to the empty glenoid cavity, highlighting the clinical sign of shoulder dislocation.
Active and passive movements were not possible and associated with excruciating pain. Distal neurovascular examination of the upper limbs was normal. No external injuries were noted on the chest or upper limbs.
Radiographs (antero‑posterior views of both shoulders) confirmed bilateral anterior dislocations of the glenohumeral joints without associated fracture (Fig. 3).
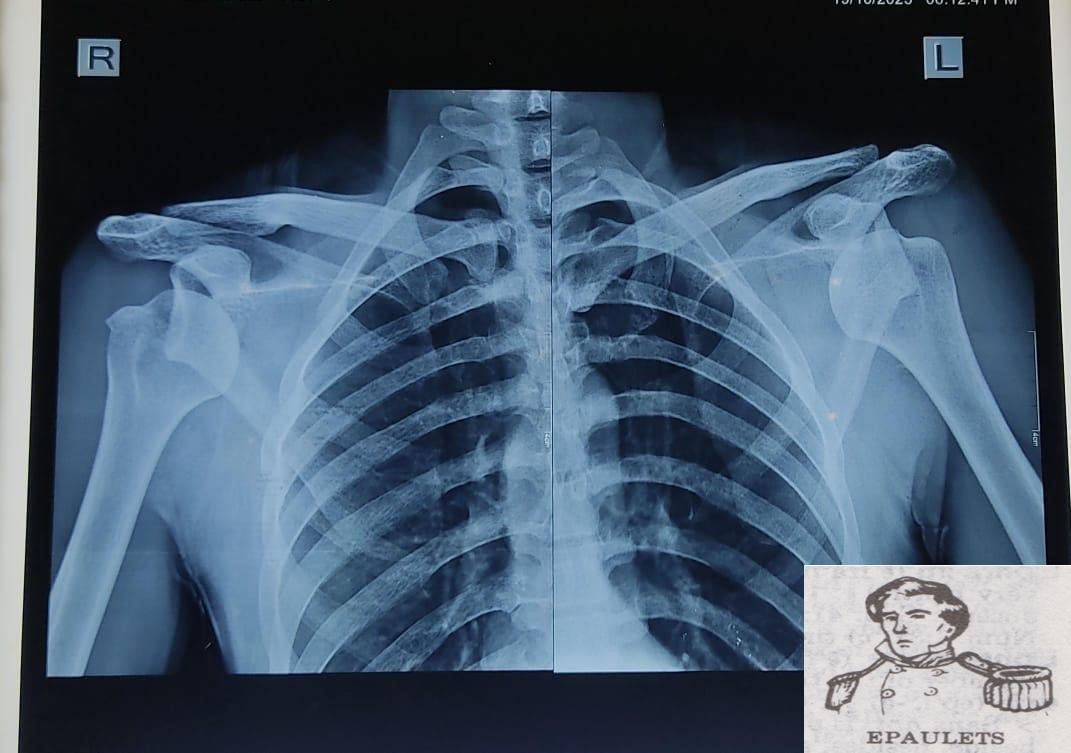
Figure 3: Pre-reduction anteroposterior radiograph showing bilateral anterior dislocation of the humeral heads (right and left) projected anterior to the glenoid fossae with squaring of both shoulders (Epaulets Sign). There is no associated fracture.
The Light bulb sign was absent. Baseline blood investigations were normal and done to rule out hypoglycemia and dyselectrolytemia.
Management
After routine pre‑anesthetic evaluation, the patient underwent closed reduction under intravenous sedation. The Kocher’s maneuver was applied sequentially to both shoulders with successful reduction confirmed clinically and radiographically (Fig. 4).
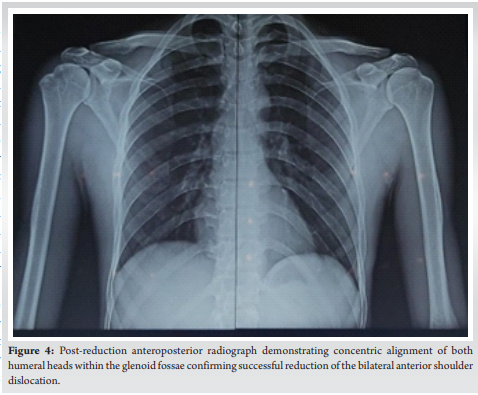 Immediate post‑reduction X‑rays showed concentric and congruent glenohumeral articulations. Both shoulders were immobilized in slings with internal rotation for 3 weeks. Early pendulum and passive range‑of‑motion exercises were started after immobilization, followed by gradual active physical rehabilitation. Epilepsy was evaluated by a neurologist and treated appropriately.
