To assess the functional outcome of proximal humerus fractures treated with hemiarthroplasty.
Dr. Mohamed Safiullah, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: dr.safiullahmbbsms@gmail.com
Introduction: Proximal humeral fractures (PHFs) represent a significant portion of fragility fractures in the elderly, ranking third after hip and distal radius fractures. While the majority of minimally displaced PHFs can be managed nonoperatively, displaced three- and four-part fractures often require surgical intervention. Hemiarthroplasty (HA) has traditionally been used for complex fracture patterns. With recent advances in prosthetic design and surgical techniques, HA continues to be a valuable option.
Case Series: This case series evaluated patients with PHFs. This study aims to assess the functional outcomes of three- or four-part proximal humerus fractures treated with HA using Constant and UCLA scores. In addition, it evaluates radiological parameters such as tuberosity position and union, tuberosity resorption, humeral head height, and signs of implant loosening or radiolucency at the bone-cement interface through serial shoulder radiographs.
Conclusion: HA provides reliable pain relief and functional recovery in elderly patients with complex proximal humerus fractures. It shows low complication rates and high patient satisfaction, though larger studies with long-term follow-up are needed for broader validation.
Keywords: Proximal humerus fracture, hemiarthroplasty, Neer classification, functional outcome, constant score, osteonecrosis.
Proximal humeral fractures (PHFs) represent up to 5% of all fractures and are particularly prevalent in the elderly, with approximately 76% of cases occurring in individuals over the age of 45. [1] Early clinical series, such as that of Zyto et al., demonstrated that complex three- and four-part fractures treated with hemiarthroplasty can achieve satisfactory pain relief and functional outcomes in selected patients. [2] While nearly 80% of PHFs are minimally displaced and managed conservatively, [3] displaced three- and four-part fractures, as defined by Neer’s classification, often require surgical intervention due to poor outcomes with nonoperative treatment. [4]
Open reduction and internal fixation (ORIF) is widely used but associated with high complication rates—such as screw cut-out, malunion, and osteonecrosis—particularly in complex fracture patterns. [5] In elderly patients with osteoporotic bone or head-splitting fracture patterns, hemiarthroplasty (HA) has emerged as a preferred option, providing predictable pain relief and functional improvement when reconstruction is not feasible. [6] Although HA shows variable functional outcomes, advances in prosthesis design and surgical technique have improved success rates. [2] Proper tuberosity positioning and humeral height restoration are key to better outcomes, as highlighted by Boileau et al. [7] Nevertheless, surgical treatment of PHFs in the elderly remains associated with non-negligible complication rates, as reported in recent series. [8] The rationale of this study is to address the increasing incidence of complex proximal humerus fractures among elderly patients in India and the limited data available on functional outcomes following hemiarthroplasty in this population. With Neer’s classification serving as the guiding framework for categorizing three- and four-part fractures, this study utilizes the system to standardize patient selection and outcome comparison. By assessing functional outcomes using Constant and UCLA scores alongside radiological parameters such as tuberosity position, union, and implant stability, this study aims to evaluate the efficacy of hemiarthroplasty and contribute localized evidence to guide treatment protocols for proximal humeral fractures.
This study was designed to assess the functional outcome of proximal humerus fractures treated with hemiarthroplasty. It was a prospective observational study that included 30 patients diagnosed with three- and four-part proximal humerus fractures at Sree Balaji Medical College and Hospital (SBMCH). Each patient was clinically examined on admission, evaluated radiologically using X-rays and CT scans, and optimized preoperatively with relevant blood investigations. After obtaining informed consent, surgery was performed following standard hemiarthroplasty protocols, and postoperative rehabilitation began the next day with passive range of motion exercises.
Patients were followed up at regular intervals—2 weeks, 6 weeks, 3 months, 6 months, and 1 year—to monitor pain, range of motion, and radiographic healing. Functional outcomes were assessed using the Constant-Murley and UCLA shoulder scores, and radiological assessment included tuberosity position, union, and implant stability.
The study was conducted in the Orthopaedics OPD and Casualty department. The study period extended from December 2022 to April 2025, with recruitment between December 2022 and March 2024 to ensure a minimum follow-up of one year. The sample size of 30 patients was calculated using the statistical formula for estimation of mean with a 95% confidence interval (Z = 1.96), estimated pooled standard deviation (σ), and 10% margin of error (E), ensuring adequate power to detect meaningful clinical differences in functional outcomes.
Rationale of the study: The study was conducted to address the growing number of proximal humeral fractures among elderly Indian patients and to evaluate the functional and radiological outcomes of hemiarthroplasty, which remains a preferred surgical treatment when osteoporotic bone and comminuted fractures preclude internal fixation. This research fills the gap in localized outcome data and aims to optimize treatment strategies suited to the Indian demographic.
