Remote thoracic osteotomy can simultaneously correct sagittal imbalance and stabilize cervical fractures in ankylosing spondylitis, offering a safe alternative to site-focused fixation.
Dr. Abhay Tyagi, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: abhay20tyagi@gmail.com
Introduction: Ankylosing spondylitis (AS) predisposes patients to unstable spinal fractures due to spinal rigidity and osteoporosis, often complicated by severe kyphotic deformity.
Case Report: A 56-year-old man with AS presented with neck pain after a trivial fall. He had severe thoracic kyphosis, a rigid spine, and impaired horizontal gaze. Neurological examination was normal. Diagnosis, Intervention, and Outcomes: Computed tomography and magnetic resonance imaging revealed an AO Type B2, N0, M3 fracture at C7 in a fused spine. A thoracic vertebral column resection (D5) with long posterior instrumentation was performed to achieve both fracture stabilization and sagittal alignment correction. Postoperatively, the patient demonstrated improved horizontal gaze and standing balance. At 2-year follow-up, correction was maintained without complications.
Conclusion: Remote thoracic osteotomy can stabilize cervical fractures in AS while correcting global sagittal alignment. This approach offers a safe and effective alternative to traditional site-focused strategies.
Keywords: Ankylosing spondylitis, cervical spine fracture, thoracic osteotomy, vertebral column resection, sagittal balance.
Ankylosing spondylitis (AS) is a chronic inflammatory disease characterized by progressive ossification of spinal ligaments, resulting in a rigid kyphotic spine. This rigidity, combined with osteoporosis, predisposes patients to unstable spinal fractures, even after minor trauma [1,2]. These fractures are often missed or diagnosed late due to altered anatomy and can lead to neurological decline or pseudoarthrosis if untreated [3]. Conventional strategies focus on fracture fixation with or without deformity correction. While intraoperative manipulation at the fracture site has been described [4,5], such methods may be inadequate in global deformity or when fractures occur distant from the kyphotic apex. This case highlights a novel approach – thoracic osteotomy remote from the fracture site – to correct deformity and stabilize the cervical fracture simultaneously.
Patient information
A 56-year-old man with a 20-year history of AS presented with neck pain following a trivial fall. He had a rigid thoracic kyphotic deformity with impaired horizontal gaze. There was localized tenderness at C7 but no neurological deficit.
Clinical findings
Tenderness at C7 with normal neurological examination.
Diagnostic assessment
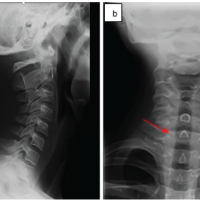
Computed tomography (CT) and magnetic resonance imaging confirmed an AO Type B2, N0, M3 fracture at C7 in a fused ankylosed spine (Fig. 1). Global sagittal profile assessment showed severe thoracic kyphosis with chin-brow vertical angle (CBVA) of 62° and sagittal vertical axis (SVA) of +8 cm. The kyphotic apex was localized at D5 on radiographs and CT.
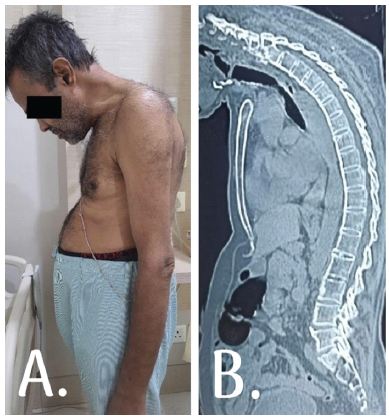
Figure 1: (a) Preoperative clinical photograph showing rigid thoracic kyphosis with impaired horizontal gaze. (b) Preoperative computed tomography scan sagittal reconstruction demonstrating fused ankylosed spine and AO type B2 fracture at C7.
