Early diagnosis and timely surgical management are crucial to halt disease progression, preserve carpal architecture, and optimize long-term functional outcomes. Furthermore, this case series underscores the importance of individualized surgical planning based on disease stage, patient activity level, and anatomical considerations.
Dr. Nischay Kaushik, Department of Orthopaedics, Dr. BSA Medical College and Hospital, Rohini, New Delhi, India. E-mail: nikku1280@gmail.com
Introduction: Kienböck’s disease results from compromised lunate vascularity and often affects young individuals performing heavy manual tasks. Radial shortening osteotomy (RSO) is widely used to reduce lunate loading in cases with ulnar-negative variance.
Materials and Methods: Five patients diagnosed with Lichtman stage IIIA Kienböck’s disease were treated with RSO. All procedures were performed through a volar approach using locking plate fixation. Pain levels, wrist motion, grip strength, modified Mayo scores, and Disabilities of the Arm, Shoulder, and Hand scores were recorded before surgery and at 12–14 months postoperatively. Radiographs were reviewed for ulnar variance correction and any signs of progression.
Results: All patients showed meaningful reductions in pain, improved wrist mobility, increased grip strength, and higher functional scores at final follow-up. Mayo scores ranged from 85 to 94. None progressed to advanced stages, and no complications occurred.
Conclusion: RSO yielded consistent improvement in symptoms and function while maintaining carpal architecture in this series. Early recognition and timely intervention remain essential for optimal treatment outcomes.
Keywords: Kienböck’s disease, radial osteotomy, lunate necrosis, wrist surgery, ulnar variance.
Kienböck’s disease, first described by Robert Kienböck in 1910, is an idiopathic avascular necrosis of the lunate bone, leading to progressive fragmentation, collapse, and eventual carpal instability if untreated [1]. The etiology remains multifactorial, involving vascular insufficiency, mechanical overload, and anatomical predispositions such as ulnar-negative variance, which increases load transmission through the radiolunate joint [2,3]. The Lichtman classification, based on radiographic and magnetic resonance imaging (MRI) findings, stages the disease from I (normal radiographs with MRI signal changes) to IV (advanced carpal collapse and osteoarthritis) [4]. Stage IIIA specifically denotes lunate collapse without fixed scaphoid rotation or carpal malalignment, representing an early advanced phase amenable to joint-leveling procedures [1]. Treatment strategies are stage-dependent, with conservative approaches (immobilization and analgesics) often insufficient for progressive symptoms in stages II-III [5]. Surgical options include core decompression, vascularized bone grafting, and unloading procedures such as radial shortening osteotomy (RSO) or capitate shortening [6,7]. RSO, particularly indicated for ulnar-negative variance (>1 mm), aims to equalize forearm length, redistribute forces across the wrist, and potentially promote lunate revascularization by reducing compressive stress [8,9]. Retrospective studies have reported favorable long-term outcomes, with pain relief, improved function, and grip strength in 75–95% of cases, though radiographic progression occurs in 19–44% [8,10,11]. This study presents clinical and radiographic results from five consecutive cases managed with RSO for stage IIIA disease.
Patient selection
Five male patients between 27 and 32 years of age presented with persistent dorsal wrist pain unresponsive to conservative therapy. Eligibility criteria included:
- MRI and radiographic confirmation of stage IIIA disease
- Presence of ulnar-negative variance
- Absence of carpal collapse or degenerative changes
- Willingness to undergo surgery and rehabilitation.
All patients were employed in labor-intensive occupations.
Surgical technique
RSO was performed using a standardized technique in all five patients.
Preoperative planning
- Standard posteroanterior, lateral, and oblique wrist radiographs were obtained
- MRI was used to confirm Stage IIIA Kienböck’s disease and assess lunate vascularity.
- Amount of shortening (2–3 mm) was determined based on ulnar variance and load-distribution goals.
