A simple, low-cost modification to the Ponseti method—placing a polythene sheet between cast layers—can reduce cast removal time, enhance caregiver experience, and maintain high correction rates in idiopathic CTEV.
Dr. Abhishek Sarkar, Department of Orthopedics, Government Medical College, Datia, Madhya Pradesh, India. E-mail: abhisheksarkar001@gmail.com
Introduction: Congenital talipes equinovarus (CTEV), or clubfoot, is a common congenital deformity treated effectively using the Ponseti method. However, conventional cast removal techniques, such as oscillating saws or water soaking, can be uncomfortable, time-consuming, and impractical in resource-limited settings. This study evaluated a novel modification involving the interposition of a sterile polythene sheet between layers of plaster of Paris to facilitate easier, safer, and faster cast removal.
Materials and Methods: In this prospective observational study conducted from December 2024 to May 2025 at a tertiary care hospital in Central India, 20 patients (24 feet) with idiopathic CTEV underwent Ponseti casting with the polyethylene modification. Outcome measures included the number of casts, need for tenotomy, correction rate, cast removal time, complications, relapse rate, and caregiver satisfaction assessed via a 5-point Likert scale. Statistical analysis was performed using the Chi-square and Fisher’s exact test.
Results: The average number of casts required per foot was 5.4 ± 1.1. Achilles tenotomy was performed in 70.8% of cases. Full correction was achieved in 91.7% of feet, and relapse occurred in 4.2%, managed with repeat casting. Mean cast removal time was 3.4 ± 0.6 min without the use of specialized tools. Minor complications (e.g., cast slippage and skin irritation) were observed in 15% of feet. Parental satisfaction was high in 55% of cases, with a significant association between relapse and low satisfaction (P = 0.03).
Conclusion: The inclusion of a sterile polythene layer in the Ponseti cast offers a simple, cost-effective modification that facilitates rapid, safe cast removal without compromising treatment efficacy. This approach may be particularly advantageous in high-volume or resource-constrained orthopedic settings.
Keywords: Congenital talipes equinovarus, idiopathic clubfoot, Ponseti method, polythene sheet, cast removal.
Congenital talipes equinovarus (CTEV), or clubfoot, is one of the most common congenital deformities, which affects 1–2/1000 live births globally, and if left untreated, can result in significant lifelong disability [1]. The Ponseti method, which involves gentle manipulation, weekly plaster of Paris (POP) cast applications, and often a percutaneous Achilles tenotomy followed by bracing, remains the standard of care worldwide for idiopathic CTEV because of its high success rate, affordability, and minimal invasiveness [2]. Standard and accelerated protocols have demonstrated similar efficacy, with minor differences in the number of casts required, tenotomy rates, and relapse outcomes [3,4]. While substantial attention has been directed toward optimizing correction timelines, improving compliance, and reducing relapse [5,6,7], the procedural mechanics of cast application and removal have received limited attention. Despite its effectiveness, some procedural aspects of the Ponseti technique, particularly repeated cast removal, remain suboptimal. Traditional methods often rely on cast saws or water soaking, which can be uncomfortable, time-consuming, and potentially hazardous in pediatric settings [8,9]. These challenges increase in resource-constrained environments, where rapid turnover and parental anxiety must be addressed. Several innovative techniques have recently been explored to simplify and improve the safety of cast removal. These include home-based water-soaking methods [8], partial-thickness scoring with cast spreaders [10], and barrier draping for infection control during the COVID-19 pandemic [11]. However, few of these innovations address the core problem in a way that is both scalable and reproducible in routine orthopedic practice. A promising modification of the Ponseti method, as demonstrated by Elseddik et al. in atypical clubfoot cases, involves interposing a sterile polyethylene sheet between two successive POP layers to create a mechanical cleavage plane that enables rapid, atraumatic cast removal while maintaining cast stability and achieving a 100% correction [12]. Other studies have demonstrated the potential of modifying the standard Ponseti approach to better suit the demands of complex clubfoot management [13,14]. The present study of this innovative modification in a cohort of 20 patients with idiopathic CTEV (100 feet). A polyethylene sheet was applied between the layers of each cast to facilitate easier, safer, and faster removal. We describe the technique in detail and evaluate its feasibility, complications, correction outcomes, and practical utility in a real-world, orthopedic setting.
