This case highlights the importance of incorporating biomechanical risk assessment into the preoperative planning of sacral tumor resections. Even when oncologic margins are successfully achieved and bone fragility risk factors are absent, resection involving the sacral ala or posterior pelvic ring may lead to late-onset pelvic insufficiency fractures. Prophylactic stabilization should be considered in selected patients to prevent structural failure, improve long-term functional outcomes, and reduce the need for reoperations.
Dr. Joaquín Zuniga-Soria, Universidad del Desarrollo – Clínica Alemana de Santiago, Vitacura, Chile. E-mail: jzunigasoria.med@gmail.com
Introduction: Sacral chondrosarcoma is a primary malignant bone tumor for which en bloc resection remains the standard treatment. Given its location and role within the pelvic ring continuity, it poses a surgical and reconstructive challenge. Even with successful oncologic resection, the lack of a comprehensive preoperative biomechanical analysis may contribute to late-onset complications requiring reinterventions and impair the patient’s quality of life.
Case Report: The case describes a 41-year-old woman with no previous diagnosis of osteoporosis or prior fractures who underwent en bloc resection of a sacral chondrosarcoma at the S1-S2 level, without initial complications. Six months post-operatively, the patient returned with pain and gait impairment. An insufficiency fracture at the S1 vertebral body and residual sacral wing was identified, without signs of tumor recurrence or associated fluid collection. It was managed with posterior lumbopelvic fixation, with a favorable outcome and recovery in a 5-year follow-up.
Conclusion: This case underlines the importance of the biomechanical integrity of the pelvic ring. It raises the need for assessment of the biomechanical risk within the oncologic surgical planning, despite the absence of classical bone fragility factors. Thus, structural destabilization of the pelvis must consider corrective or preventive strategies to prevent complications. A comprehensive analysis of these factors allows for improved functionality and patients quality of life.
Keywords: Sacral chondrosarcoma, pelvic insufficiency fracture, lumbopelvic fixation, pelvic ring instability.
Sacral chondrosarcoma is the second most common primary malignant bone tumor, accounting for approximately 25% of these tumors. It is characterized by the production of a cartilaginous matrix and a locally aggressive behavior [1]. Due to its relationship with critical neurovascular components and the anatomical limitations of the pelvis itself, the sacral chondrosarcoma poses a surgical challenge [2,3]. Given tumoral resistance to chemotherapy and radiotherapy, standard treatment consists of en bloc surgical resection with wide oncologic margins [4,5].
Intraoperative image-guided navigation has allowed for more precise osteotomies and enhances the likelihood of tumor-free margins [6,7]. However, resections in the sacrum or its supporting structures result in wider osseous defects, leading to pelvic ring instability, particularly when the sacral ala or the sacroiliac joint are compromised [8].
In patients with bone fragility risk factors – such as history of insufficiency fractures, Vitamin D deficiency, autoimmune diseases, or immunosuppressive treatments – structural impairment may result in pelvic insufficiency fractures, an often overlooked but potentially preventable complication [9,10]. Despite surgical oncologic success, neglecting a proper biomechanical analysis during preoperative planning may result in late-onset functional destabilization, persistent pain, and reoperations.
The present case describes a patient who underwent en bloc resection of a sacral chondrosarcoma with image-guided navigation and developed a pelvic insufficiency fracture as a late-onset complication. The aim of this report is to perform a causal analysis of the complication and therapeutic approach, comparing it with existing evidence.
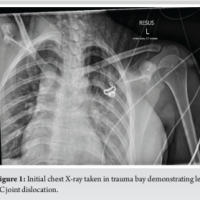
A 41-year-old female, with a history post-COVID immune dysfunction characterized by polyarthralgia, underwent a single photon emission computed tomography (SPECT-CT) scan, which revealed intense focal uptake in the left sacrum (Fig. 1), prompting the request for imaging studies with greater specificity.