Surgical steps
- Patient positioning: Patients were placed supine with the operative arm on a radiolucent hand table. A tourniquet was applied
- Approach: A volar Henry approach was used. Care was taken to protect the radial artery and superficial radial nerve branches
- Exposure: The pronator teres and brachioradialis were gently retracted to expose the distal radial diaphysis
- Osteotomy: A transverse osteotomy was performed using an oscillating saw of radius. A measured segment (2–3 mm) was excised based on preoperative planning
- Shortening and alignment: Bone ends were approximated manually, achieving the planned reduction to neutral ulnar variance
- Fixation: A volar locking plate was applied. Positioning was confirmed using fluoroscopy to ensure correct alignment and screw placement
- Closure: Layered closure was performed after confirming hemostasis.
Post-operative protocol
- Wrist immobilization in a splint for 4–5 weeks
- Physiotherapy began after immobilization, focusing on gradual range of motion (ROM) recovery
- Strengthening exercises were initiated at 8–10 weeks.
Outcome measures
Evaluations were conducted preoperatively and at final follow-up using:
- Visual analog scale (VAS) for pain
- wrist flexion and extension range
- dynamometric grip strength (percentage of contralateral side)
- modified Mayo wrist score
- Disabilities of the Arm, Shoulder, and Hand (DASH) score.
Radiographs were examined for maintenance of carpal alignment, ulnar variance correction, and progression of disease stage.
Case descriptions
Case 1
30-year-old construction worker; pre-operative VAS 7/10, ROM 45°/50°; 3-mm shortening. At 1 year: VAS 0/10, ROM 65°/60°, grip 88%, Mayo 92, DASH 5; no radiographic progression.
Case 2
28-year-old mechanic; VAS 6/10, ROM 50°/55°; 2.5-mm shortening. At 14 months: VAS 1/10, ROM 60°/65°, grip 85%, Mayo 88, DASH 8; stable lunate morphology.
Case 3
32-year-old farmer; VAS 8/10, ROM 40°/45°; 3-mm shortening. At 12 months: VAS 1/10, ROM 55°/60°, grip 82%, Mayo 85, DASH 10; no collapse progression.
Case 4
27-year-old welder; VAS 6/10, ROM 50°/40°; 2-mm shortening. At 13 months: VAS 1/10, ROM 60°/55°, grip 87%, Mayo 90, DASH 7; carpal alignment preserved.
Case 5
29-year-old laborer; VAS 7/10, ROM 45°/50°; 3-mm shortening. At 12 months: VAS 0/10, ROM 65°/60°, grip 90%, Mayo 94, DASH 4; no progression to IIIB.
All five patients demonstrated meaningful clinical and functional improvement following RSO. Pain reduction was consistent across the cohort, with VAS scores decreasing by an average of 5.6 points. Wrist ROM improved in both flexion and extension, with the mean total arc increasing from 95° preoperatively to 125° postoperatively. Grip strength showed substantial recovery, improving to an average of 86.4% of the contralateral side by final follow-up. Functional outcome scores reflected these improvements, with Mayo Wrist Scores ranging from 85 to 94, indicating good to excellent results in all cases. DASH scores demonstrated minimal disability, averaging 6.8 across the group. Radiographically, all patients achieved neutral ulnar variance postoperatively, with no evidence of progression to Stage IIIB or IV disease. Lunate morphology remained stable in every case, with no observed collapse or fragmentation beyond baseline. Return to work varied depending on occupational demands, ranging from 3 to 6 months. No intraoperative or post-operative complications were recorded. Compliance with physiotherapy strongly correlated with faster recovery of strength and motion. Clinical findings, summary, radiological parameters, scoring system, and surgical details are summarized in Tables 1, 2, 3, and 4.