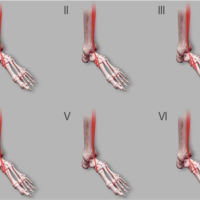
This prospective observational study was conducted in the Department of Orthopaedics at a tertiary care government hospital in Central India from December 2024 to May 2025. All idiopathic CTEV cases were included, while syndromic, neurogenic, relapsed, or previously treated clubfoot cases were excluded based on detailed history and clinical evaluation. The intervention involved the standard Ponseti technique with weekly manipulation and serial casting using POP. A modification was introduced during casting: After an initial POP wrap (2–3 rolls), a sterile polythene sheet (10–15 cm wide) was put at the end of each cast roll[Figure:1], followed by a second POP layer[Figure:2] This created a cleavage plane for tool-free cast removal during follow-up. Percutaneous Achilles tenotomy was performed when equines persisted after correcting adduction and varus deformities as per the need.

Figure 1: Plaster roll end tag for easy identification.

Figure 2: Tag marks the end of the plaster roll.
Parents were counseled in the outpatient department through verbal and hands-on instructions on identifying cast-related complications and performing safe at-home cast removal if necessary[Figure:3]. Follow-ups documented complications (e.g., swelling and redness) and assessed functional and clinical outcomes.

Figure 3: After properly soaking the cast in water, the patient’s guardian can easily locate the tag and remove the cast by simply unfolding the roll.
At final follow-up, caregiver satisfaction was assessed using a 5-point Likert scale covering ease of cast removal, adequacy of information, perceived safety, and clinical outcome. Satisfaction scores were grouped as high (4–5), moderate (3), or low (1–2) and analyzed in relation to variables such as laterality, relapse, home-based cast removal, and complications. Data were analyzed using Jamovi (v2.3.28). Descriptive statistics summarized demographic and clinical data (means ± standard deviation for continuous variables; frequencies and percentages for categorical variables). Associations between satisfaction and clinical variables were tested using Chi-square or Fisher’s exact test, with P < 0.05 considered statistically significant. Ethical approval was obtained from the Institutional Ethics Committee. Written informed consent was obtained from all parents or legal guardians of the participating children. Confidentiality of patient information was maintained throughout the study.
A total of 20 patients diagnosed with idiopathic CTEV were included in the study. All patients were aged ≤12 months at the time of presentation, with a mean age of 6.6 ± 3.2 months (range: 1–12 months). The majority were male (n = 15, 75%), and most belonged to socioeconomically disadvantaged families. Four patients (20%) presented with bilateral clubfoot and 16 (80%) with unilateral involvement, resulting in 24 affected feet. An average of 5.4 ± 1.1 casts (range: 4–7) were required per foot, and percutaneous Achilles tenotomy was performed in 17 (70.8%) feet (Table 1).