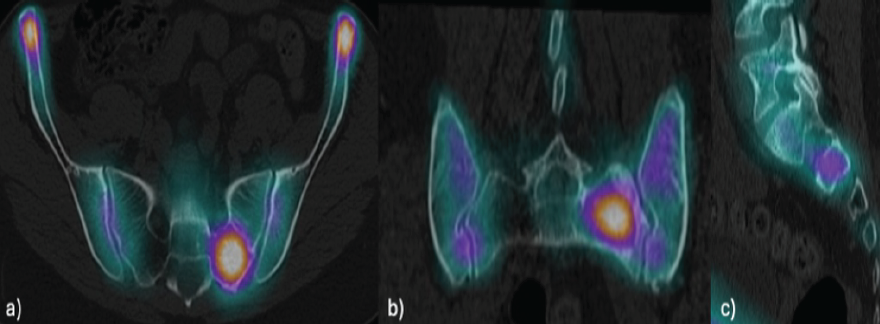
Figure 1: Single photon emission computed tomography revealing intense focal uptake in the left sacrum, adjacent to S1 foramen in axial (a), coronal (b), and sagittal (c) views.
The computed tomography (CT) identified a lytic and eccentric lesion of chondroid characteristics, with well-defined borders and a locally aggressive behavior, located within the left sacrum in the S1-S2 interforaminal region, measuring 39 × 30 × 23 mm. The lesion had a partial extension to the left sacral body and a small focus of cortical disruption in the anterior aspect of the S2 foramen (Fig. 2).
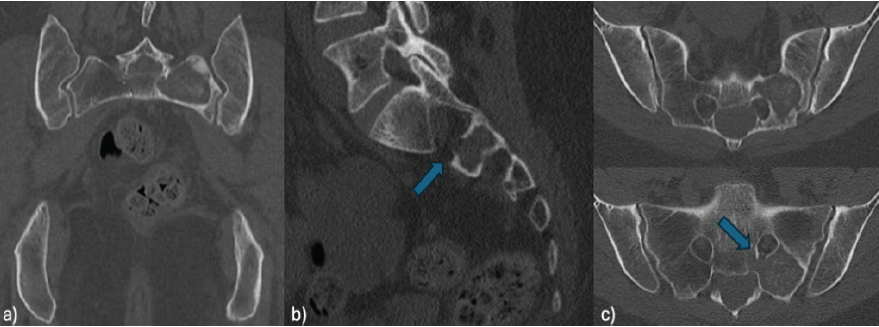
Figure 2: Pelvic computed tomography scan in axial (a), coronal (b), and sagittal (c) views. Lytic lesion in the left sacrum with cortical disruption in the anterior aspect of the S2 foramen (arrow).
Magnetic resonance imaging (MRI) demonstrated a predominantly T2 hyperintense (Fig. 3) and T1 hypointense lesion with calcifications and progressive enhancement in delayed phases. The image showed no signs of diffusion restriction or sacroiliac infiltration.
Figure 3: Magnetic resonance imaging coronal view: Hypointense lesion on T1 (a), hyperintense on short tau inversion recovery (b), and contrast enhancement on gadolinium-enhanced T1(c).
Considering a suspected primary tumor, a percutaneous bone biopsy was performed, which confirmed the diagnosis of grade 2 chondrosarcoma. Given the tumor radio-chemoresistance, en bloc resection with wide oncologic margins was indicated. Integrated CT-scan and MRI images were used preoperatively with Spine Guidance Software from Stryker to define safe resection trajectories preserving left S1 and S2 nerve roots. Superselective embolization was performed on the lateral sacral, iliolumbar, and left L4-L5 segmental arterial branches, achieving tumor devascularization.
For tumor resection, a posterior left paramedian approach extending to the iliac crest was performed under intraoperative CT-guided navigation, with reference in the right posterior-inferior iliac spine (0, 3 mm accuracy).
A sacral laminectomy with nerve root preservation was performed. Osteotomies were executed using high-speed drills, ultrasonic scalpel, and chisels, achieving en bloc resection with clear oncologic margins. Preservation of S1 and S2 nerve roots was achieved. An incidental durotomy occurred in relation to a Tarlov cyst, which was repaired. The intraoperative bleeding was 2000 mL. During surgery, the patient required 3 red blood cells units and transient vasoactive agents.
Immediate post-operative care was provided in the intermediate care unit with a stable clinical course and no need of mechanical ventilation. No neurologic, infectious, or cardiovascular complications were presented in the early stages. Progressive rehabilitation was initiated on post-operative day two with good tolerance, achieving assisted functional gait by day 7. On post-operative day 9, the patient was discharged in stable condition with scheduled outpatient oncologic follow-up, pain management, and functional rehabilitation.
