Although rare, fungal infection in a native joint is a possibility.
Dr. Vikram Venkatesh Raykar, Department of Orthopaedics, Star Hospital, Nanakramguda, Hyderabad, Telangana, India. E-mail: vikramraykar007@gmail.com
Introduction: Fungal infections of native joints are exceedingly rare and often present with non-specific symptoms, making diagnosis challenging. Hip involvement is particularly uncommon and may mimic tuberculosis or bacterial septic arthritis. Patients on long-term hemodialysis are at increased risk due to their immunocompromised state and repeated vascular access.
Case Report: We present the case of a 52-year-old male with chronic kidney disease on maintenance hemodialysis for 5 years, who developed progressive left hip pain and functional limitation over 18 months. Radiological evaluation revealed destructive arthritis. He underwent a two-stage procedure: Initial debridement with insertion of an antibiotic cement spacer, during which intra-operative cultures yielded Candida guilliermondii. The patient received six weeks of intravenous Caspofungin. After normalisation of inflammatory markers, a second-stage total hip replacement was performed. Post-operatively, the patient achieved independent ambulation with significant pain relief and improved hip function.
Conclusion: Candida guilliermondii infection of the native hip in dialysis-dependent patients is exceptionally rare [6, 7, 8]. Early diagnosis with culture confirmation, followed by antifungal therapy and staged surgical management, is critical for optimal functional recovery.
Keywords: Fungal arthritis, native hip infection, Candida guilliermondii, hemodialysis, total hip replacement.
Fungal arthritis of native joints is an uncommon clinical entity, representing <1% of all septic arthritis cases [1]. Hip joint involvement is particularly rare and frequently misdiagnosed as bacterial septic arthritis or tuberculosis, especially in endemic regions [2,3,4,5,6]. Patients with chronic kidney disease (CKD) on long-term hemodialysis are predisposed to opportunistic infections due to immunosuppression, vascular access, and repeated interventions [3,4,7]. Prompt recognition and targeted management are essential to prevent progressive joint destruction and disability.
A 52-year-old male with CKD on maintenance hemodialysis for 5 years presented with gradually worsening left hip pain and reduced mobility over 18 months. Clinical examination revealed painful restriction of motion. Radiograph (Fig. 1) and magnetic resonance imaging showed advanced destructive arthritis of the hip. A two-stage surgical procedure was planned. In stage one (Fig.2), thorough debridement was performed, and an antibiotic-impregnated cement spacer was placed (Fig.3). Intra-operative tissue cultures grew Candida guilliermondii. The patient was treated with intravenous Caspofungin for six weeks, after which inflammatory markers normalised.

Figure 1: Pre-operative Radiograph demonstrating advanced destructive arthritis of left hip
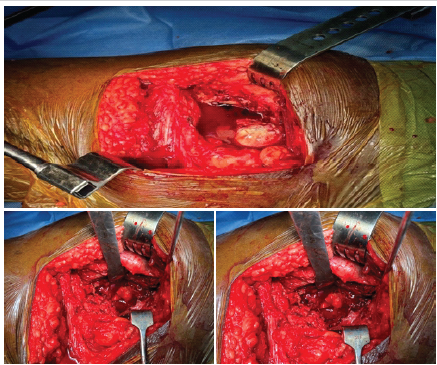
Figure 2: Intra-operative pictures showing significant synovitis and effusion
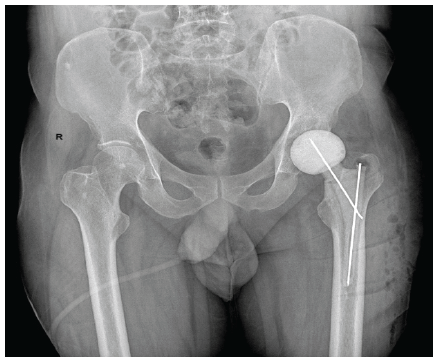
Figure 3: Post-operative radiograph following stage-1 surgery demonstrating antibiotic cement spacer.
Stage two involved total hip replacement (Fig.4). The post-operative course was uneventful. At 12 months follow-up, the patient reported marked pain relief, improved range of motion, and independent ambulation.
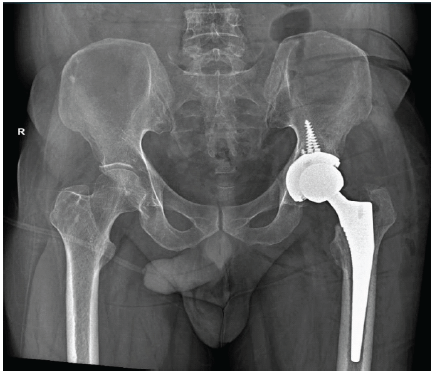
Figure 4: Post-operative radiograph following stage 2 surgery showing well aligned THR.