Use of Neer’s Classification: Neer’s classification was used to categorize patients into three- and four-part fracture groups. This system provided a standardized approach for selecting cases for hemiarthroplasty and for consistent comparison of postoperative outcomes. By basing patient inclusion and analysis on this classification, the study ensured uniformity in assessing fracture complexity and surgical indications.[5]
The patient selection criteria are as follows: Inclusion criteria includes Age more than 45 years, Neer’s classification 3-part and 4-part fractures with intact rotator cuff, fracture dislocation, and closed fractures. Exclusion criteria include associated glenoid fractures, associated humeral shaft fractures, compound fractures, and medical comorbid patients unfit for surgery.
Investigations: Each patient underwent detailed imaging studies to confirm fracture classification and plan the surgical approach. Standard X-rays of the shoulder—including anteroposterior, axillary, and scapular Y-views—were obtained for all cases to assess displacement, angulation, and involvement of tuberosities. Computed tomography (CT) scans with 3D reconstruction were performed for selected patients to delineate fracture geometry, comminution, and the extent of articular surface involvement, which guided the surgical planning and selection of prosthesis size and position.
Informed consent was obtained from all participants. Demographic details and relevant medical history were collected using a structured proforma. Clinical examination and surgical intervention were carried out using standard procedures at the SBMCH. [Fig. 1] [Fig. 2] [Fig. 3] Postoperative evaluation for implant loosening was done through serial radiographs, specifically assessing for radiolucency at the bone-cement interface. Functional outcomes were assessed 26 using the CONSTANT-Murley score and UCLA shoulder score. All data were entered in Microsoft Word and analyzed using SPSS software version 24. [Fig. 4].

Figure 1: Pre-operation X-ray.

Figure 2: C-ARM image.
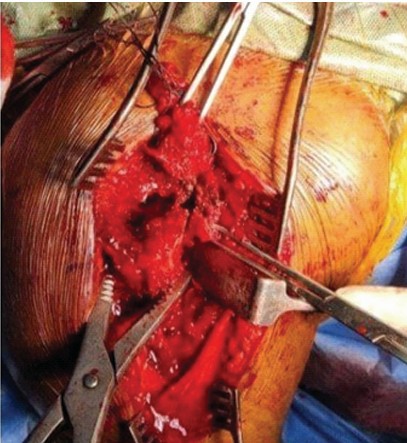
Figure 3: Inter-operation image.

Figure 4: Post-operative X-ray.
Post-operative outcomes were promising:
- 60% of patients reported no pain
- 3% had only occasional mild pain
- Only 7% experienced activity-related discomfort, with no patients requiring potent analgesics.
These results affirm the role of HA in achieving effective pain relief and restoring functional movement (Fig. 5)

Figure 5: Post-operative 1-year follow-up clinical image.
Functional evaluation using the Constant-Murley Score showed:
- 60% of patients had excellent outcomes
- 3% had good outcomes
- While only 7% had fair or poor results.
These findings align with previous research by Boileau et al. and Zyto et al., confirming the viability of HA in managing complex PHFs, particularly in elderly patients with osteoporotic bone. While ORIF remains a consideration in younger patients with reconstructable fractures, HA is preferred when there is significant comminution, poor bone quality, or when vascularity of the humeral head is compromised. Indications for HA include displaced three- or four-part fractures, head-splitting fractures, failed ORIF, and fracture-dislocations – as outlined in Neer’s guidelines. Our findings support HA as a safe and effective treatment for complex PHFs, offering predictable pain relief and functional restoration.
Our findings demonstrated that displaced three- and four-part fractures often necessitate surgical intervention. In such cases, hemiarthroplasty (HA) is a widely accepted treatment modality, especially in elderly patients with poor bone quality, complex fracture patterns, or signs of humeral head ischemia. In this study, we evaluated 30 patients who underwent primary HA for three- or four-part PHFs. The age distribution revealed that 76.7% of patients were between 55 and 74 years, aligning with global trends that associate increased PHF incidence with advancing age. The right shoulder was more commonly involved (63.3%), likely due to its dominance in most individuals, consistent with contemporary epidemiology [1].According to Neer’s classification, 53.3% had three-part and 46.7% had four-part fractures, both associated with high risk for complications if managed non-operatively. These indications justified the use of HA as the primary intervention.Tuberosity fixation is known to be a key determinant of postoperative shoulder function. In our cohort, 73.3% underwent fixation with Prolene sutures, favored for their tensile strength and biocompatibility. As supported by previous studies, stable tuberosity fixation enables better rotator cuff function and range of motion. Interestingly, our analysis found no statistically significant difference in outcomes with respect to age, gender, comorbidities, side of injury, fracture classification, or active forward flexion. This is in line with studies by Mighell, Demirhan, and others, though some literature suggests poorer outcomes in older women due to tuberosity resorption or migration. The importance of postoperative rehabilitation was also highlighted. Patients who adhered to rehabilitation protocols demonstrated better outcomes, underscoring the role of socioeconomic and motivational factors in recovery. This study is limited by its small sample size and single-center design, which may affect the generalizability of results. The short-term follow-up may not capture long-term complications like implant loosening or tuberosity resorption. The lack of a control group prevents comparison with other treatments, such as reverse shoulder arthroplasty. Functional scores used included subjective elements, and radiological evaluation was limited to plain X-rays. Additionally, selection bias may exist, as only patients suitable for hemiarthroplasty were included.
