Pediatric tibial plateau fracture-dislocations, although rare, demand urgent neurovascular evaluation, stable fixation, and long-term follow-up due to high risk of growth disturbances.
Dr. Brian D Rust, Department of Orthopaedic Surgery, Washington University School of Medicine, 660 South Euclid Avenue, Saint Louis, Missouri 63110, United States. E-mail: rust@wustl.edu
Introduction: Pediatric tibial plateau fracture-dislocations are extremely rare but can involve serious neurovascular and growth complications, requiring prompt evaluation, appropriate fixation, and long-term monitoring. This is the first case report of a tibial plateau fracture-dislocation in the pediatric population.
Case Report: A 13-year-old male fell off a motorized scooter, sustaining a tibial plateau fracture-dislocation. He underwent urgent reduction and application of external fixator with subsequent extraphyseal fixation. He had an excellent outcome at both 1-year and 5-year follow-up.
Conclusion: This unusual injury pattern requires thoughtful and comprehensive evaluation, followed by appropriately timed open reduction and stable internal fixation to allow for the early joint range of motion and optimized function. The management of this case serves as an example of how to best approach a rare injury such as this. Patients should be followed until skeletal maturity for potential leg-length discrepancy or malalignment.
Keywords: Pediatric, tibial plateau, fracture-dislocation.
Pediatric fractures about the knee are most commonly physeal or avulsion-type injuries. Epiphyseal injuries of the proximal tibia make up only 0.8–3.1% of all epiphyseal injuries [1]. These injuries occur secondary to high-energy trauma with significant varus, valgus, or hyperextension force. There have been no prior reports of pediatric proximal tibia fracture-dislocations. In 1981, Moore described five types of proximal tibia fracture-dislocations occurring in adults. There should be a high suspicion for ligamentous instability and neurovascular injury in patients with these injuries [2]. When evaluating the rare pediatric patient with a knee fracture-dislocation, there should be an equally high index of suspicion and thorough assessment for neurovascular and soft-tissue injury.
The patient is a 13-year-old male with no significant medical history who sustained a fall off a motorized scooter resulting in a right tibial plateau fracture and ipsilateral radial head fracture. On examination of his right lower extremity, his leg compartments were swollen but compressible. His motor and sensory function were grossly intact distally. Ankle-brachial index (ABI) was 0.92 and he had palpable pulses. X-rays demonstrated a Schatzker IV/Moore type 2 bicolumnar tibial plateau fracture-dislocation (Fig. 1).
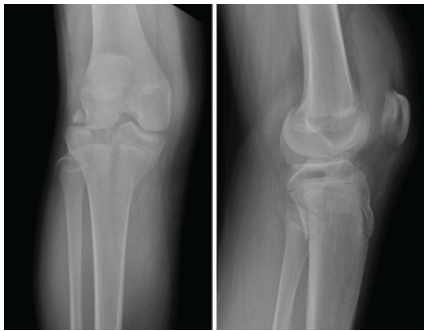
Figure 1: Anteroposterior and lateral X-ray images demonstrating a Schatzker IV/Moore type 2 bicolumnar tibial plateau fracture-dislocation.
The patient was taken urgently to the operating room for closed reduction and application of an external fixator. A computed tomography (CT) scan was obtained after external fixation (Fig. 2); this demonstrated a Salter Harris type 4 pattern of the medial tibial condyle with widely displaced articular fragments of the lateral tibial plateau.
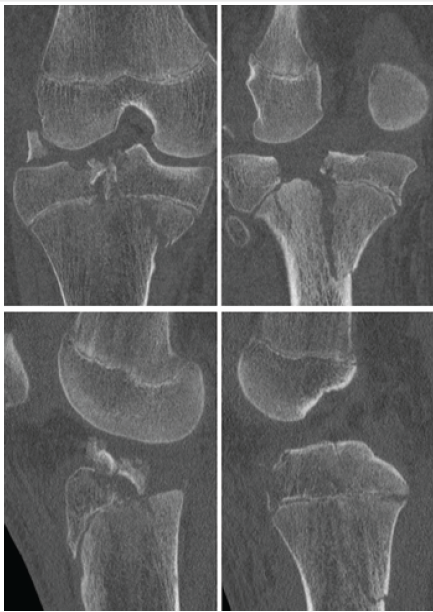
Figure 2: Select computed tomography scan cuts demonstrating Schatzker IV/Moore 2 tibial plateau fracture and large intra-articular fracture fragment.
The patient was closely monitored postoperatively and discharged home on post-injury day 1.
