It is important to assess the fracture morphology, biology, and method of fixation in cases of non-union to provide optimal treatment. Selection of appropriate graft material and customizing it is vital in achieving union. Fibular strut graft can be effectively used in treating non-unions of distal tibia after reaming it and ensuring that the biological milieu at the fracture site is conducive to union.
Dr. Varigonda Sivani, Department Of Orthopaedics, GVPIHC and MT, Visakhapatnam, Andhra, Pradesh, India. E-mail sivavarigonda@gmail.com
Introduction: Distal tibial comminuted fractures are usually a result of high-energy trauma. The subcutaneous location of the bone pre-disposes to open fractures and decreased vascular supply. All these local and biological factors contribute to increased risk of non-union. Mechanical factors such as stability of the fixation and method of fixation also add to it. Hence, it is prudent to evaluate all these factors in a case of distal tibial non-union and choose optimal method of management of distal tibia non-union. This case presentation is portrayal of one such scenario.
Case Report: A 65-year-old male patient presented with non-union of extra-articular distal tibia comminuted fracture with distal tibial locking compression plate and fibular plate in situ. He was treated with ipsilateral fibular bone grafting and retention of the implants about 1 and 1/2 years after the injury. The bone has united within 11 months with uneventful post-operative period and with good functional outcome
Conclusion: This case shows that even with minimal intervention union can be achieved in notorious distal tibia non-unions if appropriate graft materials are chosen and customized accordingly. Evaluating various biological and mechanical causes of non-union and addressing them is key to favorable outcomes.
Keywords: Non-union, distal tibia, fibular graft.
Non-union of distal tibia, especially following an open Type-3A fracture, though not uncommon problem, is challenging to treat. Precarious blood supply and poor soft-tissue cover are few factors which contribute to non-union [1]. There is plethora of surgical options for non-union distal tibia ranging from exchanging nailing, plating with bone grafting to external fixators like Ilizarov [2,3]. However, before embarking on a treatment option, initial forces acting on the fracture, stability of earlier fixation, and biology of the fracture should be considered to decide on the optimal method of management. This case report is an illustration of one tibial non union treated with fibular autograft from ipsilateral limb without disturbing the original fixation.
A 65-year-old male patient met with a road traffic accident and sustained a Gustilo Anderson Type-3A fracture of tibia with bone exposed. On radiology, it is of AO 42A3 fracture, that is, extra-articular distal tibial fracture with metaphyseal comminution (Fig. 1). He was treated at a different center initially with debridement and primary fixation with anteromedial fixation with distal tibial LCP and fibula is fixed with a one-third tubular plate (Fig. 2).

Figure 1: X-ray after initial trauma.
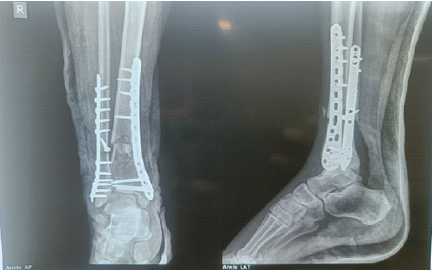
Figure 2: Immediate post-operative X-ray after initial fixation.
After 1 year and 3 months, the patient presented to the author’s outpatient department. On examination, the surgical scar was healthy. Tenderness is present at the fracture site. Range of motion of ankle was normal. Patient was walking with crutches. However, no signs of union are present on the radiograph and there are no signs of implant failure (Fig. 3). The case is diagnosed as aseptic non-union distal tibia with implants in situ.

Figure 3: One and half year post-operative X-ray after initial fixation showing non-union
Intraoperatively, the site of non-union is approached under anteromedial approach to tibia over the old scar. The proximal screws of the plate were removed and edges of the fracture are freshened and nibbled. Tibia is reamed with a 6 mm drill bit to stimulate the medullary blood flow.