Postoperative outcomes were promising:
· 60% of patients reported no pain,
· 23.3% had only occasional mild pain, and
· only 16.7% experienced activity-related discomfort, with no patients requiring potent analgesics.
These results affirm the role of HA in achieving effective pain relief and restoring functional movement. [Fig. 5]
Functional evaluation using the Constant-Murley Score showed:
· 60% of patients had excellent outcomes,
· 23.3% had good outcomes,
· While only 16.7% had fair or poor results.
These findings align with previous research by Zyto et al. [2] and Boileau et al. [7], confirming the viability of HA in managing complex PHFs, particularly in elderly patients with osteoporotic bone. While ORIF remains a consideration in younger patients with reconstructable fractures, HA is preferred when there is significant comminution, poor bone quality, or when vascularity of the humeral head is compromised.[5] Indications for HA include displaced three- or four-part fractures, head-splitting fractures, failed ORIF, and fracture-dislocations—as outlined in contemporary reviews.[9] Recent epidemiologic data by Launonen et al. further emphasize the increasing incidence of proximal humerus fractures in aging populations. [10] Our findings support HA as a safe and effective treatment for complex PHFs, offering predictable pain relief and functional restoration .
An effective therapeutic option for complicated PHF is HA. Excellent pain relief and a moderate return to function are observed in elderly patients with minor issues. The procedure demonstrated a low complication rate and high patient satisfaction, aligning well with international outcome benchmarks. Nevertheless, a larger patient sample with long-term follow-up is required before the findings can be applied to the general population.
The effective treatment plan for a complicated proximal humerus fracture is hemiarthroplasty.
References
- 1. Lind T, Kroner K, Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg 1989; 108–5:285–287 [Google Scholar] [PubMed]
- 2. Zyto K, Wallace WA, Frostick SP, Preston BJ. Outcome after hemiarthroplasty for three- and four-part fractures of the proximal humerus. J Shoulder Elbow Surg 1998;7:85–9. [Google Scholar] [PubMed]
- 3. Iannotti JP, Ramsey ML, Williams GR Jr, Warner JJ. Nonprosthetic management of proximal humeral fractures. Instr Course Lect 2004;53:403–416 [Google Scholar] [PubMed]
- 4. Kontakis G, Koutras C, Tosounidis T, Giannoudis P. Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br 2008;90:1407–1413 [Google Scholar] [PubMed]
- 5. Maier D, Jaeger M, Izadpanah K, Strohm PC, Südkamp NP. Proximal humeral fracture treatment in adults. J Bone Joint Surg Am 2014; 96(3):251–261. [Google Scholar] [PubMed]
- 6. Puzzitiello RN, Zmistowski B, Lenarz CJ, Sholder D, Abboud JA. Management of proximal humerus fractures in the elderly: state of the art. J Orthop Trauma 2018;32(8):e416–e423. [Google Scholar] [PubMed]
- 7. Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Molé D. Tuberosity healing after hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg 2018;27(5):856–867. [Google Scholar] [PubMed]
- 8. Klug A, Wincheringer D, Harth J, Schmidt-Horlohe K, Hoffmann R, Gramlich Y. Complications after surgical treatment of proximal humerus fractures in the elderly. J Shoulder Elbow Surg 2019;28:1674–1684 [Google Scholar] [PubMed]
- 9. Garrigues GE, Zmistowski B, Zettl R, Boileau P. Shoulder arthroplasty for proximal humerus fracture. J Shoulder Elbow Surg 2019;28(10):1878–1889. [Google Scholar] [PubMed]
- 10. Launonen AP, Lepola V, Flinkkilä T, Laitinen M, Paavola M. Epidemiology of proximal humerus fractures. Acta Orthop 2019;90(5):421–425. [Google Scholar] [PubMed]