Therapeutic intervention
A remote thoracic vertebral column resection (VCR) at D5 was chosen, rather than direct fracture fixation at C7, to simultaneously address the global sagittal deformity and achieve indirect stabilization of the fracture. O perative details (Fig. 2):
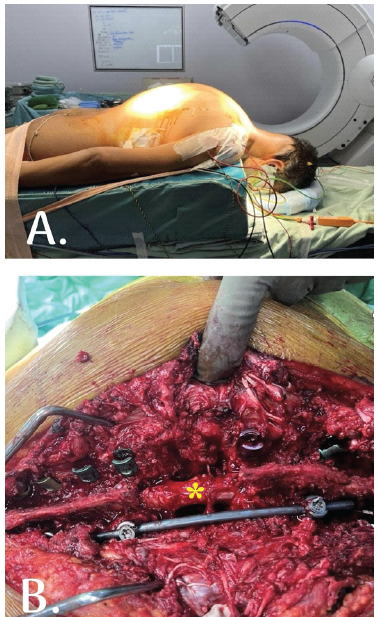
Figure 2: (a) Patient positioning in prone frame with head secured prior to osteotomy. (b) Intraoperative image demonstrating vertebral column resection at D5 (asterisk), with long posterior instrumentation extending cranially to stabilize the cervical fracture and caudally to D10.
- Approach: Standard posterior midline
- Osteotomy: Complete VCR at
- Fixation: Pedicle screw
- Neuromonitoring: Continuous intraoperative neurophysiological monitoring showed no
- Duration: 6
- Estimated blood loss: ~1,800 mL; managed with cell salvage and
- Complications: None
Perioperative course: The patient was managed in the intensive care unit for 48 h with a stable neurological status. No wound or systemic complications occurred.
Follow-up and outcomes
Immediate
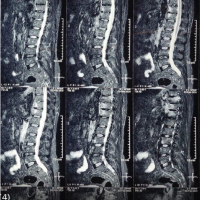
Postoperative radiographs confirmed fracture stabilization and restoration of sagittal alignment (Fig. 3). Global kyphosis improved from 82° to 46°, CBVA from 62° to 11°, and SVA from +8 cm to +2 cm (Table 1).
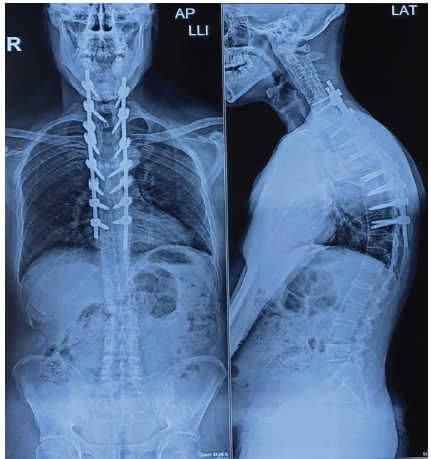
Figure 3: Postoperative lateral radiograph showing correction of sagittal alignment. The cervical fracture site at C7 is stabilized.
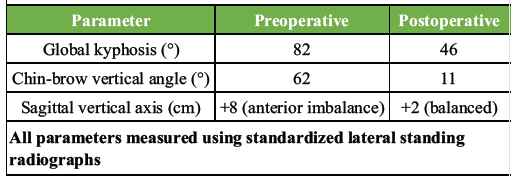
Table 1: Pre- and postoperative radiographic parameters
Functional outcomes
The patient reported improved horizontal gaze, the ability to ambulate independently, and return to daily activities. Although validated functional outcome scores such as the Oswestry disability index and SF-36 were not recorded, clinical assessment confirmed improved posture and mobility.
Long-term
At 2-year follow-up, the correction was maintained with no implant failure, pseudoarthrosis, or neurological deterioration (Fig. 4). The patient remained independent in activities of daily living and reported sustained improvement in quality of life.

Figure 4: Clinical photograph at 2-year follow-up demonstrating improved posture and restored horizontal gaze, with maintained correction.