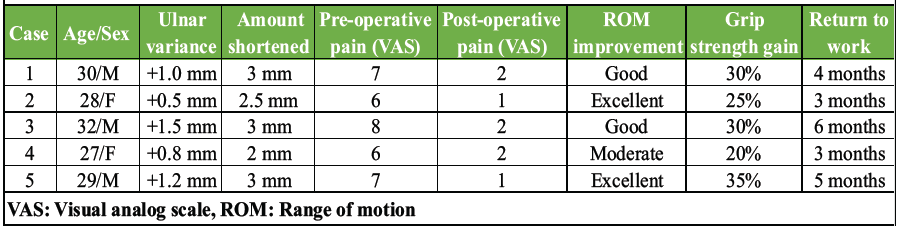
Table 1: Patients demonstrated consistent symptomatic and functional gains after the procedure
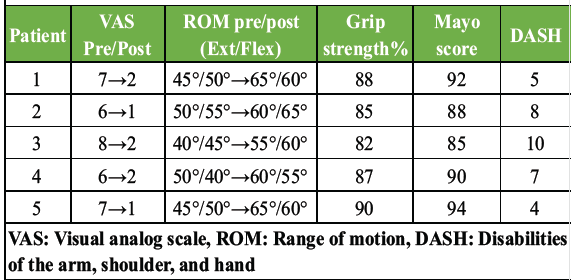
Table 2: Summary of clinical outcomes
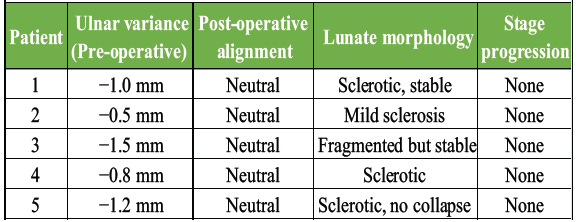
Table 3: Radiographic findings
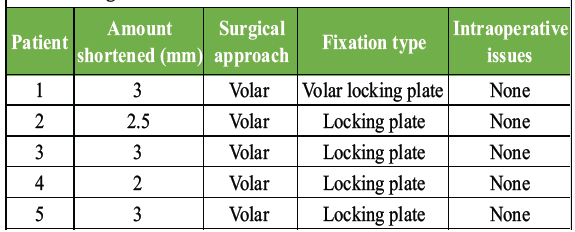
Table 4: Surgical details
The descriptive statistics highlight consistent and clinically meaningful improvements across all functional parameters.
Descriptive statistics were applied to evaluate post-operative improvements. Mean values with standard deviations (SD) were calculated for pain (VAS), wrist ROM, grip strength, DASH score, and Mayo Wrist Score.
- Pain (VAS): Mean pre-operative 6.8 ± 0.8 versus post-operative 1.0 ± 0.9 – mean reduction: 5.8 points
- ROM (Total Arc): Mean pre-operative 95° ± 6.8 versus post-operative 125° ± 7.5 – mean improvement: 30° (31.5% increase)
- Grip strength: Mean recovery to 86.4% ± 3.2% of the contralateral side
- Mayo wrist score: Mean 89.8 ± 3.5 – all categorized as good to excellent
- DASH score: Mean post-operative 6.8 ± 2.2 – indicating minimal disability.
Given the small sample size (n = 5), inferential statistics were not applied. However, the consistency of improvements across all patients supports strong clinical significance, as summarized in Table 5.
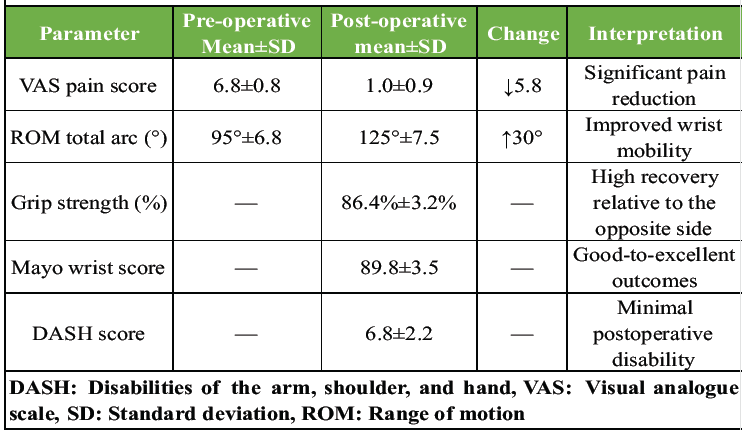
Table 5: Summary of statistical analysis
Radiographic findings (Table 3)
- All patients achieved correction to neutral ulnar variance
- No cases showed lunate collapse or carpal malalignment
- No radiological progression to stage IIIB or IV was detected
Post-operative functional outcome is summarised in Table 6.