On post-injury day 8, the patient returned for removal of external fixator and definitive fixation. The medial side was addressed first through a posteromedial approach. After direct open reduction, a small fragment plate was used to buttress the medial condyle with all fixation performed distal to the physis. Attention was then turned to the lateral side where a standard anterolateral approach was made, centered over Gerdy’s tubercle. A femoral distractor was applied for lateral joint visualization and a submeniscal arthrotomy was performed. The flipped articular fragment was noted to be trapped between the femur and the tibia. When this piece was rotated anteriorly, the torn lateral meniscus was revealed and noted to be impacted into the tibial metaphysis. The articular fragment was reduced and held with Steinmann pins. A minifragment plate was then contoured as a rim plate and screws were inserted to raft and secure the articular fragment as well as the medial epiphysis. All lateral fixation was proximal to the physis (Fig. 3). The lateral meniscus was then repaired using an all-inside device posteriorly and open repair to the lateral plate for the remainder of the body. Following fixation, the knee was ligamentously stable on examination.
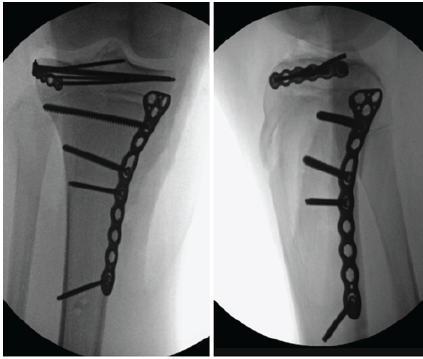
Figure 3: Final intraoperative fluoroscopic images following fixation: All lateral fixation was kept proximal to the physis and all medial fixation distal to the physis.
The patient was kept non-weight-bearing for 12 weeks postoperatively with instructions to work on knee range of motion. At 6 weeks post-operative, his range of motion was 15–90° and he was instructed to begin physical therapy. At 4 months post-operative, his range of motion was 5–120° and he was ambulating with a limp. At 7 months post-operative, both his range of motion and strength were full and symmetric to the contralateral side at 0–130°. He was asymptomatic and had returned to all desired activities, including gym class. X-rays demonstrated a healed fracture with well-maintained alignment and premature closure of the proximal tibial physis. There was no evidence of length-length or sagittal plane growth discrepancy (Fig. 4).
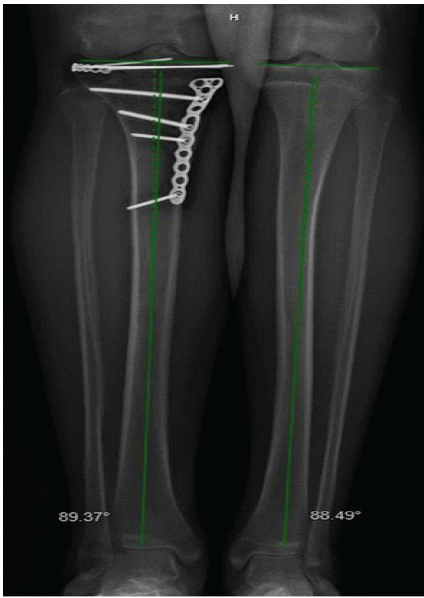
Figure 4: Lower extremity alignment films at 7 months post-operative demonstrating no significant asymmetry.
At 1 year post-operative, he continued to participate in all desired activities without pain or limp. Knee range of motion and strength remained full and symmetric. X-rays of the knee demonstrated maintained fixation, and lower extremity alignment films demonstrated mild valgus relative to the contralateral side (Fig. 5), although this was not clinically apparent.
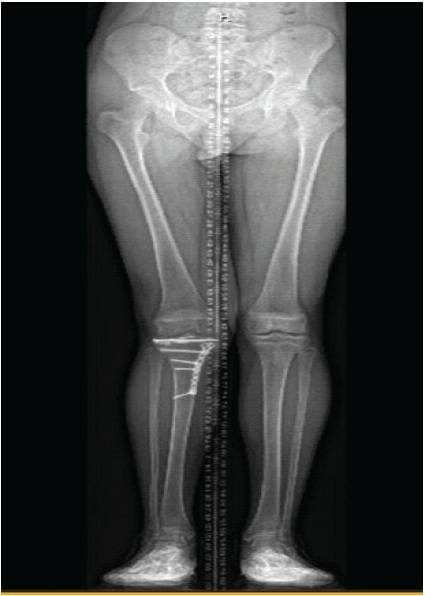
Figure 5: Lower extremity alignment films at 1 year post-operative demonstrating mild valgus deformity relative to the contralateral lower extremity.
At 5 years post-operative, he continued to have no limitations to his activities, and he remained free of any pain or mechanical symptoms. In fact, he has become active in triathlons and competitive distance running. X-rays at this time showed completely healed fractures, intact hardware, and well-preserved joint spaces with continued mild genu valgum on the right (Fig. 6). Knee range of motion has remained full, and leg length and muscle bulk remain symmetrical bilaterally (Fig. 7).
