Anterior less invasive plating using indirect reduction and careful avoidance of fracture site distraction accelerates bone healing, decreases radial nerve injury when performed with judicious technique and early functional recovery while minimizing radial nerve risk in OTA/AO 12A–12B subset of fractures.
Dr. Anshul Raj, Department of Orthopaedics, Institute of Medical Sciences/Banaras Hindu University, Varanasi, Uttar Pradesh, India. E-mail: rajanshul281994@gmail.com
Introduction: The scope of this research was to examine the radiographic healing and functional results in OTA/AO type 12A and 12B humeral diaphyseal fractures (HDFs) treated surgically either by anterior minimally invasive plate osteosynthesis (MIPO) or by open reduction plate osteosynthesis (ORPO) along the posterior cortex of the humerus.
Materials and Methods: In this prospective cohort observational analysis, experienced orthopedic surgeons performed two different surgeries in two non-randomly allocated groups of 30 patients each. Outcomes measured radiographic healing, defined as cortical bridging on orthogonal radiographs, and shoulder and elbow functional scores at multiple intervals over 1 year using the University of California at Los Angeles (UCLA), the mayo elbow performance index (MEPI), and the disabilities of the arm, shoulder and hand (DASH) scores comparing the outcomes between both interventions using different statistical methods.
Results: The study found insignificant variations in the age, sex, or AO/OTA fracture types between the groups. MIPO group had a significantly shorter time to healing (13.1 ± 3.1 weeks vs. 18.1 ± 4.7 weeks; P = 0.03), a better functional result of the shoulder and elbow (UCLA: 34.2 ± 2.7 vs. 32.8 ± 3.1; P = 0.05; MEPI: 90.3 ± 10.8 vs 88.7 ± 9.8; P = 0.04), and a lower DASH score (15.8 ± 3.1 vs. 17.9 ± 5.8; P = 0.03) than ORPO. Complications included two non-unions in ORPO and one in MIPO; radial nerve palsy occurred in four cases treated with ORPO.
Conclusion: Anterior MIPO is a biologically favorable and skill-dependent approach for managing HDFs. While not simply a replacement for ORPO, it affords earlier radiographic union, reduced surgical morbidity, enhanced recovery of shoulder and elbow function, fewer secondary interventions, and allows safe avoidance of the radial and musculocutaneous nerves.
Keywords: Minimally invasive plate osteosynthesis, open reduction plate osteosynthesis, locking compression plate, Mayo elbow performance index, OTA/AO.
The incidence of humeral diaphyseal fractures (HDFs) varies from 1% to 4% of all fractures [1,2,3,4]. Minimally invasive plate osteosynthesis (MIPO) has gained popularity as a practical alternative to open reduction plate osteosynthesis (ORPO) for comminuted fractures [1,2,3], but its clinical indication for simple diaphyseal fractures (AO/OTA 12-A and 12-B) is still under investigation [4]. MIPO allows safe plate placement along the anterior, anterolateral, and medial surfaces of the humerus as it preserves the fracture hematoma and allows for biologic healing of the fracture, whereas ORPO happens through an anterolateral or posterior exposure. Radial nerve (RN) injury is a complication associated with ORPO, especially when the anterolateral dissection occurs more distally over the mid-distal shaft and in the spiral groove region on the posterior surface [4,5]. Hence, an important clinical question arises: How safe and efficacious is MIPO for the treatment of transverse, oblique, spiral, and wedge-type HDFs in comparison to traditional open reduction techniques? [1,2,3,4,5]. Recent randomized controlled trials and meta-analyses have assessed the best fixation strategies for HDFs and have thus assisted in evidence-based decision-making and optimization of treatment outcomes [5,6,7]. While fracture union is well documented for both interventions, functional restoration is correspondingly crucial as it has a significant impact on the quality of life [6,7,8,9]. By comparing these two treatment modalities, this study sought to critically appraise the outcomes of MIPO and ORPO on fracture union time and scoring according to standardized scoring systems such as the University of California, Los Angeles (UCLA) score; Mayo Elbow Performance Index (MEPI); and disabilities of the arm, shoulder, and hand (DASH) scores. These indices integrate patient-reported outcomes with clinically derived measurements [1,2,3,4,6,8,9].
The Department of Orthopedics conducted this study from March 2022 to March 2024. The Institutional Review Board approval was granted for this research (approval no. -Dean/2023/EC/6104), and written consent from all the participants was taken before the intervention.