Ipsilateral fibular graft is harvested with its medullary canal reamed to stimulate medullary blood flow. It was contoured into triflanged shape and inserted into the fracture site of tibia. The distal tibial locking compression plate (LCP) was fixed back proximally with new screws. Post-operative period was uneventful. At 3 months follow-up, callus response was observed (Fig. 4). At subsequent follow-ups at 5 months and 9 months, it was observed that the fracture is progressing to union. At 10 months, the fracture united completely (Fig. 5) and the patient was walking without any support (Fig. 6).

Figure 4: Immediate post-operative X-ray after placing fibular strut graft.
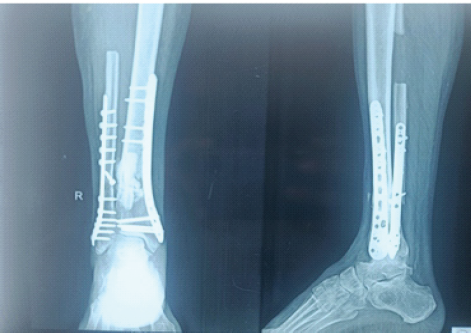
Figure 5: One-year follow-up X-ray showing union following fibular grafting.

Figure 6: Functional outcome at 1 year follow-up.
Non-union is one of the common complications of extra-articular distal tibia fractures despite internal fixation due to precarious blood supply and subcutaneous location of the bone [4]. Apart from the local factors which are responsible for non-union, there are certain factors like age more than 60 years, male gender, high-energy injury, and open injury, along with fixation model which increase the risk of non-union [5]. Among various treatment options for distal tibia extra-articular comminuted fractures, bridge plating is increasingly being used as it preserves fracture biology and is less invasive using minimally invasive plate osteosynthesis technique [6]. Bridge plating provides relative stability and fracture heals with callus formation. Too rigid a fixation or poor blood supply in such conditions lead to absence of callus formation and end up in non-union [7]. In the above case, even though bridge plating was done to tibia, open injury might have contributed to the atrophic non-union. Other reasons for lack of callus response could be rigid fixation of fibula with one-third tubular plate. Anterolateral plate or support is found to be biomechanically superior in valgus type of injury to distal tibia [8]. Non-vascularized fibular strut graft is shown to be effective in cases of non-union of neck of femur in some studies [9]. Fibula being cortical bone provides structural support. In addition, as the fibular graft gets incorporated with the surrounding bone, biological fixation can also be achieved [10]. Fibula thus acts as a “Biological Intra-medullary Nail’’ providing structural support. Its contact with the endosteal surface of tibia facilitates early fracture healing. It also helps in strengthening the osteopenic bone in elderly. Triflanged fibula holds both ends of the non-union firmly and might not even require additional fixation [11].
In the management of the non-union in the above case, following factors might have contributed to its union:
- Freshening of the fracture ends along with reaming of the tibia might have increased the local medullary blood supply.
- Reaming of the medullary cavity of the fibular graft before harvesting and replacing it might have induced some osteogenic capability of the graft.
- Fashioning the fibula to fit into the diaphysis of tibia gave snug fit, which contributed to stability and biological fixation.
- Osteotomy of fibula might have reduced the rigidity of the construct, there by creating a mechanical environment conducive to callus formation
- The placement of fibular graft at anterolateral aspect of tibia might have countered the valgus forces on the fracture.
Iliac crest graft is commonly used in these cases of non-union as it provides cortical and trabecular bone and it has limited role in mechanical activities in day-to-day activities [12]. However, there are limitations such as limited volume of iliac crest (30 cc) available in larger defects [12] and increased vertical resorption of iliac crest bone grafts [13]. In this case, there is requirement of not only osteoinduction but also a need for a lateral buttress in the area of comminution. Reaming the distal tibia, which is metaphyseal region and the fibular graft contributed to the osteoinduction as well as osteoconduction. The fibular strut provided the lateral support in the area of comminution.