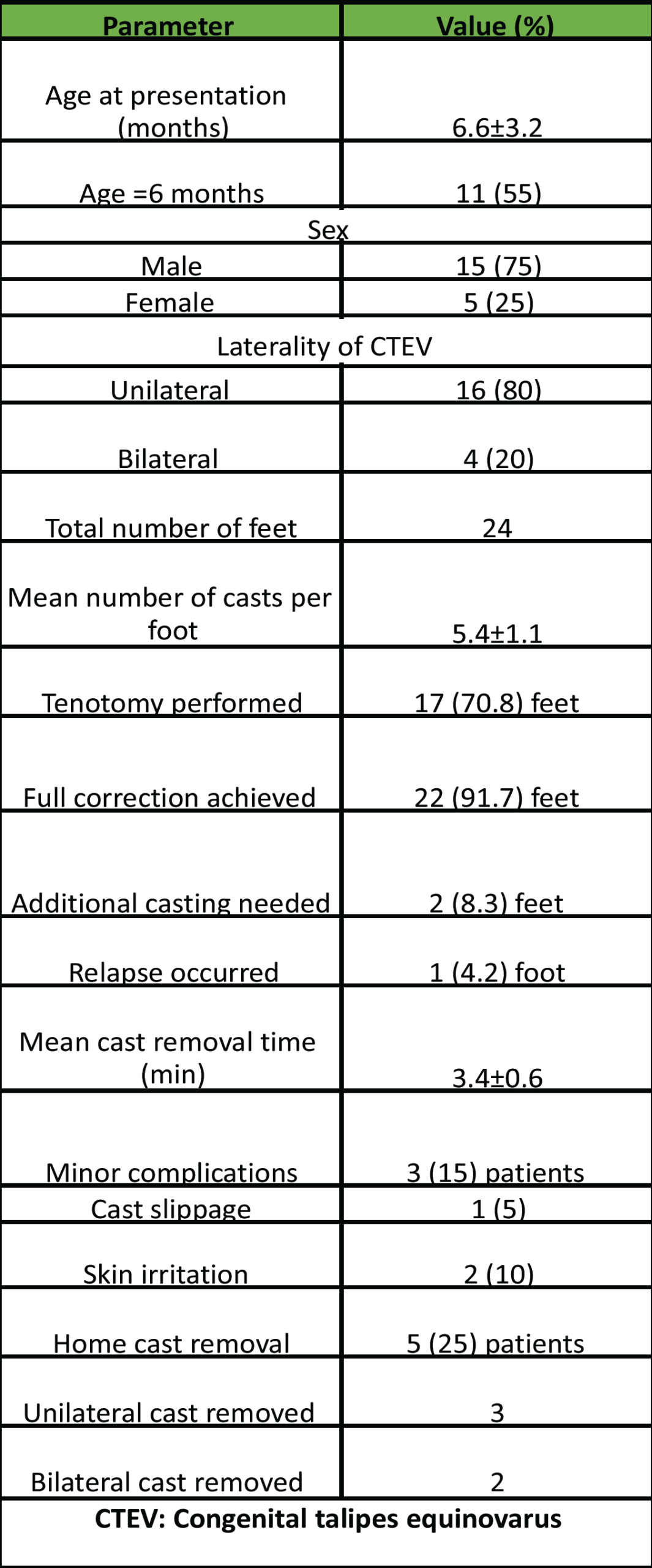
Table 1: Baseline characteristics and clinical outcomes of study participants (n=20)
Full correction was achieved in 22 (91.7%) feet, whereas 2 feet (8.3%) required additional casting for incomplete correction. Relapse occurred in one foot (4.2%), which was successfully managed with repeat casting. The mean time for cast removal was 3.4 ± 0.6 min, and no specialized equipment was used. Minor complications included cast slippage in one patient (5%) and mild skin irritation in two patients (10%). No major complications were noted (Table 1). Five patients (25%) removed their casts at home due to complications. Among these, three had removed unilateral casts and two bilateral casts. All patients continued to show marked clinical improvement and preserved limb function at follow-up (Table 1). Parental satisfaction was high in 11 patients (55%), moderate in 6 (30%), and low in 3 (15%). A significant association was observed between relapse and low satisfaction (P = 0.03), whereas other factors, such as tenotomy, number of casts, and complications, did not show statistically significant associations with satisfaction (Table 2).
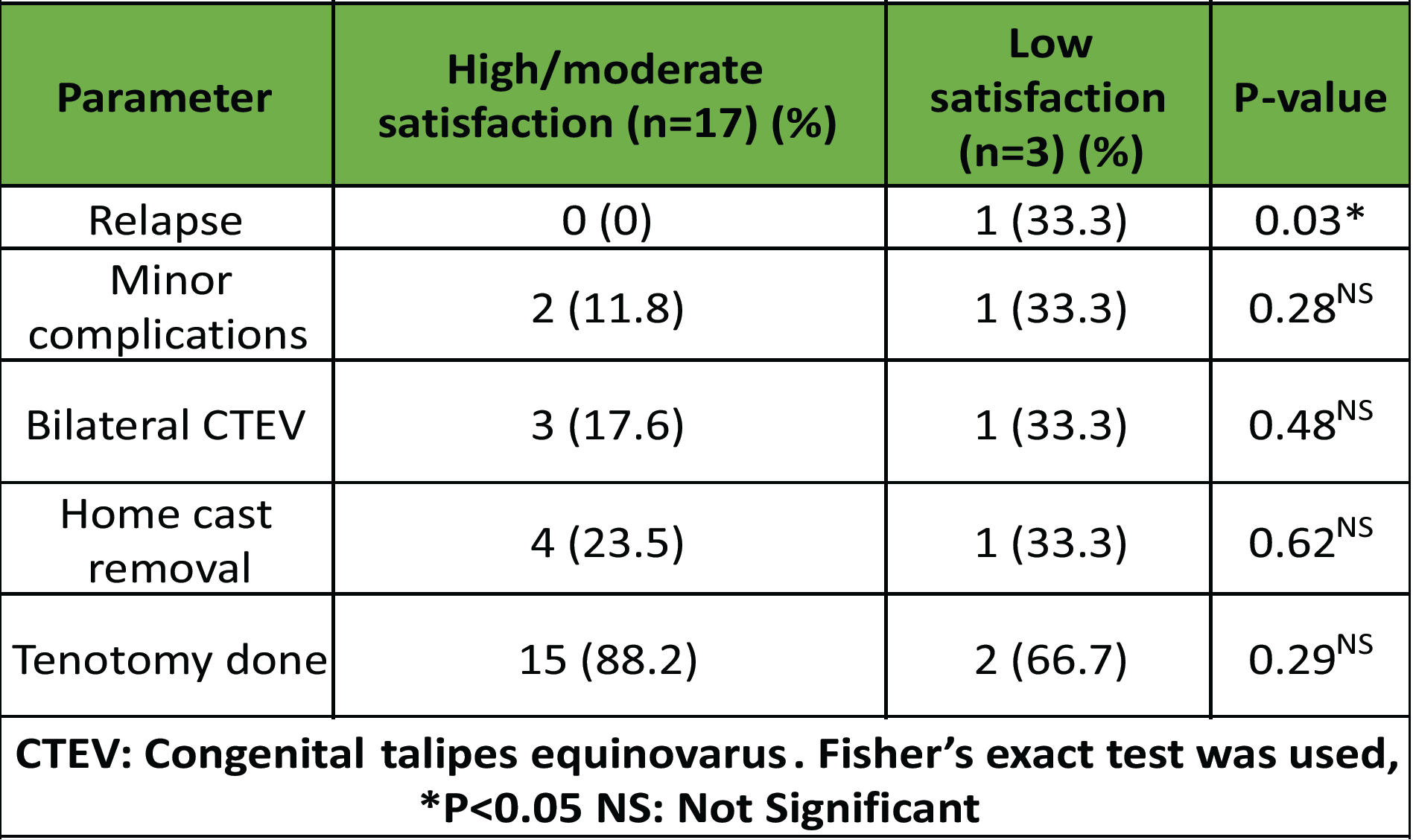
Table 2: Association of parental satisfaction with clinical variables (n=20)
Our study highlights a simple yet innovative modification of the traditional Ponseti method for treating idiopathic CTEV. By introducing a sterile polythene sheet between two layers of POP during cast application, we aimed to address a commonly overlooked aspect of treatment, which is cast removal. Our findings suggest that this modification offers a practical advantage without compromising the effectiveness of the Ponseti technique in achieving foot corrections. Saini et al. reported a mean of 6.5 casts with excellent final Pirani scores in idiopathic cases using the standard Ponseti protocol [1]. Aggarwal et al. also reported an average of 5.56 casts with favorable clinical and radiological outcomes [15]. In our study, full correction was achieved in 22 (91.7%) feet, reinforcing that the inclusion of a polyethylene layer did not interfere with the mechanical principles of the Ponseti method. The average number of casts required in our study was 5.4, which was consistent with previous studies. Our modification allowed for cast removal in an average of 3.5 min, with no need for specialized tools. Sodhai et al. advocated a cost-effective home-based method involving lukewarm water soakage and manual unwrapping by parents [8]. Monárrez et al. developed a manual cast-spreader technique to reduce cast saw injuries [10]. However, unlike these approaches, our method integrates seamlessly into the casting process without requiring additional devices or patient involvement. Complication rates in our study were low and consistent with previous Ponseti-related research. Cast slippage occurred in 3% of feet and