Six months post-operatively, the patient presented with progressive lumbosacral pain and gait impairment. The CT scan identified an insufficiency fracture in the vertebral body of S1 and the remnant of the left sacral ala (Fig. 4), without evident tumor recurrence or associated fluid collections.
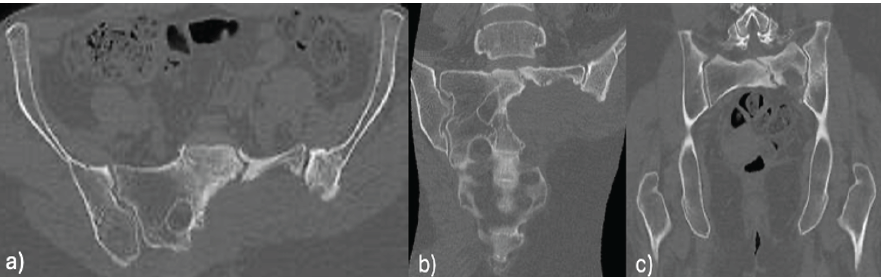
Figure 4: 6-month post-operative pelvic computed tomography scan: Insufficiency fracture on the left sacral ala.
The fracture was managed with percutaneous posterior lumbopelvic fixation. Robust stabilization was achieved by employing unilateral pedicle screw instrumentation from L5 to the iliac bone, reinforced with interiliac fixation (Fig. 5). The procedure was performed without complications.
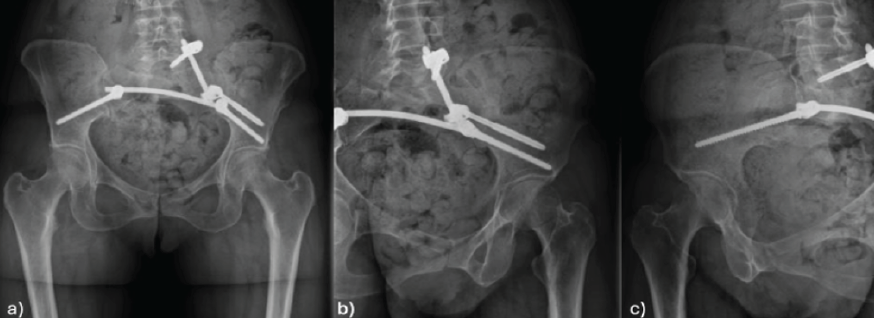
Figure 5: Post-operative pelvic X-rays: Anteroposterior (a), left sacral ala (b), and right sacral ala (c) view.
Five-years post-operatively, the patient maintains an adequate clinical follow-up without pain or functional deterioration. Imaging follow-up indicates stability of the lumbopelvic osteosynthesis, without relevant structural complications. SPECT-CT shows no signs of tumor recurrence (Fig. 6).
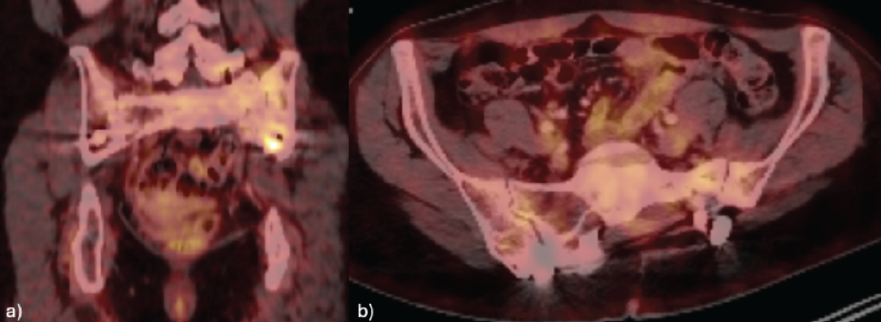
Figure 6: Single photon emission computed tomography at 5-year follow-up after tumor resection: No evidence of local recurrence on coronal (a) and axial (b) pelvic views.
Chondrosarcoma is a cartilaginous-origin primary malignant bone tumor, characterized by locally aggressive behavior and radio-chemoresistance. Thus, en bloc surgical resection with wide oncologic margins remains the standard treatment, especially in anatomically complex regions, such as the sacrum, in which proximity with neurovascular structures poses a challenge in achieving adequate local control [1].