Study population
This analysis included 60 patients with HDFs at a single tertiary care academic hospital between 2022 and 2024, non-randomly allocated to either Group A (MIPO, n = 30) or Group B (ORPO, n = 30) [1,4,6].
Study design
This single-center, prospective, non-randomized, comparative, observational analysis aimed to evaluate the radiographic healing and functional results of anterior MIPO versus ORPO along the posterior cortex of the humerus.
Participants
The eligible subjects comprised adults aged 18–65 years with closed HDFs (AO/OTA 12A and B) <3 weeks old. The exclusion criteria were adults with open HDFs, closed HDFs (AO/OTA 12C), fractures >3 weeks of age, pathological fractures, prior humeral surgery, fracture extension to the metaphysis, and RN injury to maintain uniformity [1,6].
Treatment modalities
Surgical techniques
MIPO (Group A)
Preoperatively, the operating surgeon predetermined the length of the narrow locking compression plate (LCP) fluoroscopically. Using a pair of incisions, one proximal in the deltopectoral interval and one distal incision 1 inch above the olecranon fossa of approximately 3 cm each, a long periosteal elevator creates a submuscular, extraperiosteal tunnel, allowing the plate to be positioned on the humerus [1,5]. Using indirect reduction under fluoroscopic guidance, special attention was paid to ensure that proper length, alignment, and no distraction at the fracture site were visible. The musculocutaneous nerves were carefully protected with medially retracting biceps brachii to expose the brachialis [9], and a couple of screws were placed on each end through the LCP and anterior cortex of the bone. Hence, the RN did not enter the path and was unnecessary to expose during the surgery [9,10,11].
ORPO (Group B)
With the arm aligned over the side post and the elbow supported, the surgeon utilised a dorsal triceps-splitting approach and carefully identified the radial nerve(RN) near the aponeurosis of the lateral and medial heads of the triceps by locating and tracing the lower lateral cutaneous nerve, first identified on the lateral humeral cortex. RN, crossing medially to laterally, is dissected and retracted to allow for direct visualisation of the fracture. Localised periosteal stripping at the opposing cortical edges, followed by direct stabilisation of bony fragments and osteosynthesis using a DCP, with supplementary lag screws anchorage for oblique or wedge-type fragments where appropriate. While sliding the dynamic compression plate (DCP) over the dorsal shaft, the scrub team ensures that neurovascular structures are cautiously protected during drilling through the bone [1,4,5,7,8,10].
Rehabilitation protocol
Post-operative rehabilitation protocols varied between groups. The MIPO group initiated passive overhead movements and range of motion (ROM) exercises within 48 h of surgery (post-operative pain score of 4–6 on the Visual Analog Scale [VAS]), while ORPO commenced similar exercises after 1 week. Weight training exercises began after post-radiologic confirmation of fracture consolidation [1,2,9].
Follow-up and outcome measures
The orthopedic surgeons and a radiologist assessed the fracture union radiographically by using predefined criteria (cortical bridging and callus formation) and upper limb functional outcome using UCLA, MEPI, and DASH scores, respectively, reviewed at 6-week post-treatment, followed by assessments at 3 months, 6 months, and 1 year [1,2,10,12,13,14,15].
Sources
The UCLA and MEPI are publicly available [12,13]. Permission for academic and non-commercial use of the DASH was granted by the copyright holder [15].
Statistical method and study variables
Data were collected at each follow-up visit and entered into a secure database. Statistical evaluation was done with IBM Statistical Package for the Social Sciences Software (version 26.0) for intergroup comparisons. Unpaired t-tests were used to compare continuous variables between groups, while categorical variables were analyzed using the chi-square test. Comparison of changes at the follow-up within each group was assessed by repeated-measures analysis of variance (RM-ANOVA) and linear mixed-effects models. Correlation analysis between union time and functional outcomes was achieved using Spearman’s rank correlation coefficient and multiple linear regression while adjusting for confounding factors.
Participants’ mean age (years) in the MIPO group was 39 ± 12.32 compared with 36.42 ± 12.61 in the ORPO group. The distribution of both groups showed a predominance of the male gender with 40 males and 20 females in both groups. Both groups showed a nearly equal prevalence of tobacco use (Table 1).
