Bilateral joint arthroplasty is a practical treatment approach for young patients with severe rheumatoid arthritis and intricate deformities. Prioritizing early planning, fostering multidisciplinary care, and incorporating robotic assistance can greatly enhance surgical accuracy, safety, and functional recovery in these high-risk situations.
Dr. Gaurav Gupta, Department of Orthopaedics, Max Superspeciality Hospital, Dehradun, Uttarakhand, India. E-mail: drgauravorthosurgeon@gmail.com
Introduction: Rheumatoid arthritis (RA) is a chronic autoimmune condition that frequently results in serious joint deformities, reduced function, and systemic issues. Complicated deformities in major joints such as the hips and knees create considerable management difficulties, particularly when aggravated by osteoporosis and anemia.
Case Report: We report a 39-year-old woman with a 15-year history of RA who has severe bilateral deformities in her hips and knees. She could not ambulate independently due to advanced joint destruction, chronic flexion contractures, and functional disability. Pre-operative imaging confirmed end-stage arthropathy, and laboratory workup showed severe anemia and osteoporosis. A multidisciplinary approach led to successful staged bilateral total hip and knee arthroplasty, including robotic-assisted left hip replacement. Post-operative recovery was uneventful, enabling the patient to ambulate independently and restore joint mobility pain-free.
Conclusion: This case demonstrates the success of a staged, multidisciplinary strategy for addressing intricate bilateral joint deformities resulting from RA. The use of robotic assistance along with thorough perioperative planning can enhance surgical precision and support functional recovery, even for high-risk patients.
Keywords: Rheumatoid arthritis, total joint arthroplasty, flexion deformity, bilateral hip and knee replacement, osteoporosis, robotic hip replacement, staged surgery, functional recovery.
Rheumatoid arthritis (RA) is a systemic autoimmune disorder predominantly affecting the joints, presenting a range of clinical manifestations. Pain and stiffness frequently increase after periods of inactivity. The wrists and hands are most commonly affected, typically on both sides of the body. The condition can also influence other body areas, potentially causing a low red blood cell count, lung inflammation, and heart inflammation. Its progression is marked by joint inflammation, pain, and stiffness, potentially impacting multiple organ systems. Symptoms such as fever and low energy may also occur and usually develop gradually over weeks or months.
Recognizing these clinical manifestations is essential for prompt diagnosis and the application of effective management strategies [1,2,3].
The primary characteristic of RA is synovitis, the synovial membrane inflammation surrounding the joints. This inflammation typically affects the joints symmetrically on both sides of the body. The small joints in the hands and feet are frequently involved, but larger joints, such as the knees, shoulders, and hips, can also be affected. The inflamed synovium leads to symptoms such as swelling, warmth, and tenderness in the joints, which subsequently cause pain and restrict the range of motion. A notable symptom is morning stiffness, which often endures for over 30 min, making it a significant indicator of RA. If left untreated, chronic inflammation of the synovium can result in joint damage, leading to deformities and a reduction in function. This damaging process can be assessed using imaging techniques, such as X-rays and magnetic resonance imaging, which may reveal erosions, narrowing of the joint space, and periarticular osteopenia [4,5].
RA primarily targets the joints but can also present extra-articular symptoms across organ systems, indicating the disease’s systemic nature. These manifestations include rheumatoid nodules, cardiovascular complications, pulmonary issues, ocular conditions, hematologic deviations, and neurological problems. Rheumatoid nodules, typically painless, often form over bony prominences and can signal more aggressive disease. Patients face a higher risk of cardiovascular issues such as atherosclerosis and myocardial infarction, increasing their cardiovascular mortality risk due to the disease’s impact on cardiac structures [6,7].
Conditions include atherosclerosis, arterial stiffness, coronary arteritis, congestive heart failure, valvular disease, and fibrinous pericarditis. Prognostic indicators may consist of dyslipidemia and hypertension. Common pulmonary consequences involve pleural effusions, pulmonary fibrosis, interstitial lung disease, and arteritis, especially in smokers, who are at risk of severe complications. RA also affects eye health, leading to scleritis, keratitis, and dry eye syndrome. Neurological issues may result in peripheral neuropathy and cervical myelopathy, while renal symptoms like glomerulonephritis are rare and linked to vasculitis [8].
The onset of disease is not similar in all patients but varies regarding type, number, and the pattern of joint involvement. The course of disease may also differ according to the presence or absence of several variables, including genetic background, frequency of swollen joints, autoantibodies in the serum, and the severity of the inflammatory process [9]. The causes of RA remain unclear, but it is thought to stem from an improper immune response. RA can onset at any age and leads to fatigue and extended stiffness following rest periods. While there is no cure for RA, a growing number of effective medications are available to manage the condition and prevent joint deformities. Alongside drugs and surgery, scientifically backed self-management strategies – techniques people employ daily to handle their condition and engage in meaningful activities – such as exercise, can alleviate pain and reduce disability. Stages of RA: Early identification and treatment to manage inflammation are crucial due to the risk of rapid joint degradation and damage to other tissues’ functioning [10]. This case report outlines the clinical, radiological, and surgical management of a severely disabled RA patient and complies with CARE case report guidelines.