Based on this case report, it can be conferred that, distal tibia comminuted fractures are prone to non-union due to compromised blood supply and surrounding soft tissue. Hence, maintenance of fracture biology, soft tissue is of utmost importance in fracture healing. Too rigid a fixation in bridge plating leads to lack of micromotion at fracture site and lack of callus response there. Hence, the fixation should be stable but not too rigid to inhibit fracture healing in bridge plating and relative stability pattern of fixation. Understanding the method of fixation and reason for failure is key in treating non-unions to prevent recurrent and resistant non-unions. Choosing and customizing appropriate graft, with minimal morbidity to the patient and optimal fixation strategies, is key for treating non-unions. Thus, non-vascular fibular strut graft with or without additional fixation can be used as an effective solution for diaphyseal non-unions by providing mechanical support and favorable biology with its osteoinductive and osteoconductive properties.
Reamed fibular strut graft can be used in extra-articular comminuted meta-diaphyseal fractures to achieve union. It not only provides structural support but might also exhibit osteoconductive and osteoinductive properties.
References
- 1. McMillan TE, Johnstone AJ. Technical considerations to avoid delayed and non-union. Injury 2017;48:64-8. [Google Scholar] [PubMed]
- 2. Ebraheim NA, Evans B, Liu X, Tanios M, Gillette M, Liu J. Comparison of intramedullary nail, plate, and external fixation in the treatment of distal tibia nonunions. Int Orthop 2017;41:1925-34. [Google Scholar] [PubMed]
- 3. Zhai WL, Xiong YF, Liu H, Zhang JH, Xu WZ, Wu J. Nonunion of the distal one-fourth of the tibia treated by retrograde tibial intramedullary nail. J Int Med Res 2024;52:3000605241289017. [Google Scholar] [PubMed]
- 4. Aravind S, Harshavardhan G, Suryakumar S. Resistant and refractory distal tibia non-union using an intramedullary free fibular graft and ilizarov fixation – an illustrative case report. J Orthop Case Rep 2024;14:45-9. [Google Scholar] [PubMed]
- 5. Tian R, Zheng F, Zhao W, Zhang Y, Yuan J, Zhang B, et al. Prevalence and influencing factors of nonunion in patients with tibial fracture: Systematic review and meta-analysis. J Orthop Surg Res 2020;15:377. [Google Scholar] [PubMed]
- 6. Abboud A, Masrouha K, Hanna T, Saghieh S. Union following biological and rigid fixations of distal tibia extra-articular fractures. Arch Bone Jt Surg 2020;8:162-7. [Google Scholar] [PubMed]
- 7. Simpson AH, Tsang ST. Non-union after plate fixation. Injury 2018;49 Suppl 1:S78-82. [Google Scholar] [PubMed]
- 8. Surendran, Langshong R, Shira MJ, Leya B, Saini M, Jopir A, et al. Surgical management of fracture lower end of tibia in adults with anterolateral plate- a prospective study in RIMS. Int J Acad Med Pharm 2023;5:1364-72. [Google Scholar] [PubMed]
- 9. Tripathy SK, Sen RK, Goyal T. Nonvascularized fibular grafting in nonunion of femoral neck fracture: A systematic review. Indian J Orthop 2016;50:345-51. [Google Scholar] [PubMed]
- 10. Roshan A, Ram S. The neglected femoral neck fracture in young adults: Review of a challenging problem. Clin Med Res 2008;6:33-9. [Google Scholar] [PubMed]
- 11. Yadav SS. The use of a free fibular strut as a “biological intramedullary nail” for the treatment of complex nonunion of long bones. JB JS Open Access 2018;3:e0050. [Google Scholar] [PubMed]
- 12. Gómez-Barrena E, Ehrnthaller C. Long bone uninfected non-union: Grafting techniques. EFORT Open Rev 2024;9:329-38. [Google Scholar] [PubMed]
- 13. Koo H, Hwang J, Choi BJ, Lee JW, Ohe JY, Jung J. Comparison of vertical bone resorption following various types of autologous block bone grafts. Maxillofac Plast Reconstr Surg 2023;45:38. [Google Scholar] [PubMed]