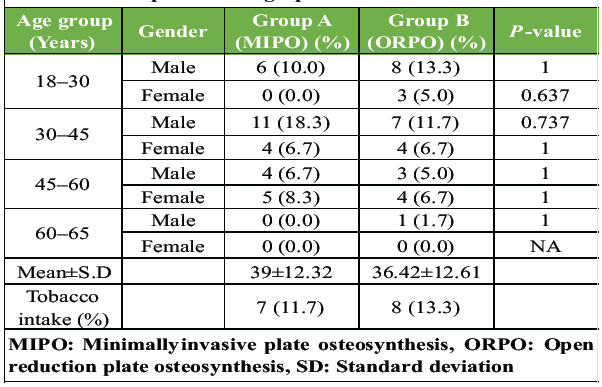
Table 1: Participants’ demographics
Distribution of the OTA/AO classifications was comparable between the groups, with insignificant statistical variation. The common type of fracture was 12A3 in 22 patients (36.7%) and 12A2 in 18 patients (30.0%). The remaining comprised 12B1 in 7 patients (11.7%), 12A1 in 5 patients (8.3%), and 12B2 and 12B3 in 4 patients (6.7%).
Most of the injuries sustained in road traffic accidents (36 patients, 60.0%), followed by falls (17 patients, 28.3%), and sports/direct impact injuries (7 patients, 11.7%), were identified as the mechanisms of injury. AO/OTA fracture patterns are displayed in a bar chart, and the modes of injury are depicted in a pie chart (Figs. 1A and 1B).
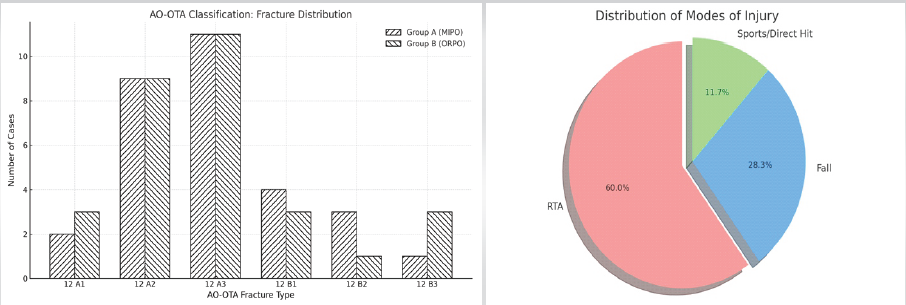
Fig. 1: The distribution of OTA/AO Fracture Types and modes of injury. (A)Vertical bar chart displays the Classification of AO-OTA fractures by distribution.
(B) Pie Chart indicates the distribution of the modes of injury.
Radiological outcomes
The mean time taken for union was 13.3 ± 3.1 weeks (95% confidence interval [CI]: 10.9–20) in Group A and 18.1 ± 4.7 weeks in Group B (95% CI: 12.1–24), which shows a significant statistical variation (P = 0.03, independent t-test). Both approaches helped in healing the bone, with Group A having a quicker union (Figs. 2A, 2B and 3) [1,2,4,7,15].
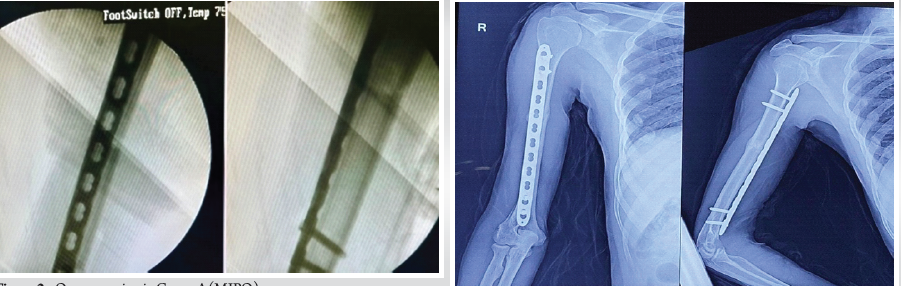
Fig. 2: Osseous union in Group A (MIPO (A)Intraoperative fluoroscopic orthogonal images demonstrating acceptable length and alignment of the fracture, with a narrow locking compression plate spanning the anterior cortex of the right humerus.
(B) The fracture was observed to have healed at 11 weeks post-surgery (indicated by the label ‘early callus’), with the 4 cortices touching on both AP and lateral images. The orientation is indicated by ‘R’ (right).