A 39-year-old woman came in OPD in June 2024, reporting a 15-year history of severe joint pain and deformities in her hips and knees. She was unable to stand or walk independently. Her medical history includes RA undergoing treatment with disease-modifying antirheumatic drugs and corticosteroids. The family’s medical history provided no further insights. Her functional status was significantly compromised.
Clinical Findings: Examination revealed a V-shaped spinal posture, fixed flexion deformities in both knees (right: 50°, left: 90°), bilateral hip flexion, and external rotation contractures. She required assistance to stand (Fig. 1).

Figure 1: Clinical photograph showing severe bilateral lower limb deformity preoperatively.
Diagnostic assessment
Radiographs of the hips and knees showed significant joint damage, evident through reduced joint space and deformities. The X-rays for the right and left knee revealed total joint space loss and periarticular osteopenia (Fig. 2).
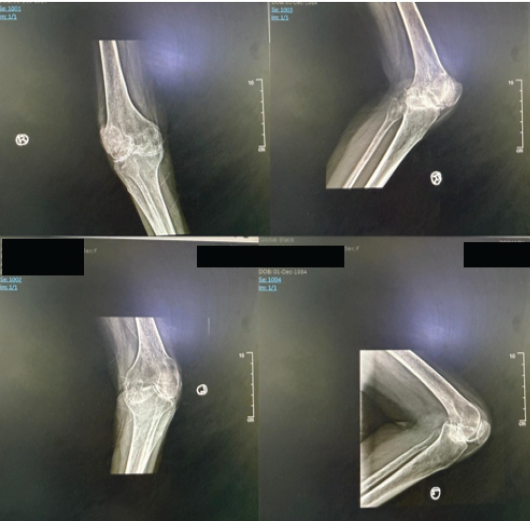
Figure 2: Pre-operative anteroposterior and lateral X-ray of the right knee and left knee (June 25, 2024).
A 3D reconstructed computed tomography scan of the pelvis highlighted bilateral acetabular and proximal femoral deformities (Fig. 3). Laboratory tests indicated severe anemia (Hb = 6.7 g/dL), which was effectively treated through transfusions. Bone mineral density scans confirmed the existence of severe osteoporosis. The diagnosis of end-stage joint involvement from RA remains confirmed.
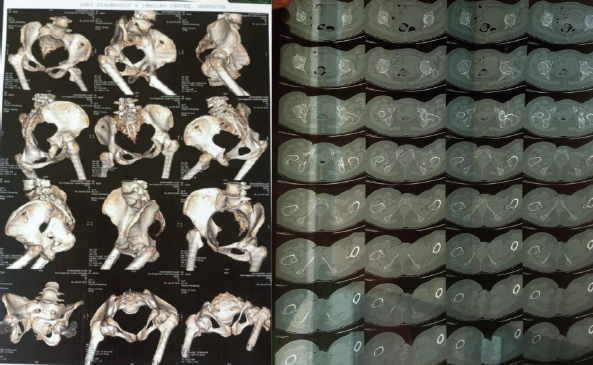
Figure 3: Pre-operative 3D computed tomography scan of the pelvis showing bilateral hip deformities (June 2024).
Therapeutic intervention
A multidisciplinary team created a staged surgical strategy:
- June 21, 2024: Right uncemented total hip arthroplasty (THA)
- June 26, 2024: Right total knee replacement (Fig. 4)

Figure 4: Post-operative X-ray showing right total knee replacement (June 27, 2024, and August 20, 2024).
- August 21, 2024: Left total knee replacement (Fig. 5)
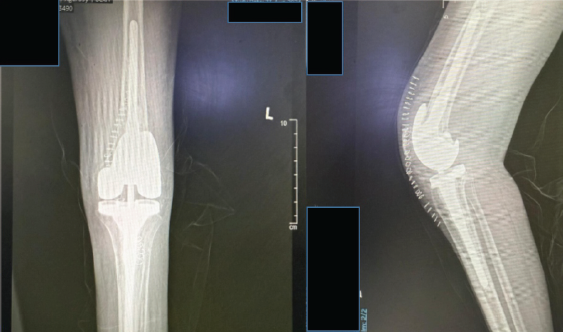
Figure 5: Post-operative X-ray showing the left total knee replacement (August 23, 2024).
- September 6, 2024: Robotic-assisted uncemented left THA.