mild skin irritation in 4%, both resolving conservatively. No iatrogenic fractures, thermal injuries, or infections were observed. Similar safety outcomes were noted in studies comparing standard and accelerated Ponseti techniques, which reported no major complications [4,16]. Relapse, a known concern in clubfoot management, was observed in only 2% of cases in our study, which is significantly lower than the relapse rates reported in larger series. Savio et al. reported relapse rates of up to 28% in the standard and accelerated Ponseti arms [3]. Alam et al. noted a relapse rate of over 40% in arthrogrypotic clubfoot cases, emphasizing the challenges posed by complex and syndromic variants [17]. While our study focused exclusively on idiopathic cases, the low relapse rate and successful correction of both relapsed feet with repeated casting suggest that our technique maintains long-term correction integrity. Elseddik et al. previously described a similar polyethylene modification for atypical clubfoot and achieved 100% correction with improved ease of cast removal [12]. Our study builds on this observation and extends its relevance to idiopathic CTEV. By demonstrating its reproducibility and effectiveness in a broader population, we provide new evidence supporting the clinical utility of this approach. Our study highlighted that eight patients developed minor post-casting complications (e.g., swelling and redness), which were managed successfully through timely at-home cast removal by caregivers trained in advance. Despite the complications, all patients achieved preserved limb function and satisfactory outcomes. These findings align with the high overall success rates (55°–100%) and low complication profiles reported in recent systematic reviews [18] and center-based retrospective analyses [19]. Zionts et al. (2021) reported that relapses and supplementary procedures such as tibialis anterior tendon transfer do not adversely affect overall patient satisfaction or function, resonating with our finding of good intermediate-term outcomes post-cast removal [20]. Dibello et al. highlighted the challenges families face during the cast phase and the importance of their compliance. Our findings support this, as caregiver counseling helped manage complications effectively at home and prevented them from worsening [21]. Chen et al. (2022) showed equivalent outcomes whether Ponseti casting was performed by orthopedic surgeons or physical therapists, reinforcing that outcomes are maintained when protocols are adhered to [22]. Our results suggest that trained caregivers can serve as vital partners in maintaining treatment success and minimizing complications when appropriately empowered.
Limitations
This was a single-center study with a relatively short follow-up period and was unable to assess long-term outcomes, such as delayed relapse, brace compliance, or functional scores. Caregiver satisfaction was not evaluated using a standardized tool, which led to further bias.
