This case report illustrates the effective and successful use of the long head of the biceps tendon to serve as autograft for superior capsular reconstruction in the setting of irreparable supraspinatus tear. In addition, the report highlights a novel method of biceps tenodesis that allows for both retention of native tendon tension as well as ample proximal tendon length for SCR autograft.
Dr. John R. Tuttle, Department of Orthopeadic Sugery, Carilion Clinic, Virginia, United States of America. E-mail: jrtuttle@carilionclinic.org
Introduction: Rotator cuff tears are a common clinical pathology increasingly markedly with age. Large to massive tears are often complex procedures due to the underlying nature of the injury.
Case Report: We present a case of a superior capsular reconstruction (SCR) utilizing the long head biceps tendon as an autograft as well as a novel arthroscopic, suprapectoral biceps tenodesis technique here on a 68-year-old male with complaints of the right shoulder pain over the previous 6 months.
Conclusion: Primary repair of a complete supraspinatus tear was attempted, but due to tendon retraction and inability to mobilize the supraspinatus back to the footprint, SCR utilizing the long head biceps tendon was performed. In addition, a novel technique of biceps tenodesis fixation utilizing an all-suture knotless anchor is used.
Keywords: Superior capsular reconstruction, rotator cuff, long head biceps tendon, arthroscopy, biceps tenodesis.
Large/massive tears represent over half of all rotator cuff (RTC) tears, and they often lead to atrophy and fatty degeneration of the RTC muscles, loss of shoulder function, and pain [1,2]. Poor tendon quality, mobility, and retraction make repairs of large tears a complex procedure [1]. When it comes to management of these large RTC tears, previous studies have shown that any alternative to complete repair are inferior and that patch grafts attached to the torn tendon have a high failure rate [3,4,5,6,7]. In a 2012 publication, Mihata presented a novel technique for surgical management of irreparable RTC tears: Superior capsular reconstruction (SCR) [8]. Since its introduction, there have been multiple efforts to improve on the SCR technique. First was the use of extracellular matrix, or dermal allograft. This technique has the advantages of decreased donor site morbidity and shorter operative times, but it also carries its own list of disadvantages. The dermal allografts are only available in 1–3 mm thickness, whereas the fascia lata autografts are typically 8 mm in thickness. Grafts at 8 mm thickness have been shown to be superior to those of 4 mm in thickness [9,10]. In addition, the allografts had decreased tissue incorporation on histological analysis [11].
A more novel technique for SCR is use of the long head of the biceps tendon (LHBT) to stabilize the superior shoulder capsule. In this technique, the LHBT origin on the supraglenoid tubercle is left intact and the LHBT is anchored to the greater tuberosity [12,13]. The distal portion of the LHBT can then be managed through tenotomy or tenodesis. This alternative technique overcomes the problems of donor site morbidity, viability of the autograft, and additional costs of the allograft [14]. It is also more efficient given the biceps graft does not require glenoid fixation. In 2021, Kitridis et al. conducted a literature review to evaluate this new technique. Some of the reported advantages of utilizing the LHBT include increased vascularity with improved healing rates incorporation of tissue that is rich in live tenocytes and fibroblasts, lower cost, no donor site morbidity, reduced inflammatory reactions compared to allografts, decreased infection rate, and shorter operative times [15]. In addition, the mean diameter of the LHBT is 6.6 mm which is closer to the 8 mm graft thickness that has previously been shown to be superior than what is currently available in dermal allografts [15]. The LHBT is not as wide as the fascia lata or dermal graft; however, biomechanical studies thus far have shown that this technique still re-centers the humeral head on the glenoid and prevents humeral migration to the same degree as the fascia lata autograft [16,17,18,19]. The major disadvantage associated with this technique is that it cannot be utilized in patients with significant pathosis to the LHBT or superior labrum, or prior tenotomy or tenodesis. In the following report, we present a case in which primary repair of a RTC tear was attempted, but due to tendon retraction and inability to mobilize the supraspinatus back to the footprint, SCR utilizing the LHBT was performed. This was in conjunction with a novel technique for biceps tenodesis, which left the proximal attachment in place, where it was able to be utilized as a tendon graft for the SCR. This biceps tenodesis technique was performed before the release of the tendon, allowing for anatomic tension to the biceps muscle to be maintained.
A 68-year-old male presented with complaints of the right shoulder pain over the previous 6 months after a fall from his bicycle. Following negative X-rays (Fig. 1), he initially elected to proceed with an intra-articular injection and physical therapy, with plans to obtain a magnetic resonance imaging (MRI) if no improvement occurred. He noted initial improvement but returned 6 months later due to recurrence of pain. Subsequent MRI revealed a full-thickness tear of the supraspinatus tendon with 4.5 cm of retraction, as well as tendinosis of the infraspinatus, subscapularis, and biceps tendon.