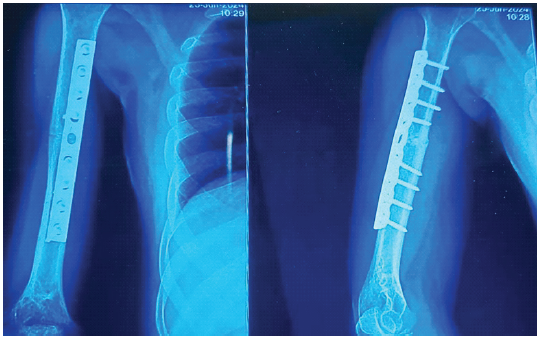
Fig. 3: Osseous healing in the ORPO Group: An AP and lateral radiographic images of direct fixation (via a dynamic compression plate) along the posterior cortex of the right humerus, without any discernible fracture line, at 14 weeks post-surgery.
Functional outcomes
The UCLA scores were higher for Group A in all aspects: Patient satisfaction, pain, ROM, and strength. Mean scores were 34.2 ± 2.7 for Group A and 32.8 ± 3.1 for Group B (P = 0.05) [9,12]. The total MEPI score was significantly higher in Group A (90.33 ± 10.8) than in Group B (88.7 ± 9.8) (P = 0.04) for elbow function over the specified periods, highlighting a positive recovery trend [9,10,13]. Finally, DASH scores significantly decreased over time in both groups (P = 0.03) (15.8 ± 3.11) in comparison with Group B (17.9 ± 5.8), indicating better upper limb function and less disability post-treatment (Table 2) [1,2,3,6,7,8,9,10,14].
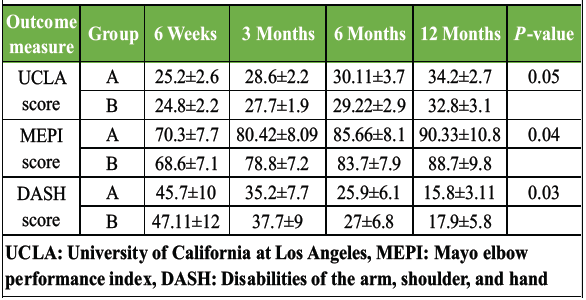
Table 2: Functional outcomes (UCLA, MEPI, DASH) at different follow-up periods
A correlation matrix illustrated the interrelationships among functional scores and time to union, while regression analysis assessed their independent association with clinical recovery (Figs. 4A and 4B).
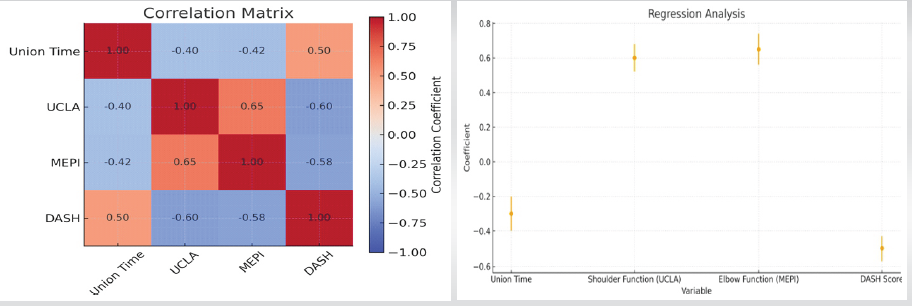
Fig. 4: Association between union time and functional scores.(A)Correlation matrix identifies relationships among different variables of functional scores: Positive correlations are indicative of higher functional scores, and negative correlations represent lower functional scores for better recovery.
(B) Regression coefficients between multiple predictors (Union Time, UCLA, MEPI, and DASH scores) revealed that higher UCLA and MEPI scores and lower union time and lower DASH scores are positive determinants of recovery.
Complications
The overall complication rate was 15% (nine patients), and 5% (three patients) required secondary surgery. Nonunion occurred in one patient (AO/OTA 12 A3) in the MIPO group and two patients (AO/OTA 12A3 and 12B3) in the ORPO group who underwent secondary surgical intervention (Figs. 5A and 5B). Other complications in the post-operative period included distraction in 3.33% (2 patients in Group A) and RN palsy in 6.67% (4 patients in Group B). Hematoma, infection, delayed union, malalignment, irritation due to implants, or screw pullout did not occur.