The addition of a sterile polythene sheet between successive layers of POP during Ponseti casting presents a simple, cost-effective, and practical modification that significantly enhances the ease and safety of cast removal in the treatment of idiopathic CTEV. This modification, which we propose to name the Gaur and Jadon technique, made cast removal quicker, easier, and less stressful for both caregivers and medical staff, all without affecting the treatment outcome. We were able to achieve good correction in nearly all cases, with very few complications and no need for specialized tools. This approach could be especially useful in busy or low-resource clinics where time, equipment, and trained personnel are often limited. While our early results are promising, further research with larger groups and longer follow-up will help us better understand the long-term benefits and whether this technique can become a standard part of Ponseti casting.
A polythene sheet interposed between plaster layers during Ponseti casting significantly simplifies cast removal in idiopathic clubfoot without affecting treatment outcomes.
References
- 1. Saini R, Sharma A, Ravalji D, Baisoya K, Sharma G. A prospective study on functional outcomes of serial cast correction in congenital talipes equinovarus (CTEV) by Ponseti method. Cureus 2023;15:e35987. [Google Scholar] [PubMed]
- 2. Castro AD, Peixoto JB, Miyahara LK, Akuri MC, Moriwaki TL, Sato VN, et al. Clubfoot: Congenital talipes equinovarus. Radiographics 2024;44:e230178. [Google Scholar] [PubMed]
- 3. Savio S, Maharjana M. Accelerated versus standard Ponseti method for idiopathic congenital talipes equinovarus: A systematic review and meta-analysis. Pediatr Traumatol Orthop Reconstr Surg 2021;8:473-84. [Google Scholar] [PubMed]
- 4. Ahmad MN, Ghani A, Singh R, Bhatt MF, Shabir SA, Nisar K, et al. Comparative study of accelerated Ponseti cast with standard Ponseti cast. J Med Sci Clin Res 2020;8:426-32. [Google Scholar] [PubMed]
- 5. Mohsenh WA, Alqarni MM, Alshehri AK, Asiri AM, Mohsenh OH, Mahmood SE, et al. Factors related to relapse of congenital talipes equinovarus (CTEV) after the Ponseti method. Cureus 2023;15:e43701. [Google Scholar] [PubMed]
- 6. Pavone V, Vescio A, Caldaci A, Culmone A, Sapienza M, Rabito M, et al. Sport ability during walking age in clubfoot-affected children after Ponseti method: A case-series study. Children (Basel) 2021;8:181. [Google Scholar] [PubMed]
- 7. Tabard-Fougère A, Bonnefoy-Mazure A, Dayer R, Vazquez O, De Coulon G. The importance of having a single, dedicated medical team to treat congenital talipes equinovarus using the Ponseti method: A retrospective analysis of treatment outcomes after 3 years of follow-up. J Pediatr Orthop 2024;44:e361-8. [Google Scholar] [PubMed]
- 8. Sodhai VM, Patwardhan SA, Shyam AK, Haphiz A, Sancheti P. Ponseti cast removal: Video technique. J Orthop Case Rep 2020;10:50-2. [Google Scholar] [PubMed]