Fractures in AS patients are challenging due to fused segments, osteoporosis, and altered spinal biomechanics [1,3]. Recent literature has established that surgical management is now the preferred approach, with nonsurgical treatment associated with failure rates exceeding 50% and poor neurological outcomes [6,7]. Traditional approaches focus on site stabilization, sometimes with osteotomy at the fracture site [4,5]. Cervical fractures are particularly risky due to nearby critical neurovascular structures. In this case, a remote thoracic VCR (D5) was performed to restore sagittal alignment and indirectly stabilize the cervical fracture. Unlike reports of cervical pedicle subtraction osteotomy (PSO) with higher complications [5], our approach minimized risks while achieving functional and radiographic improvements. The decision was guided by principles of targeting the kyphotic apex to restore balance [8,9]. This strategy avoided direct manipulation of the unstable fracture and leveraged long posterior constructs for stabilization. Our results align with reports of elective PSO in AS without fracture [10], but with the added benefit of single-stage correction of both instability and deformity.
Limitations
Single-patient design, short follow-up, and lack of quantitative functional outcome measures.
Take-away lesson
Remote thoracic osteotomy can be an effective alternative to site-focused stabilization in AS patients with cervical fractures and severe kyphosis.
This case illustrates that remote thoracic osteotomy can be applied to address both cervical fracture stabilization and sagittal imbalance in AS. By targeting the kyphotic apex rather than the fracture site, alignment restoration and indirect stabilization were achieved in a single stage. Remote osteotomy may represent a feasible alternative in carefully selected patients, but its role must be confirmed in larger comparative studies.
Remote thoracic vertebral column resection provides a powerful single-stage solution for both deformity correction and fracture stabilization in ankylosing spondylitis with cervical involvement.
References
- 1. Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;18:145-56. [Google Scholar] [PubMed]
- 2. Reinhold M, Knop C, Kneitz C, Disch A. Spine fractures in ankylosing diseases: Recommendations of the spine section of the German society for orthopaedics and trauma (DGOU). Global Spine J 2018;8 2 Suppl:56S-68. [Google Scholar] [PubMed]
- 3. Rustagi T, Drazin D, Oner C, York J, Schroeder GD, Vaccaro AR. Fractures in spinal ankylosing disorders: A review. Spine (Phila Pa 1976) 2014;39:1198-207. [Google Scholar] [PubMed]
- 4. Sapkas G, Kateros K, Papadakis SA, Brilakis E, Machairas G. Surgical treatment of spinal fractures in ankylosing spondylitis. Eur Spine J 2009;18:132-6. [Google Scholar] [PubMed]
- 5. Urbanski W, Zaluski R. Surgical treatment of spinal fracture in a patient with ankylosing spondylitis: An opportunity to correct spinal deformity simultaneously with fracture fixation? Cureus 2022;14:e21936. [Google Scholar] [PubMed]
- 6. Musa G, Phiri J, Ndandja DT, Familia K, Barrientos RE, Mwela BM, et al. Management of cervical fractures in ankylosing spondylitis: A ten-year systemic review of surgical and nonsurgical outcomes. Neurosurg Rev 2025;48:234. [Google Scholar] [PubMed]
- 7. Wang L, Song Y, Liu L, Wang Y, Gao Z, Lu X. Analysis of risk factors affecting postoperative neurological recovery in patients with cervical fractures. Spine J 2024;24:1456-65. [Google Scholar] [PubMed]
- 8. Van Royen BJ, De Gast A. Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment. Ann Rheum Dis 1999;58:399-406. [Google Scholar] [PubMed]
- 9. Chen HW, Chen IH. Strategies for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. Spine (Phila Pa 1976) 2006;31:70-9. [Google Scholar] [PubMed]
- 10. Kim KT, Park DH, Lee SH, Lee JH. Results of corrective osteotomy and treatment strategy for ankylosing spondylitis with kyphotic deformity. Clin Orthop Surg 2015;7:330-6. [Google Scholar] [PubMed]