A post-operative image after both hip replacements displays well-aligned bilateral prostheses with no evidence of loosening or malposition (Fig. 6). Perioperative care included addressing anemia, administering calcium and Vitamin D supplements, implementing thromboprophylaxis, and starting early rehabilitation.
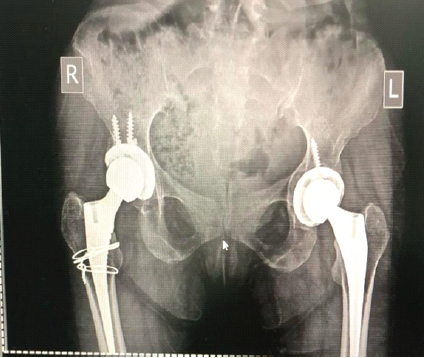
Figure 6: Post-operative X-ray showing both hips with well-positioned prostheses (January 14, 2025).
Follow-up and outcomes
All surgeries were successful without intraoperative or immediate post-operative complications. The patient fully regained motion in all affected joints. By October 2024, she could walk pain-free independently and resumed her daily activities, enjoying a markedly improved quality of life.
This case illustrates the challenges and positive results of complex bilateral total joint replacements in patients with severe deformities resulting from RA. The patient reached significant functional recovery through a systematic approach involving medical optimization, careful surgical planning, and rehabilitation. Post-operative imaging confirmed optimal alignment of the implanted limb preservation prosthesis system, with maintained limb length equality. The patient was initiated on partial weight-bearing ambulation with walker assistance from post-operative day 3. A structured physiotherapy regimen focused on joint mobility and muscle strengthening. Within a few days, the patient demonstrated stable knee function and achieved pain-free, independent ambulation. Robotic hip replacement allowed for accurate implant placement, even with the altered anatomy. This case underscores the advantages of proactive surgical intervention for younger RA patients facing end-stage joint disease. Cao et al. (2023) studied 30 RA patients who underwent bilateral cementless THA and cemented posterior-stabilized total knee arthroplasty (PS-TKA). After surgery, all patients regained mobility, with average satisfaction scores of 92.5 for THA and 89.6 for TKA. Only one patient needed revision due to knee instability, and radiographs showed stable implants with a 99.2% survivorship at 84 months [11]. Karunaratne et al. (2019) explained that robotic-assisted TKA uses pre-operative imaging or intraoperative bone mapping to develop a patient-specific 3D knee model, allowing precise bone cuts and implant placement. Intraoperative optical tracking helps assess ligament balance and soft tissue management, improving implant alignment and stability [12]. Similarly, Ma et al. (2023) compared robot-assisted THA (R-THA) with manual THA in 95 matched patients with osteonecrosis of the femoral head. The R-THA group had significantly higher Forgotten Joint Scores (P = 0.01) at 6 months, indicating better early functional recovery without increased surgical invasiveness [13]. Supporting these results, Song et al. (2011) performed a within-patient comparison of robotic-assisted and traditional TKA in 30 patients who had bilateral procedures. The robotic side showed fewer alignment outliers in the mechanical axis and component orientation, as well as less post-operative bleeding. Although the robotic procedures took longer, clinical scores and range of motion were slightly better on that side [14]. Overall, these studies highlight that robotic-assisted arthroplasty improves implant placement accuracy and early recovery without increasing invasiveness, representing an important step forward in treating complex RA and joint degeneration.
Patient perspective
The patient expressed satisfaction with the surgical outcomes and reported significant pain relief and restoration of independence. This patient is at a high risk of periprosthetic fractures in the future. For this patient and other high-risk elderly individuals with periprosthetic fractures, the long-term strategy involves a structured rehabilitation program designed to restore joint function while reducing the risk of falls. Consistent follow-ups with radiographic evaluations are vital to track the integrity of the prosthesis and the healing of the fracture. Future care must prioritize personalized physiotherapy, nutritional enhancements (particularly calcium and vitamin D), and management of osteoporosis. It is crucial to implement home safety modifications and fall-prevention initiatives.
This case highlights the significant potential of a systematic, multidisciplinary approach to restoring function and mobility in patients with end-stage RA complicated by severe lower-limb deformities. By following a carefully planned staged sequence of bilateral total hip and knee replacements, the patient achieved complete correction of contractures, realignment of anatomy, and regained independent walking ability. Essential pre-operative preparations – including correcting anemia and managing osteoporosis – coupled with early mobilization and structured physiotherapy – were crucial for optimal recovery. The use of robotic-assisted uncemented THA played a key role in overcoming complex anatomical challenges, ensuring precise implant placement, balanced limb alignment, and improved prosthesis durability, thus highlighting the benefits of robotic precision in advanced joint replacement procedures.