Fungal arthritis accounts for a very small fraction of native joint infections [1,2]. Candida species are more commonly implicated in prosthetic joint infections than native joints [6,8]. Candida guilliermondii is a rare pathogen but has been reported in immunocompromised hosts, especially in those with CKD and on dialysis [7,9]. Diagnosis requires a high index of suspicion, as symptoms are often non-specific and may mimic bacterial or tubercular arthritis [2,10]. Imaging findings are inconclusive; culture of joint fluid or intraoperative tissue remains the gold standard [11]. Treatment typically involves a combination of surgical debridement and systemic antifungal therapy [8,12]. Staged surgical management, as in this case, ensures eradication of infection while enabling subsequent joint reconstruction. Two-stage revision arthroplasty has been reported with favourable outcomes in Candida prosthetic joint infections [6,12].
Native hip joint infection due to Candida guilliermondii is exceptionally rare, particularly in dialysis-dependent patients. This case highlights the importance of early suspicion, culture-based diagnosis, prolonged antifungal therapy, and staged surgical management for achieving favourable outcomes.
This case highlights
- To have a high index of suspicion of subacute/chronic infection ( Fungal / Koch’s) with atypical clinical and radiological presentation in immunocompromised patient.
- The importance of tissue culture to rule out fungal / tubercular / bacterial infection, especially in immunocompromised patient.
References
- 1. De Meo F, F, Cera G, Ceccarelli G, Castagna V, Aronica R, Pieracci EM, Persiani P, Villani C. e Candida fracture-related infection: A systematic review. J Bone Jt Infect 2021;6:321-28. [Google Scholar] [PubMed]
- 2. Lee SJ, Kim ES, Eoh W, Lee SJ. Primary Candida guilliermondii infection of the knee in a patient without predisposing factors. Case Rep Orthop. 2012;2012:375682. [Google Scholar] [PubMed]
- 3. Hachem R, Raad I, Jiang Y, Abikaram G, Rolston KVI. High rate of Candida deep-seated infection in patients under chronic hemodialysis with extended central venous catheter use. Nephrol Dial Transplant 2016;31:503-10. [Google Scholar] [PubMed]
- 4. Klevens RM, Edwards JR, Andriole VT. Candida bloodstream infections in hemodialysis recipients. Emerg Infect Dis 2008;14:41-7. [Google Scholar] [PubMed]
- 5. Mastroianni CM, Paoletti F, D’Antonio D, Casciani C, Luzzi S, Scognamiglio P. Candida guilliermondii peritonitis during peritoneal dialysis. Clin Microbiol Infect 1999;5:634-6. [Google Scholar] [PubMed]
- 6. Cho CT, Kim DH, Lee SY, Choi NT. Periprosthetic knee inf ec tion by Mycobac terium bov is and Candida guilliermondii: A case report and literature review. J Med Case Rep 2019;13:57. [Google Scholar] [PubMed]
- 7. Pasqualotto AC, Denning DW, Gugelmin MCA, Freitas ETL. Candida guilliermondii as the aetiology of candidosis: Epidemiology, antifungal resistance and treatment. Rev Inst Med Trop Sao Paulo 2005;47:239-46. [Google Scholar] [PubMed]
- 8. Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA,Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, Zaoutis TE, Sobel JD. et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin Infect Dis.2016;62:e1-50. [Google Scholar] [PubMed]
- 9. Nakazawa Y, Saito I, Takahashi T, Ueda Y. Breakthrough Candida guilliermondii fungemia during azole prophylaxis after cord blood transplantation. Transpl Infect Dis 2017;19:e12738. [Google Scholar] [PubMed]
- 10. Tattevin P, Crickx E, Le Moal G, Bouvet E, Hofman P. Candida arthritis: Analysis of 30 cases and review of the literature. Medicine (Baltimore) 2004;83:313-22. [Google Scholar] [PubMed]
- 11. Chen CY, Lin CH, Wang SC, Chang YC, Chou CH. Fungal arthritis with adjacent osteomyelitis caused by Candida pelliculosa. BMC Infect Dis 2020;20:389. [Google Scholar] [PubMed]
- 12. Azzam KA, Gitelis S, Gitelis A, Kass L, McAlister VC, Sculco TP, Hanssen AD. Outcome of a two-stage reimplantation protocol for Candida prosthetic joint infection: A systematic review. J Arthroplasty 2009;24:1011-6. [Google Scholar] [PubMed]