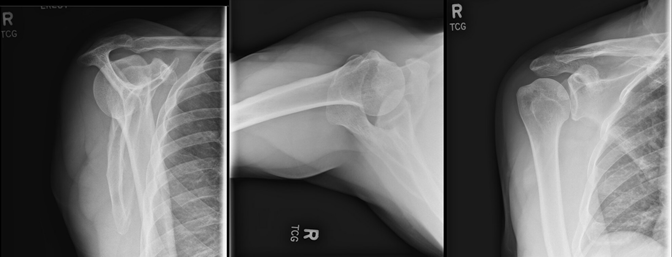
Figure 1: X-ray lateral, superior-inferior axial, and anteroposterior view. Joint bases are well preserved without significant osteoarthritis. No fractures, dislocation, or loose body seen.
Examination at the time revealed 4/5 weakness of the supraspinatus, tenderness over the LHBT and AC joint, and positive Neer, Hawkins, and cross-body adduction signs. Surgical treatment options were discussed and the patient elected to proceed with a right shoulder arthroscopy, RTC repair, distal clavicle excision, decompression, and biceps tenodesis. Informed consent was obtained. The surgical technique was performed with the patient in beach chair position under general anesthesia. A posterior arthroscopic portal was created, and no changes were noted on the glenoid or humeral articular surfaces. The labrum was intact. An anterior portal was created through an outside-in fashion in the rotator interval. The LHBT was intact but erythematous distally. The subscapularis was intact with no loose bodies in the subscapularis recess. The articular surface of the supraspinatus revealed a complete tear with retraction to the glenoid with scarring and poor mobilization. The infraspinatus and teres minor were intact and there were no loose bodies or other abnormalities in the axillary pouch. A standard arthroscopic decompression was carried out followed by an arthroscopic distal clavicle excision. Attention was then returned to the RTC tear. Mobilization of the cuff in the scapulohumeral and intra-articular planes was performed with a liberator and traction suture. An interval slide was performed. The supraspinatus tissue quality was poor and did not mobilize to the footprint despite these maneuvers. The decision was then made to use the biceps tendon as a superior capsular autograft as no allograft was available at the surgery center due to cost. Attention was then turned to the anterior shoulder and proximal arm, viewing from the lateral portal. The subacromial tissue was debrided to allow for visualization, and the superior border of the pectoralis major tendon was identified. The biceps tendon was located and the synovial sheath was released (Fig. 2a). The tenodesis site was prepared with a shaver and cautery to remove surrounding soft tissue and allow the tendon to sit directly on the humeral cortex. A 1.8 mm knotless all-suture anchor was placed through the center of the biceps tendon and anchored into bone after a pilot hole was created using the appropriate drill. The passing stitch was then looped around the lateral half of the tendon and secured back through the anchor and tensioned to complete the tenodesis (Fig. 2b). The arthroscope was repositioned to the posterior portal. The greater tuberosity was prepared to bleeding bone. The biceps tendon was released as it enters the transverse ligament. The biceps tendon was then captured with 2 fiber link sutures and anchored to the greater tuberosity with a 4.75 mm knotless, biocomposite anchor (Fig. 2c, d, e, f). The subscapularis and infraspinatus were then repaired to the biceps tendon in a side to side repair.
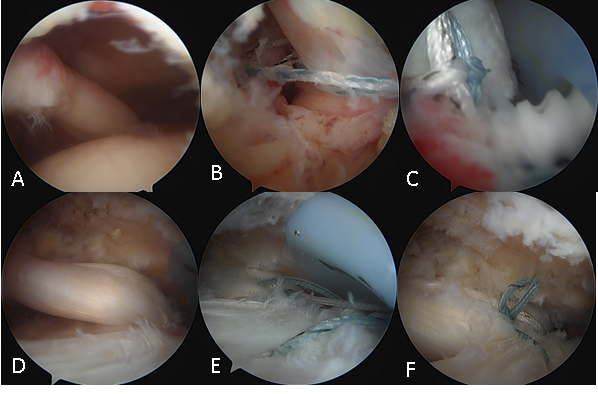
Figure 2: Intraoperative images. (a) Long head biceps tendon before intervention. (b) All-suture knotless anchor in place and passed around tendon for biceps tenodesis, just before tensioning. (c) Biocomposite, 4.75 mm knotless anchor being placed at greater tuberosity loaded with two Fiberlink sutures attached to distal end of the biceps SCR autograft. (d) Completed biceps SCR autograft fixation. (e) Sutures passed before tying between infraspinatus and biceps autograft SCR. (f) Completed side to side repair of biceps to infraspinatus tendon.