Immediate post‑reduction X‑rays showed concentric and congruent glenohumeral articulations. Both shoulders were immobilized in slings with internal rotation for 3 weeks. Early pendulum and passive range‑of‑motion exercises were started after immobilization, followed by gradual active physical rehabilitation. Epilepsy was evaluated by a neurologist and treated appropriately.
Outcome: At 1 year of final follow‑up, the patient was pain‑free with a near full range of movements bilaterally and no instability episodes. Constant shoulder scoring showed 92 on the right and 90 on the left. He was counseled on strict compliance with antiepileptic therapy to prevent recurrence.
Mechanism of Injury
The proposed mechanism differs from posterior dislocations. In seizure‑related anterior dislocation, the injury is more likely attributed to the secondary trauma of falling during convulsion, with the shoulders forced into extension, abduction, and external rotation. This position levers the humeral head anteriorly against a relatively unstable glenoid rim, resulting in anterior displacement. The synchronous impact on both shoulders explains the bilateral involvement.
BASD is an exceptionally rare clinical entity compared to unilateral anterior dislocations (Tables 1 and 2), which account for the majority of shoulder dislocations [1,2].
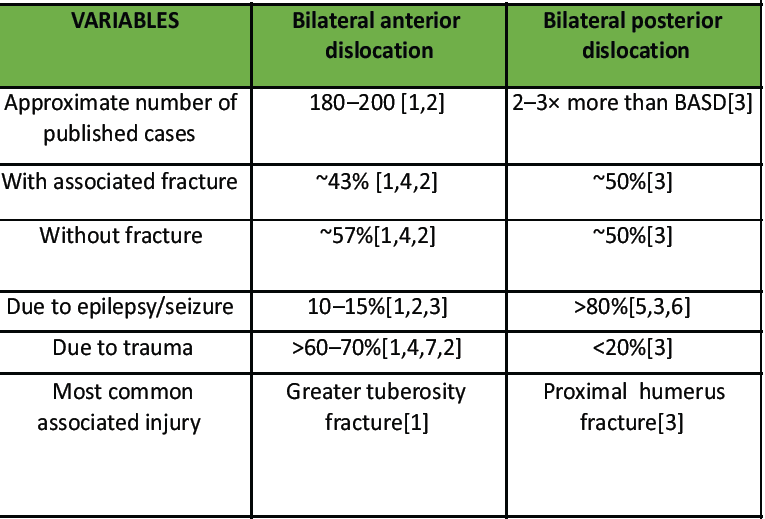
Table 1: Comparison of bilateral anterior and posterior shoulder dislocations
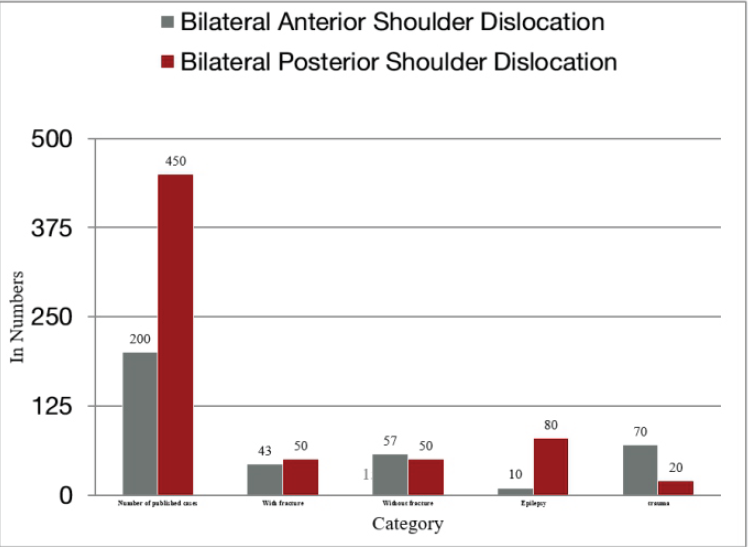
Table 2: Comparison of Bilateral Anterior and Posterior Shoulder dislocations: Case numbers and Etiologies
While most bilateral shoulder dislocations reported in literature are posterior and typically occur due to seizure-induced violent internal rotator muscle contractions, BASD following epileptic seizures is uncommon and is more often associated with direct trauma or fall during convulsions [1,2,3,4]. The diagnosis can be challenging as patients may present post-ictally with altered sensorium, and deformities might be overlooked due to the symmetric appearance and the rarity of the condition [1,4,5,6,7,8,9]. Classic clinical signs, including loss of the normal deltoid contour (Epaulet sign), arms held in abduction and external rotation, and palpable humeral heads anteriorly, aid clinical suspicion; confirmation is by anteroposterior radiographs [1,2,10]. Since Cooper and Myenter reported the first cases in 1839 and 1902, posterior shoulder dislocations have been the most common type of bilateral shoulder dislocations [11,12]. This can happen during epileptic convulsions when a violent muscle contraction dislocates the humeral head posteriorly [13]. BASD is a rare occurrence [1,2]. Trauma, nocturnal hypoglycemia, electrocution, diving, and bench pressing are some of the other reported causes of these bilateral injuries [14,15]. A 19-year-old man with a similar history was described in 2020 by Talebi et al. [16]. The patient improved by conservative management without the need for surgery. In their analysis, Diallo et al., found that 43% of BASDs were associated with complications, frequently on both sides [4].