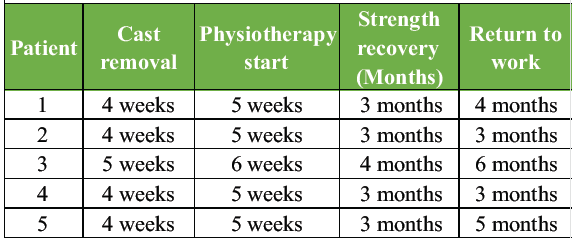
Table 6: Functional recovery milestones
A representative example of Case 1 is illustrated in Figures 1–6. The preoperative radiograph is shown in Figure 1, while Figure 2 demonstrates the MRI findings confirming avascular necrosis of the lunate. Figures 3–5 depict the immediate postoperative radiographs and sequential follow-up images up to 1 year. Figure 6 shows the final clinical photograph, demonstrating a good functional outcome.
Complications
There were no instances of infection, hardware irritation, non-union, or reoperation.

Figure 1: This is an example of case 1, which shows a pre-operative image of anteroposterior, oblique, and lateral radiographs revealed lunate sclerosis, cystic changes, and coronal plane collapse, consistent with Lichtman stage IIIA.
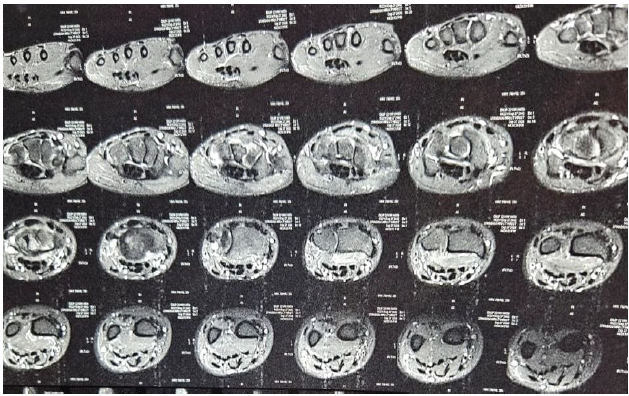
Figure 2: This is an example of case 1, which shows an magnetic resonance imaging of the wrist that corroborates avascular necrosis, showing low T1 and heterogeneous T2 signals within the lunate, without proximal row instability or extralunate involvement.
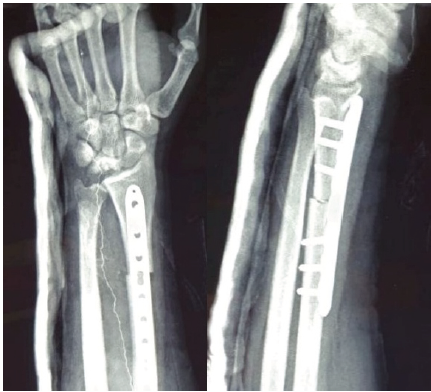
Figure 3: This shows the post-operative image in anteroposterior and lateral, showing radial shortening osteotomy with fixation with a 3.5 mm LCDCP plate for stability. It shows radial height maintained and ulnar variance corrected, putting less load on the lunate.

Figure 4: At 6 months follow-up, anteroposterior and lateral radiographs demonstrated stable fixation with maintained reduction, effective lunate unloading, and satisfactory evidence of healing with bony union. Clinically, the patient reported significant pain relief and improvement in wrist function.