The patient went home with an abduction sling in place. He reported consistent improvement in his pain at his 1-week appointment and resolution of his pain and full passive range of motion at 6 weeks post-operative at which time physical therapy was initiated and the sling was discontinued. At the 12-week follow-up, he had full active range of motion, including forward elevation and abduction, noting mild pain with increased movement that had been improving with time and physical therapy. At 4.5 months, the patient noted no pain, full motion, was finished with physical therapy and back to his normal exercise routine, including weight lifting and riding his bicycle. He had no impingement signs on his exam and 5/5 supraspinatus strength at this visit. At 6 months, he continued to do well and was discharged to activity as tolerated (Fig. 3). He continues to do well without symptoms 18 months from the operation (Fig. 4).
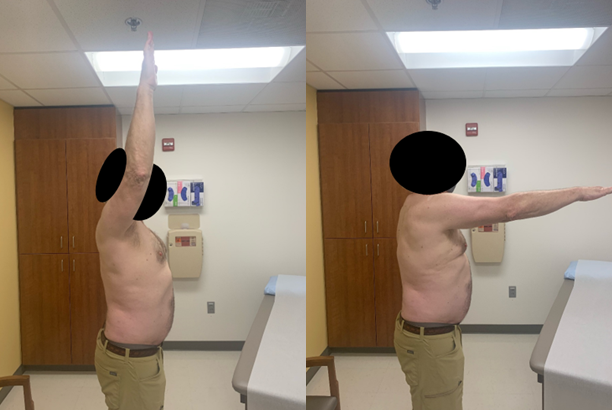
Figure 3: Clinical pictures at 6 months. Post-operative range of motion is demonstrated with full forward elevation and excellent control and strength with active elevation despite an irreparable supraspinatus tendon.
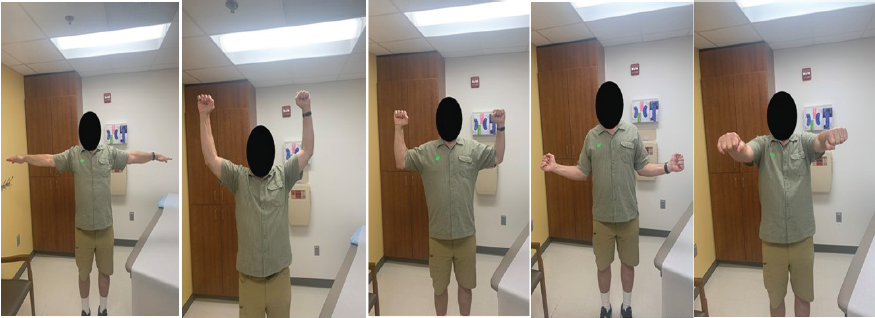
Figure 4: Clinical pictures at 18 months. Post-operative range of motion is demonstrated with full abduction, forward elevation, rotation, and excellent control and strength with active elevation despite an irreparable supraspinatus tendon.
Over recent years, SCR has become an emerging technique for previously irreparable RTC tears [4]. The use of the LHBT has shown great promise due to its increased strength and faster remodeling and ingrowth as well as a decreased risk of infection as it is native tissue. In addition, it allows for a more efficient repair as well as decreased cost of allograft tissue but with similar mechanical strength [1]. The novel technique used for biceps tenodesis provides several benefits: Ease of surgical execution, decreased operative times, smaller osseous tunnel, and maintenance of the natural length-tension relationship on the biceps muscle. To maintain the anatomic length-tension relationship, the biceps tenodesis was performed before the release of the tendon. The most important advantage for this technique is the ability to secure the biceps tendon distally, preserving a large portion of proximal tendon to be used as autograft for the SCR procedure. The benefits of biceps autograft for SCR in an ambulatory surgical setting without access to dermal allografts due to cost must be highlighted. This procedure saved the patient from a second surgical site in which the fascia lata would have had to be harvested. Alternatively, it saved the patient from a second surgery in which a dermal allograft could be made available. This technique allowed for decreased operative time, decreased implant cost, and likely decreased infection risk [20].
This case represents the successful execution of an alternative way to perform biceps tenodesis while allowing adequate tissue for biceps autograft SCR. Our patient was a good candidate for this technique because he had healthy LHBT tissue, there was no superior labral tear, and the subscapularis and infraspinatus tissue were intact and viable. While this technique has shown multiple advantages thus far, further study is required to determine its full indications and disadvantages.
In this case, primary repair of a complete supraspinatus tear was attempted, but due to tendon retraction and inability to mobilize the supraspinatus back to the footprint, SCR utilizing the LHBT was performed. In addition, a novel technique of biceps tenodesis fixation utilizing an all-suture knotless anchor is used, allowing for maintenance of the natural length-tension relationship at the biceps muscle as well as adequate tissue for transposition to use for the SCR.