Our case adds to the limited literature on BASD secondary to epileptic seizures by documenting a successful closed reduction and early physiotherapy without surgical intervention, achieving near full functional recovery at 3 months [1,2,9]. Unlike some reports that recommend magnetic resonance imaging (MRI) to assess soft tissue injury or associated rotator cuff tears, we did not perform MRI as the patient had no clinical signs suggestive of rotator cuff pathology or neurovascular deficits, and immediate radiographs confirmed stable concentric reduction [1,2,7,9]. Since there was no recurrence of an instability episode, MRI was deferred. This approach aligns with conservative management principles for uncomplicated BASD cases where radiographs suffice for decision-making, and MRI is reserved for suspected complications or recurrent cases [1,2,5,8].
Comparison with published data highlights that the majority of BASD cases entail associated fractures, especially of the greater tuberosity, and may require surgical stabilization [4,5,6,7]. Our patient being an exception with pure dislocation and no fracture, reinforcing that closed reduction remains standard for such uncomplicated presentations [1,2,9]. Moreover, this case reiterates that seizure-related BASD likely results from secondary trauma at the time of convulsive collapse, with the characteristic forced position of abduction and external rotation precipitating anterior displacement, contrasting the classic mechanism of internal rotation-induced posterior dislocation typically seen in seizures [3,4,5,6].
Overall, early diagnosis using clinical vigilance and timely radiographs coupled with appropriate closed reduction and tailored rehabilitation can yield excellent outcomes in seizure-related BASD [1,2,4,5,6,7,8,9]. Controlling the underlying epileptic disorder is vital for preventing recurrence, a focus echoed in recent literature [1,2,4].
Diagnostic challenges
Patients may present with confusion post‑seizure; subtle shoulder deformities might be missed. High suspicion is needed when bilateral painful restriction of movement follows a convulsive episode. Radiographs in two planes are essential to differentiate between anterior and posterior dislocations. Advanced imaging (computed tomography/MRI) is considered if associated fractures or soft tissue injuries are suspected.
Treatment and prognosis
Closed reduction under adequate analgesia is the standard of care in acute, uncomplicated cases. Immobilization for 2–3 weeks, followed by structured physiotherapy, ensures shoulder stability and mobility. Surgical stabilization may be necessary in cases with associated fractures, rotator cuff injuries, or recurrent dislocations.
Our patient achieved excellent functional recovery with non‑operative management, consistent with similar reported cases. Recurrence risk is minimized by controlling the underlying seizure disorder.
BASDs are an exceptional sequela of epileptic seizures. High clinical vigilance is required, particularly when a middle‑aged male presents with painful restriction of both shoulders following convulsions. Prompt diagnosis with radiography and timely closed reduction can yield excellent functional recovery. Education on seizure control and treatment compliance is critical in mitigating the recurrence.