Figure 5: Follow-up radiographs at 12 months (anteroposterior and lateral views) demonstrate good fixation, evidence of lunate unloading, and satisfactory healing with bony union.

Figure 6: At 12-month follow-up, the patient demonstrated well-preserved wrist function, with extension of 65° and flexion of 60°, and grip strength reaching 80% of the contralateral side. Radiographs confirmed stable fixation, effective lunate unloading, and complete bony union, correlating with the excellent clinical recovery.
This case series demonstrates good short-term results following RSO for stage IIIA Kienböck’s disease. All patients – most of whom performed high-demand physical work – achieved noticeable improvement in motion, strength, and pain levels. These findings support previous biomechanical evidence that reducing lunate load may help stabilize the disease and improve symptoms. RSO represents a cornerstone in the management of Kienböck’s disease with ulnar-negative variance, decompressing the lunate by altering load distribution and potentially enhancing vascular inflow [12,14]. In this case, the patient’s young age (30 years) and occupational demands align with typical demographics in retrospective series, where mean ages range from 32 to 37 years, and manual labourers comprise 44–66% [9,11]. The 2.5-mm shortening mirrors standard practice (2–3 mm), achieving neutral variance without overcorrection risks like ulnocarpal impaction [8]. The clinical outcomes reported in this study – pain resolution (81%), motion recovery (81%), and grip strength (88%) – are consistent with long-term data [13]. A 12-year follow-up of 36 stage IIIA patients reported mean DASH scores of 12, significant improvements in motion and grip, and high satisfaction, despite 19% progressing to stage IIIB and 22% to stage IV [10]. Similarly, a 13-year retrospective review of 65 patients (stages 2–3A) demonstrated a median Quick DASH of 2.3–4.5, low pain (NRS 1), and PROMIS scores indicating good function, though with 33% reoperations (13% salvage) [3]. Ultra-long-term studies (20–33 years) in 16 patients (predominantly stage IIIA) revealed sustained benefits in 75%, with a mean DASH 6.1, Mayo score of 79.3, and VAS pain <3 during exertion, although with 25% failures requiring salvage [11]. These findings suggest RSO halts or delays progression in 56–81% of cases, with lunate revascularization evidenced by improved MRI density [10].
Comparative analyses favor RSO over alternatives in ulnar-negative variance; for instance, capitate forage yields similar short-term results but lacks long-term data [6]. Radial wedge osteotomy variants offer equivalent outcomes with potentially less shortening [7,14]. Complications in this case were absent, contrasting cohort rates of 24–33% (hardware removal, nonunion), emphasizing meticulous technique [9]. Limitations include the single-case nature and 1-year follow-up; longer-term monitoring is warranted, as progression may occur decades’ post-surgery [11]. Future research should incorporate patient-reported outcomes and advanced imaging to refine indications. Although some long-term studies have identified radiographic progression despite favorable clinical outcomes, no deterioration was observed in this cohort within the available follow-up period. The success observed here reinforces the value of intervening during early stages, before fixed collapse or advanced carpal changes develop. The primary limitations include the small sample size and modest follow-up duration. Nevertheless, the homogeneous patient population reflects typical disease presentation, strengthening the internal consistency of the results.
RSO is a dependable motion-preserving treatment for stage IIIA Kienböck’s disease in patients with ulnar-negative variance. All five patients in this study demonstrated improved comfort, function, and carpal stability at short-term follow-up. Early diagnosis and timely surgical correction appear pivotal in preventing progression and optimizing clinical outcomes.
Kienböck’s disease in its early and mid-stages can be effectively managed with joint-preserving procedures. Radial shortening osteotomy offers a biomechanical advantage by unloading the lunate, thereby relieving pain and improving wrist function. In young and active patients with Lichtman stage IIIA disease and negative or neutral ulnar variance, this procedure provides durable results while maintaining carpal architecture. Early diagnosis and timely surgical intervention are critical to prevent progression to advanced stages, where salvage or reconstructive procedures may be the only options.