Early detection and sequential surgical planning are crucial in managing advanced joint deformities caused by rheumatoid arthritis. This case illustrates that it is possible to restore functional independence, even amid severe flexion deformities, osteoporosis, and anemia, by utilizing multidisciplinary optimization and cutting-edge joint replacement methods. Robotic-assisted hip arthroplasty improves precision in altered anatomical structures. A systematic, patient-focused strategy guarantees safety while enhancing outcomes. This report demonstrates the practicality of complex staged arthroplasty for younger patients with RA, providing them with better mobility and an improved quality of life.
References
- 1. Wasserman AM. Diagnosis and management of rheumatoid arthritis. American family physician. 2011;84(11):1245-52. PMID: 22150658 [Google Scholar] [PubMed]
- 2. Aletaha D, Smolen JS. Diagnosis and management of rheumatoid arthritis: a review. Jama. 2018;320(13):1360-72. doi: 10.1001/jama.2018.13103. [Google Scholar] [PubMed] [CrossRef]
- 3. Salaffi F, Gutierrez M, Carotti M. Ultrasound versus conventional radiography in the assessment of bone erosions in rheumatoid arthritis. Clin Exp Rheumatol. 2014;32(1 Suppl 80):S85-90. PMID: 24528649. [Google Scholar] [PubMed]
- 4. Baghdadi LR, Woodman RJ, Shanahan EM, Mangoni AA. The impact of traditional cardiovascular risk factors on cardiovascular outcomes in patients with rheumatoid arthritis: a systematic review and meta-analysis. PLOS ONE. 2015;10(2):e0117952. 10.1371/journal.pone.0117952 [Google Scholar] [PubMed] [CrossRef]
- 5. Chen Y, Xu W, Yang H, Shao M, Xu S, Deng J, Gao X, Liu H, Shuai Z, Xu S, Pan F. Serum levels of hepcidin in rheumatoid arthritis and its correlation with disease activity and anaemia: a meta-analysis. Immunological investigations. 2021;50(2-3):243-58. 10.1080/08820139.2020.1742731 [Google Scholar] [PubMed] [CrossRef]
- 6. Haddani F, Guich A, Youssoufi T, Boudhar E, Abouqal R, Achemlal L, Allali F, Bahiri R, Bouchti E, Maghraoui E, Ghozlani I. Comorbidities in rheumatoid arthritis: The RBSMR study. Int. J. Clin. Rheumtol. 2020;15:1-0. [Google Scholar] [PubMed]
- 7. Singh JA, Christensen R, Wells GA, Suarez-Almazor ME, Buchbinder R, Lopez-Olivo MA, Ghogomu ET, Tugwell P. A network meta-analysis of randomized controlled trials of biologics for rheumatoid arthritis: a Cochrane overview. Cmaj. 2009;181(11):787-96. 10.1503/cmaj.091391 [Google Scholar] [PubMed] [CrossRef]
- 8. El Miedany Y, Youssef S, Mehanna AN, El Gaafary M. Development of a scoring system for assessment of outcome of early undifferentiated inflammatory synovitis. Joint Bone Spine. 2008; 75:155–62. 10.1016/j.jbspin.2007.04.021 [Google Scholar] [PubMed] [CrossRef]
- 9. Gossec L, Combescure C, Rincheval N, Saraux A, Combe B, Dougados M. Relative Clinical Influence of Clinical, Laboratory, and Radiological Investigations in Early Arthritis on the Diagnosis of Rheumatoid Arthritis. Data from the French Early Arthritis Cohort ESPOIR. J Rheumatol. 2010; 37:2486–92. 10.3899/jrheum.100267 [Google Scholar] [PubMed] [CrossRef]
- 10. Jahid M, Khan KU, Rehan-Ul-Haq, Ahmed RS. Overview of Rheumatoid Arthritis and Scientific Understanding of the Disease. Mediterr J Rheumatol. 2023 Aug 1;34(3):284-291. 10.31138/mjr.20230801.oo [Google Scholar] [PubMed] [CrossRef]
- 11. Cao J, Wang W, Feng W, Xu H, Wang D, Zhou Z. Staged replacement of both hips and both knees in patients with rheumatoid ar thritis. BMC Musculoskelet Disord 2023;24:231. [Google Scholar] [PubMed]
- 12. Karunaratne S, Duan M, Pappas E, Fritsch B, Boyle R, Gupta S, et al. The effectiveness of robotic hip and knee arthroplasty on patient-reported outcomes: A systematic review and meta-analysis. Int Orthop 2019;43:1283-95. [Google Scholar] [PubMed]
- 13. Ma M, Cao Z, Yang M, Kong X, Chai W. The invasiveness of robot-assisted total hip replacement is similar to that of conventional surgery. J Robot Surg 2023;17:2987-93. [Google Scholar] [PubMed]
- 14. Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: A prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2011;19:1069-76. [Google Scholar] [PubMed]