New technologies, such as intraoperative CT-guided navigation and 3D reconstructions for pre-operative planning have significantly improved surgical accuracy with tumor-free margins during resections, particularly in topographically constrained regions. Nevertheless, it should be complemented by proper pre-operative planning, considering not only oncologic outcome, but also post-resection structural integrity. When en bloc resection involves the acetabulum or sacral ala, disruption of posterior pelvic ring continuity poses a significant risk for pelvic destabilization, particularly in patients with previous risk factors [6, 10-14].
Sacral ala and sacroiliac joint have a crucial role in mechanical load transmission between the torso and the lower limbs; therefore, its resection significantly compromises pelvic biomechanical functions. This alteration may manifest as pelvic instability, progressive deformity, chronic pain, or insufficiency fractures, even in patients without a history of bone fragility or osteoporosis [2,3]. Therefore, pelvic ring integrity must be considered a critical variable in the surgical planning of sacral tumors.
In patients with tumors affecting the pelvic ring, studies have demonstrated prophylactic fixation to be efficient in preventing late onset complications, such as pathologic fractures or mechanical alterations. Assouline et al. evaluated the use of prophylactic percutaneous cemented screws in osteolytic pelvic lesions, obtaining successful consolidation in 98% of cases and a drastic reduction in fracture risk, even in the absence of open reconstruction [8]. These findings support the notion that prophylactic structural support is essential for maintaining long-term functionality, especially in wide or unstable resections.
Present recommendations suggest considering prophylactic lumbopelvic fixation in the following clinical contexts:
- Tumor resection comprising sacral ala or sacroiliac joint, due to the risk of posterior pelvic ring disruption [3]
- Total or high sacrectomies (S1 or above) which entail loss of axial vertebral support [4,10]
- Periacetabular resections, where acetabular loss precludes adequate functional loads without reconstruction [1,2]
- Broad pelvic defects that involve multiple regions [3,10]
- Patients with risk factors for insufficiency fractures, such as previous radiotherapy, extensive osteolysis (>4 cm), advanced age, or metabolic bone disease [8,9].
These indications support the emerging consensus that mechanical stability must be a primary surgical outcome, and it should be considered a parallel objective to oncologic control. Neglecting adequate structural stabilization in patients with a high biomechanical risk may severely jeopardize their functional outcome, even if tumor-free margins are achieved.
In this setting, sacral insufficiency fractures represent a severe late-onset complication. Clinical manifestation may resemble tumor recurrence, which hampers diagnosis and delays definitive treatment. These fractures often present with progressive axial pain and gait impairment, and they may require complex reinterventions [4,5].
We present a young patient with no previous history of osteopathy or osteotoxic treatments who developed an insufficiency fracture at the S1 vertebral body and residual sacral wing 6 months after sacral tumor resection. This event underscores the importance of incorporating biomechanical criteria within surgical planning, beyond usual oncologic analysis.
The pelvis constitutes an anatomically closed system, highly specialized for load transmission. Destabilization of the system, if left uncorrected or unprevented promptly, may lead to severe clinical consequences. Contemporary surgical planning in musculoskeletal oncology must integrate a systematic evaluation of the structural risk, incorporating anatomical, biomechanical, and bone quality criteria. This, in turn, optimizes functional outcomes and reduces long-term morbidity.
En bloc resection with wide oncologic margins remains the standard treatment for sacral chondrosarcoma. However, when key structures, such as the sacral ala or sacroiliac joint are resected, posterior pelvic ring stability is significantly compromised. The present case demonstrates how, despite the absence of classic bone fragility factors, the absence of prophylactic stabilization can result in insufficiency fractures with severe functional outcomes.
Both the case analysis and the present evidence reinforce the need for a multidimensional approach within oncologic preoperative planning. Systematic integration of biomechanical criteria allows the identification of patients at risk of post-operative structural instability and enables the implementation of effective prophylactic measures. This approach not only improves functional outcome and reduces the need for reinterventions but also enhances surgical safety in high-risk surgery, such as sacral in bloc resections.