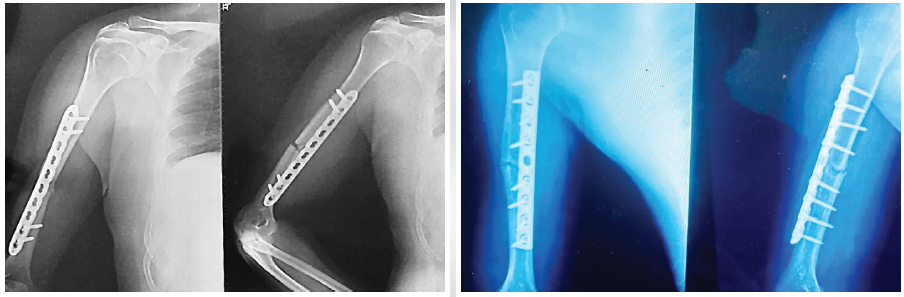
Fig. 5: Nonunion requiring secondary surgical interventions. (A) Anteroposterior and Lateral radiographic images of the right humerus taken 6 months after 10-Hole LCP Fixation exhibiting biomechanical failure, marked by evident distraction, inadequate bridging of the fracture and lack of callus formation (R=right). (B) AP and lateral radiographic views after using a 9-hole DCP in the right humerus also demonstrated no signs of osseous healing, and a gap was still evident at six months.
9-hole DCP in the right humerus also demonstrated no signs of osseous healing, and a gap was still evident at six months.
Available evidence suggests that the use of MIPO and ORPO is an effective surgical treatment for HDFs and seems to be superior to intramedullary nailing and functional bracing in terms of functional results and union rate [1,2,3,4,6,7]. These results concur with those of previous studies on less invasive fixation of HDFs [3,6,7]. This anterior MIPO approach has biological and soft-tissue advantages over ORPO by limiting surgical exposure and thus preserving periosteal perfusion and the native fracture hematoma while avoiding devitalization of fracture fragments [1,5,10]. A long periosteal elevator facilitates the surgeon to accommodate plate passage in the submuscular, extra-periosteal tunnel, and mobilize any interposed soft tissues [1,2,11]. Even so, the RN remains particularly vulnerable, especially because the screws are oriented anteriorly to posteriorly in the region of the deltoid insertion and mid-diaphysis of the humerus. The incorporation of longer anterior plates in this series diminishes the likelihood of RN injury and enhances the stability of this construct, while two proximal and two distal bicortical screws enhance stability under physiologic loading conditions with a more uniform stress distribution [1,9,10]. Distally, medial displacement of the biceps brachii provides a safe interval that minimizes the risk of musculocutaneous nerve injury [9,11]. MIPO maximizes intraoperative radiation exposure due to manual maintenance of reduction and alignment without distraction using fluoroscopy [1,2,4,5,9]. Intraoperative distraction in these cases necessitates immediate screw revision. The added perioperative benefits of MIPO include less intraoperative blood loss, shorter hospital stay, and favorable cosmetic results [2,3,4,5,6,10]. ORPO has the advantage of direct visualization, accurate and stable reduction, and less fluoroscopic exposure and is more familiar and widely accepted. The flat, broad posterior surface of the humerus is an advantage in mid-distal HDFs due to ease in contouring plates and screw purchase is uniform for the length of the shaft and favorable for compression plating, whereas plate positioning and fixation are more problematic on a rounded, convex anterolateral surface [4,5,8]. Furthermore, exposure of the RN during deep dissection of the mid-distal diaphysis increases the risk of injury owing to limited nerve mobility.
One patient in Group A had a distraction requiring autologous bone marrow injection, which achieved union [2,8]. Revision surgery for non-union in one patient from Group A and two from Group B involved implant removal and revision plating on the posterior surface using autologous iliac crest grafting [10]. Four cases of RN palsy in the ORPO: Two recovered partially, while the remaining two regained their nerve function in 8 months [5,6,8].
Rehabilitation began when post-operative pain was sufficiently reduced, as reflected by the VAS scores, to allow early ROM in both groups [9]. One of the strengths of this study is the use of standardized functional assessment tools such as the UCLA, MEPI, and DASH scores, which are useful in clinical settings [12,13,14,15].
Limitations
The limitations of this study are that it is a single-center, non-randomized study with a short duration of follow-up and non-probability sampling, which may constrain generalizability and raise potential selection and performance biases.
Implications for practice and future directions
Larger multicenter randomized controlled trials with longer follow-up to conclude the findings and evaluate patient-reported long-term therapeutic effects of MIPO in AO/OTA 12A and 12B HDFs.
MIPO, especially through an anterior approach, results in better shoulder and elbow functions than direct plate osteosynthesis along the posterior cortex of the humerus. Radiographic healing was faster with MIPO. Operation demands special technical skills to overcome distractions during surgery. Injecting bone marrow enhances the healing process in distraction. Anterior MIPO carries a lower risk to the radial and musculocutaneous nerves for all HDFs to be treated without compromise.