BASD is an exceptionally rare clinical entity compared to unilateral anterior dislocations. The diagnosis can be challenging as patients may present post-ictally with altered sensorium, and deformities might be overlooked due to the symmetric appearance and the rarity of the condition. Early diagnosis using clinical vigilance and timely radiographs, coupled with appropriate closed reduction and tailored rehabilitation, can yield excellent outcomes in seizure-related BASD. Controlling the underlying epileptic disorder is vital for preventing recurrences.
References
- 1. Meena S, Saini P, Singh V, Kumar R, Trikha V. Bilateral anterior shoulder dislocation. J Nat Sci Biol Med 2013;4:499-501. [Google Scholar] [PubMed]
- 2. Akar B. Bilateral anterior shoulder dislocation: A case report. Ulus Travma Acil Cerrahi Derg 2024;30:761-3. [Google Scholar] [PubMed]
- 3. Siu YC, Lui TH. Bilateral anterior shoulder dislocation. Arch Trauma Res 2014;3:e18178. [Google Scholar] [PubMed]
- 4. Diallo M, Soulama M, Kaboré DS, Dakouré PW, Liverneaux P. Bilateral anterior shoulder dislocations: A review of two cases and the relevant literature. Clin Case Rep 2020;8:3379-88. [Google Scholar] [PubMed]
- 5. Kulkarni M, Shetty S, Vijayan S, Rao SK. Bilateral anterior glenohumeral dislocation: Two rare scenarios and pathomechanics. Indian J Orthop Surg 2020;6:259-62. [Google Scholar] [PubMed]
- 6. Dlimi F, Rhanim A, Lahlou A, Kharmaz M, Ouadghiri M, El Bardouni A, et al. Bilateral anterior dislocation of the shoulders at the start of a backstroke competition. J Orthop Traumatol 2012;13:47-9. [Google Scholar] [PubMed]
- 7. Ballesteros R, Benavente P, Bonsfills N, Chacón M, García-Lázaro FJ. Bilateral anterior dislocation of the shoulder: Review of seventy cases and proposal of a new etiological-mechanical classification. J Emerg Med 2013;44:269-79. [Google Scholar] [PubMed]
- 8. Cresswell TR, Smith RB. Bilateral anterior shoulder dislocations in bench pressing: An unusual cause. Br J Sports Med 1998;32:71-2. [Google Scholar] [PubMed]
- 9. Dunlop CC. Bilateral anterior shoulder dislocation–a case report and review of the literature. Acta Orthop Belg 2002;68:168-70. [Google Scholar] [PubMed]
- 10. Singh S, Kumar S. Bilateral anterior shoulder dislocation: A case report. Eur J Emerg Med 2005;12:33-5. [Google Scholar] [PubMed]
- 11. Cooper A. A Treatise on Dislocations and Fractures of the Joints. Philadelphia PA: Blanchard and Lea; 1851. [Google Scholar] [PubMed]
- 12. Mynter H. XIV. Subacromial dislocation from muscular spasm. Ann Surg 1902;36:117-9. [Google Scholar] [PubMed]
- 13. Thomas T, Noel E, Bouvier M. Pitfall of stiff shoulder: Inveterated posterior dislocation. Clin Rheumatol 1995;14:467-70. [Google Scholar] [PubMed]
- 14. Abdelaziz G. Acute bilateral anterior shoulder dislocation after an epileptic seizure: A case report. EC Ortho-Paedics 2020;11:59-61. [Google Scholar] [PubMed]
- 15. Choulapalle R, Chokkarapu R, Kolluri RK, Anne SR, Perumal SR, Avadhanam PK, et al. A case of neglected bilateral anterior shoulder dislocation: A rare entity with unusual mechanism of injury. Case Rep Orthop 2015;2015:461910. [Google Scholar] [PubMed]
- 16. Talebi S, Teimoury A, Ghadiri A. Bilateral anterior shoulder dislocation after an episode of grand-mal seizure: A case report and literature review. J Orthop Spine Trauma 2021;7:64-6. [Google Scholar] [PubMed]