Early recognition of pelvic biomechanical instability is essential after sacral tumor resection. Even in the absence of traditional fragility risk factors, resections involving the sacral ala or posterior pelvic ring may lead to insufficiency fractures. Incorporating biomechanical assessment into preoperative oncologic planning and considering prophylactic stabilization can prevent structural failure, reduce reoperations, and improve long-term functional outcomes.
References
- 1. Ghoneimy AM, El-Sherif AM, Abo-Elenen M, Khalil AG, Mohamed A, Farid M, et al. Surgical management of sacral chondrosarcoma: En bloc resection with and without lumbopelvic stabilization. World Neurosurg 2021;151:e61-70. [Google Scholar] [PubMed]
- 2. Griffin AM, Boland PJ, Grimer RJ, Ferguson PC, Wunder JS, Healey JH, et al. Residual bone defects following pelvic tumor resections: Reconstruction with allograft and the role of pelvic continuity in mechanical failure. Clin Orthop Relat Res 2015;473:869-76. [Google Scholar] [PubMed]
- 3. Wang Y, Wang Y, Kong L, Zhang L, Li J, Sun W, et al. Risk factors for sacral insufficiency fractures following en bloc resection of sacral tumors. Spine (Phila Pa 1976) 2019;44:E1013-20. [Google Scholar] [PubMed]
- 4. Tanaka T, Ogura K, Uehara K, Matsumine A, Nakamura T, Kawai A, et al. Sacral insufficiency fractures after total sacrectomy: Clinical features and risk factors. Eur Spine J 2018;27:359-67. [Google Scholar] [PubMed]
- 5. Jutte PC, Castelein RM, van der Woude HJ, van Royen BJ, Taminiau AH, Hogendoorn PCW, et al. Complications of pelvic and sacral tumor resections. Clin Orthop Relat Res 2001;390:159-68. [Google Scholar] [PubMed]
- 6. Wang B, Liu T, Wang X, Li Z, Zhou Y, Xu W, et al. Reconstruction strategies after en bloc resection of primary malignant tumors involving sacroiliac joint. Spine J 2020;20:965-74. [Google Scholar] [PubMed]
- 7. Gonzalez AS, Rivas GQ, Mena RC, Barrientos RY, Pacheco BM, Martínez L, et al. Resection of a sacral chordoma aided by neuronavigation: A case report. Interdiscip Neurosurg 2021;23:100985. [Google Scholar] [PubMed]
- 8. Assouline A, Ammari S, Pham TT, Bousson V, Hamze B, Laredo JD, et al. Prophylactic percutaneous consolidation of large osteolytic tumors of the pelvic ring using cement and screws. Eur J Surg Oncol 2021;47:2844-50. [Google Scholar] [PubMed]
- 9. Errani C, Mavrogenis AF, Cevolani L, Spinelli S, Picci P, Donati DM, et al. Risk factors for failure in pelvic resections and reconstructive surgery. Eur J Surg Oncol 2016;42:1384-91. [Google Scholar] [PubMed]
- 10. Archibeck MJ, Clanton TO, Martinez SA, Rhodes J, Randall RL, Jones DA, et al. Surgical navigation in orthopaedic oncology. J Am Acad Orthop Surg 2010;18:386-94. [Google Scholar] [PubMed]
- 11. Lin PP, Tamboli D, Lewis VO, Yan J, Yasko AW, Moon BS, et al. Surgical management of pelvic bone tumors. J Surg Oncol 2007;96:497-503. [Google Scholar] [PubMed]
- 12. Chen S, Wang Z, Teng W, Zhang Y, Zhou Y, Hu W, et al. Clinical analysis of lumbopelvic reconstruction after type I+II+III pelvic tumor resection. Front Oncol 2022;12:935059. [Google Scholar] [PubMed]
- 13. Lin X, Wu Z, Zhang C, Huang L, Gao Y, Chen Y, et al. Fractures after Enneking type I+II+III pelvic resections without lumbopelvic reconstruction: A retrospective study. Front Surg 2024;11:1266393. [Google Scholar] [PubMed]
- 14. Angelini A, Trovarelli G, Berizzi A, Pala E, Shen J, Ruggieri P, et al. Surgical margins in pelvic bone tumors: How wide should they be? Clin Orthop Relat Res 2020;478:607-18. [Google Scholar] [PubMed]