MIPO provides faster radiographic union and better early functional recovery in OTA/AO 12A and 12B humeral shaft fractures than open posterior plating. Moreover, it reduces the risk of injury to the RN by respecting soft-tissue biology and preserving the fracture hematoma. The union occurs with both approaches, but MIPO has better patient-reported functional (PROM) recovery at 1 year.
References
- 1. Sugumar N, Sathiyaseelan N, Purushothaman JR, Natarajan S. Assessing functional and radiological outcomes: Open reduction and internal fixation vs. Minimally invasive plate osteosynthesis for humerus shaft fractures – a prospective comparative study. Int Orthop 2024;48:2979-91. [Google Scholar] [PubMed]
- 2. Yang Z, Ouyang B, Yang J, Liu D, Kang X. Anterior medial minimally invasive plate osteosynthesis for humeral shaft fractures shows superior early shoulder and elbow function compared to locking compression plate: A retrospective study. Injury 2024;55:111692. [Google Scholar] [PubMed]
- 3. Colasanti CA, Anil U, Cerasani MN, Li ZI, Morgan AM, Simovitch RW, et al. Management of humeral shaft fracture: A network meta-analysis of individual treatment modalities. J Orthop Trauma 2024;38:e257-66. [Google Scholar] [PubMed]
- 4. Yang J, Liu D, Zhang L, Lu Z, Liu T, Tao C. Treatment of humeral shaft fractures: A new minimally-invasive plate osteosynthesis versus open reduction and internal fixation: A case control study. BMC Surg 2021;21:349. [Google Scholar] [PubMed]
- 5. Orapiriyakul W, Apivatthakakul V, Theppariyapol B, Apivatthakakul T. Humerus shaft fractures, approaches and management. J Clin Orthop Trauma 2023;43:102230. [Google Scholar] [PubMed]
- 6. Den Hartog D, Mahabier KC, Van Bergen SH, Verhofstad MH, Van Lieshout EM. Functional and clinical outcomes after plate osteosynthesis versus intramedullary nailing of a humeral shaft fracture. J Bone Joint Surg 2023;105:1101-11. [Google Scholar] [PubMed]
- 7. Zavras AG, Monahan KT, Winek NC, Pan T, Altman GT, Altman DT, et al. Conservative management with functional brace versus various surgical fixation techniques for humeral shaft fractures: A network meta-analysis. J Bone Joint Surg Am 2023;105:1112-22. [Google Scholar] [PubMed]
- 8. Randell M, Glatt V, Stabler A, Bussoletti T, Hohmann E, Tetsworth K. Anterior minimally invasive plate osteosynthesis for humeral shaft fractures is safer than open reduction internal fixation: A matched case-controlled comparison. J Orthop Trauma 2021;35:424-9. [Google Scholar] [PubMed]
- 9. Mahmoud HF, Farhan AH, Fahmy FS. Assessment of shoulder function after internal fixation of humeral diaphyseal fractures in young adults: A prospective comparative study. Adv Orthop 2021;2021:9471009. [Google Scholar] [PubMed]
- 10. Randell M, Glatt V, Stabler A, Bussoletti T, Hohmann E, Tetsworth K. Anterior minimally invasive plate osteosynthesis for humeral shaft fractures is safer than open reduction internal fixation: A matched case-controlled comparison. J Orthop Trauma 2021;35:424-9. [Google Scholar] [PubMed]
- 11. Giordano M, Giordano V, Gameiro VS, Belangero W, Livani B, Giannoudis PV, et al. Anterior minimally invasive plating osteosynthesis technique (MIPO) for humeral shaft fractures: An anatomical study of neuromuscular structures at risk. Eur J Orthop Surg Traumatol 2020;31:449-58. [Google Scholar] [PubMed]
- 12. LWW. Ucla shoulder rating scale. J Orthop Trauma 2006;20:S139-40. [Google Scholar] [PubMed]
- 13. LWW. Mayo elbow performance score. J Orthop Trauma 2006;20:S127. [Google Scholar] [PubMed]
- 14. Jester A, Harth A, Wind G, Germann G, Sauerbier M. Disabilities of the arm, shoulder and hand (DASH) questionnaire: Determining functional activity profiles in patients with upper extremity disorders. J Hand Surg Br. 2005 Feb;30(1):23-8. doi: 10.1016/j.jhsb.2004.08.008. PMID: 15620487. [Google Scholar] [PubMed] [CrossRef]
- 15. Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord 2003;4:11. [Google Scholar] [PubMed]