References
- 1. Adrian SC, Field LD. Biceps transposition for biological superior capsular reconstruction. Arthrosc Tech 2020;9:e841-6. [Google Scholar] [PubMed]
- 2. Obma PR. Free biceps tendon autograft to augment arthroscopic rotator cuff repair. Arthrosc Tech 2013;2:e441-5. [Google Scholar] [PubMed]
- 3. Audenaert E, Van Nuffel J, Schepens A, Verhelst M, Verdonk R. Reconstruction of massive rotator cuff lesions with a synthetic interposition graft: A prospective study of 41 patients. Knee Surg Sports Traumatol Arthrosc 2006;14:360-4. [Google Scholar] [PubMed]
- 4. Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am 2010;92:1894-908. [Google Scholar] [PubMed]
- 5. Moore DR, Cain EL, Schwartz ML, Clancy WG Jr. Allograft reconstruction for massive, irreparable rotator cuff tears. Am J Sports Med 2006;34:392-6. [Google Scholar] [PubMed]
- 6. Sclamberg SG, Tibone JE, Itamura JM, Kasraeian S. Six-month magnetic resonance imaging follow-up of large and massive rotator cuff repairs reinforced with porcine small intestinal submucosa. J shoulder Elbow Surg 2004;13:538-41. [Google Scholar] [PubMed]
- 7. Soler JA, Gidwani S, Curtis MJ. Early complications from the use of porcine dermal collagen implants (Permacol) as bridging constructs in the repair of massive rotator cuff tears. A report of 4 cases. Acta Orthop Belg 2007;73:432-6. [Google Scholar] [PubMed]
- 8. Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 2013;29:459-70. [Google Scholar] [PubMed]
- 9. Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy 2018;34:93-9. [Google Scholar] [PubMed]
- 10. Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical effect of thickness and tension of fascia lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy 2016;32:418-26. [Google Scholar] [PubMed]
- 11. Athanasiou VT, Papachristou DJ, Panagopoulos A, Saridis A, Scopa CD, Megas P. Histological comparison of autograft, allograft-DBM, xenograft, and synthetic grafts in a trabecular bone defect: An experimental study in rabbits. Med Sci Monit 2010;16:BR24-31. [Google Scholar] [PubMed]
- 12. Sano H, Mineta M, Kita A, Itoi E. Tendon patch grafting using the long head of the biceps for irreparable massive rotator cuff tears. J Orthop Sci 2010;15:310-6. [Google Scholar] [PubMed]
- 13. Veen EJ, Stevens M, Diercks RL. Biceps autograft augmentation for rotator cuff repair: A systematic review. Arthroscopy 2018;34:1297-305. [Google Scholar] [PubMed]
- 14. Boutsiadis A, Chen S, Jiang C, Lenoir H, Delsol P, Barth J. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: “The Chinese way.” Arthrosc Tech 2017;6:e1559-66. [Google Scholar] [PubMed]
- 15. Kitridis D, Yiannakopoulos C, Sinopidis C, Givissis P, Galanis N. Superior capsular reconstruction of the shoulder using the long head of the biceps tendon: A systematic review of surgical techniques and clinical outcomes. Medicina (Kaunas) 2021;57:229. [Google Scholar] [PubMed]
- 16. El-shaar R, Soin S, Nicandri G, Maloney M, Voloshin I. Superior capsular reconstruction with a long head of the biceps tendon autograft: A cadaveric study. Orthop J Sport Med 2018;6:2325967118785365. [Google Scholar] [PubMed]
- 17. Han F, Kong CH, Hasan MY, Ramruttun AK, Kumar VP. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res 2019;105:257-63. [Google Scholar] [PubMed]
- 18. Han SY, Lee TQ, Wright DJ, Park IJ, Mauro M, McGarry MH, et al. Effect of biceps rerouting technique to restore glenohumeral joint stability for large irreparable rotator cuff tears: A cadaveric biomechanical study. J Shoulder Elbow Surg 2020;29:1425-34. [Google Scholar] [PubMed]
- 19. Park MC, Itami Y, Lin CC, Kantor A, McGarry MH, Park CJ, et al. Anterior cable reconstruction using the proximal biceps tendon for large rotator cuff defects limits superior migration and subacromial contact without inhibiting range of motion: A biomechanical analysis. Arthroscopy 2018;34:2590-600. [Google Scholar] [PubMed]
- 20. Kim D, Jang Y, Park J, On M. Arthroscopic superior capsular reconstruction with biceps autograft: Snake technique. Arthrosc Tech 2019;8:e1085-92. [Google Scholar] [PubMed]