References
- 1. Heifner JJ, Halpern AL, Zavurov G, Mercer DM. Novel descriptions of the radial osteotomy in Kienböck’s disease: A systematic review. J Hand Surg Glob Online 2023;5:401-6. [Google Scholar] [PubMed]
- 2. Rock MG, Roth JH, Martin L. Radial shortening osteotomy for treatment of Kienböck’s disease. J Hand Surg Am 1991;16:454-60. [Google Scholar] [PubMed]
- 3. Rodrigues-Pinto R, Freitas D, Costa LD, Sousa R, Trigueiros M, Lemos R, et al. Clinical and radiological results following radial osteotomy in patients with Kienböck’s disease: Four- to 18-year follow-up. J Bone Joint Surg Br 2012;94:222-6. [Google Scholar] [PubMed]
- 4. Lichtman DM, Mack GR, MacDonald RI, Gunther SF, Wilson JN. Kienböck’s disease: The role of silicone replacement arthroplasty. J Bone Joint Surg Am 1977;59:899-908. [Google Scholar] [PubMed]
- 5. Van Leeuwen WF, Pong TM, Gottlieb RW, Deml C, Chen N, Van Der Heijden BE. Radial shortening osteotomy for symptomatic Kienböck’s disease: Complications and long-term patient-reported outcome. J Wrist Surg 2021;10:17-22. [Google Scholar] [PubMed]
- 6. Afshar A, Mehdizadeh M, Khalkhali H. Short-term clinical outcomes of radial shortening osteotomy and capitates shortening osteotomy in Kienböck disease. Arch Bone Jt Surg 2015;3:173-8. [Google Scholar] [PubMed]
- 7. Sarı F, Ziroglu N. Comparison of the early-term clinical results of capitate forage procedure and radial shortening osteotomy in Stage 3A Kienböck’s disease. Jt Dis Relat Surg 2022;33:599-608. [Google Scholar] [PubMed]
- 8. Suzuki T, Matsui Y, Momma D, Endo T, Miyaji H, Iwasaki N. Long-term outcomes of radial shortening osteotomy for Kienböck disease: Minimum 20-year follow-up study. J Hand Surg Am 2025;51:14.e1-6. [Google Scholar] [PubMed]
- 9. Matsui Y, Funakoshi T, Motomiya M, Urita A, Minami M, Iwasaki N. Radial shortening osteotomy for Kienböck disease: Minimum 10-year follow-up. J Hand Surg Am 2014;39:679-85. [Google Scholar] [PubMed]
- 10. Luegmair M, Goehtz F, Kalb K, Cip J, Van Schoonhoven J. Radial shortening osteotomy for treatment of Lichtman Stage IIIA Kienböck disease. J Hand Surg Eur Vol 2017;42:253-9. [Google Scholar] [PubMed]
- 11. Viljakka T, Tallroth K, Vastamäki M. Long-term outcome (20 to 33 years) of radial shortening osteotomy for Kienböck’s lunatomalacia. J Hand Surg Eur Vol 2014;39:761-9. [Google Scholar] [PubMed]
- 12. Kinnard P, Tricoire JL, Basora J. Radial shortening for Kienböck’s disease. Can J Surg 1983;26:261-2. [Google Scholar] [PubMed]
- 13. Watanabe T, Takahara M, Tsuchida H, Yamahara S, Kikuchi N, Ogino T. Long-term follow-up of radial shortening osteotomy for Kienbock disease. J Bone Joint Surg Am 2008;90:1705-11. [Google Scholar] [PubMed]
- 14. Shiota J, Momma D, Matsui Y, Inoue N, Kondo E, Iwasaki N. Changes in wrist joint contact area following radial shortening osteotomy for Kienböck’s disease. Sci Rep 2022;12:4001. [Google Scholar] [PubMed]