- 9. Bozkurt C, Sarıkaya B, Sipahioğlu S, Altay MA, Çetin BV. Using the modified Ponseti method to treat complex clubfoot: Early results. Jt Dis Relat Surg 2021;32:170-6. [Google Scholar] [PubMed]
- 10. Monárrez R, Herzenberg JE, McClure PK. A novel technique to remove plaster Ponseti clubfoot casts: Surgical/technical tips. J Pediatr Orthop Soc North Am 2022;4:526. [Google Scholar] [PubMed]
- 11. Aroojis A, Pragadeeswaran V. ‘Return to the new normal’: Innovative solutions for safe Ponseti casting in clubfoot clinics during the COVID-19 pandemic. Indian J Orthop 2020;55:224-9. [Google Scholar] [PubMed]
- 12. Elseddik HM, Helal MM, Kholeif MM, Sherif MM. Modified Ponseti manipulation and casting technique for treatment of atypical clubfoot. Egypt Orthop J 2018;55(Suppl 1):123-7. [Google Scholar] [PubMed]
- 13. Al-Mohrej OA, Alshaalan FN, Alhussainan TS. Is the modified Ponseti method effective in treating atypical and complex clubfoot? A systematic review. Int Orthop 2021;45:2589-7. [Google Scholar] [PubMed]
- 14. Rangasamy K, Baburaj V, Gopinathan NR, Behera P, Sudesh P, Subramanian SR. Correction results of atypical clubfeet managed with modified Ponseti technique: A meta-analysis of 354 feet. J Clin Orthop Trauma 2022;31:101939. [Google Scholar] [PubMed]
- 15. Jain AK, Kohli N, Bansal N, Sahni G, Aggarwal HO, Mathur M. Evaluation of results of Ponseti technique in idiopathic clubfoot using clinical evaluation and radiological assessment. Int J Appl Basic Med Res 2022;12:43-6. [Google Scholar] [PubMed]
- 16. Islam MS, Masood QM, Bashir A, Shah FY, Halwai MA. Results of a standard versus an accelerated Ponseti protocol for clubfoot: A prospective randomized study. Clin Orthop Surg 2020;12:100-6. [Google Scholar] [PubMed]
- 17. Alam N, Abbas MB, Siddiqui YS, Julfiqar M, Abbas M, Khan MJ, et al. Effectiveness of Ponseti technique in management of arthrogrypotic clubfeet – a prospective study. Int J Burns Trauma 2023;13:33-43. [Google Scholar] [PubMed]
- 18. Maghfuri HB, Alshareef AA. The efficacy of the Ponseti method in the management of clubfoot: A systematic review. Cureus 2024;16:e52482. [Google Scholar] [PubMed]
- 19. Butt MN, Perveen W, Ciongradi CI, Alexe DI, Marryam M, Khalid L, et al. Outcomes of the Ponseti technique in different types of clubfoot-a single center retrospective analysis. Children (Basel) 2023;10:1340. [Google Scholar] [PubMed]
- 20. Zionts LE, Ebramzadeh E, Sangiorgio SN. Objective analysis of intermediate-term outcome of the Ponseti technique: A review of the experience from Los Angeles. Ann Transl Med 2021;9:1101. [Google Scholar] [PubMed]
- 21. Dibello D, Colin G, Galimberti AM, Torelli L, Di Carlo V. How to cope with the Ponseti method for clubfoot: The families’ standpoint. Children (Basel) 2022;9:1134. [Google Scholar] [PubMed]
- 22. Chen SN, Ragsdale TD, Rhodes LN, Locke LL, Moisan A, Kelly DM. Prospective, randomized Ponseti treatment for clubfoot: Orthopaedic surgeons versus physical therapists. J Pediatr Orthop 2023;43:e93-9. [Google Scholar] [PubMed]