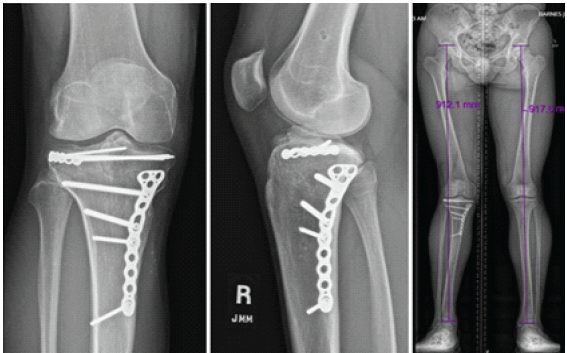
Figure 6: Five years post-operative X-ray images demonstrating well-maintained alignment, fixation, and joint congruity.

Figure 7: Full range of motion and bilateral symmetry demonstrated at 5 years post-operative.
High-energy tibial plateau fractures, including fracture-dislocations, have been shown to have a higher incidence of popliteal artery and peroneal nerve injuries. In adult patients with knee dislocation, the incidence of vascular injury may be up to 16% based on five retrospective studies [3]. While pediatric tibial plateau fracture-dislocations have not been previously reported, Burkhart reported neurologic and vascular injuries in 14% of proximal tibia epiphyseal fractures [4]. Pediatric tibial plateau fracture-dislocations should be evaluated as urgently and thoroughly as knee fracture-dislocations in the adult population. Detailed evaluation must include pulse exam, ABI, neurologic examination, and compartment checks [5,6,7,8]. Following comprehensive examination, urgent reduction should take priority, with the addition of external fixation if the extremity is too swollen for acute definitive fixation. Further assessment should then include detailed evaluation of bony and soft-tissue injuries with CT scan and/or magnetic resonance imaging. Prior series have shown 71–77% incidence of ligament rupture and 49–91% incidence of meniscal injury in patients with operative tibial plateau fractures [9,10]. Once the injury has been adequately defined, definitive fixation should be planned. Planning should include extraphyseal fixation methods, rigid internal fixation to provide absolute stability and allow for early range of motion, and awareness of strategies for management of associated soft-tissue injuries. Those not familiar with these treatment strategies should transfer to a facility with trauma-trained orthopedic surgeons for definitive care. As was true in this case, physeal arrest may occur despite physeal-sparing fixation methods. This is likely attributable to traumatic injury to the physis. A summary of six case series of pediatric proximal tibial fractures demonstrated a 45% incidence deformity, with a 25% incidence of posttraumatic growth deformities of >25 mm length or >5° of angulation [1]. Due to the high prevalence of post-traumatic deformity and leg length discrepancy, treating surgeons must be vigilant in monitoring these patients at least until skeletal maturity is reached. In this case, the patient’s function was excellent despite his resultant valgus deformity. Given no active symptoms and extremely high function, any interventions to correct his valgus alignment have been deferred but the patient was educated on possible long-term issues related to the lateral compartment of his knee.
This is the first reported case of a pediatric tibial plateau fracture-dislocation. Emphasis should be placed on neurovascular assessment and urgent reduction in the operating room. Advanced imaging should be considered for detailed assessment of bony and ligamentous injury and for preoperative planning. This is a rare clinical entity that requires stable internal fixation to allow for restoration of joint stability and early range of motion to optimize clinical outcomes. While fixation should remain extraphyseal if possible, there remains a high-risk for premature physeal closure and resultant leg-length discrepancy or malalignment. For this reason, patients should be followed at least until skeletal maturity and advised of this possible complication.
Pediatric tibial plateau fracture-dislocations are a rare injury. This case report will be the first contribution to the literature on how to manage such a case.
References
- 1. Gautier E, Ziran BH, Egger B, Slongo T, Jakob RP. Growth disturbances after injuries of the proximal tibial epiphysis. Arch Orthop Trauma Surg 1998;118:37-41. [Google Scholar] [PubMed]
- 2. Moore TM. Fracture–dislocation of the knee. Clin Orthop Relat Res 1981;156:128-40. [Google Scholar] [PubMed]
- 3. Miranda FE, Dennis JW, Veldenz HC, Dovgan PS, Frykberg ER. Confirmation of the safety and accuracy of physical examination in the evaluation of knee dislocation for injury of the popliteal artery: A prospective study. J Trauma 2002;52:247-51, discussion 251-2. [Google Scholar] [PubMed]
- 4. Burkhart SS, Peterson HA. Fractures of the proximal tibial epiphysis. J Bone Jt Surg Am 1979;61:996-1002. [Google Scholar] [PubMed]
- 5. Mayer S, Albright JC, Stoneback JW. Pediatric knee dislocations and physeal fractures about the knee. J Am Acad Orthop Surg 2015;23:571-80. [Google Scholar] [PubMed]
- 6. Bailey ME, Wei R, Bolton S, Richards RH. Paediatric injuries around the knee: Bony injuries. Injury 2020;51:611-9. [Google Scholar] [PubMed]
- 7. Halvorson J. Reduction techniques for young femoral neck fractures. J Orthop Trauma 2019;33:S12-9. [Google Scholar] [PubMed]
- 8. Levy BA, Zlowodzki MP, Graves M, Cole PA. Screening for extermity arterial injury with the arterial pressure index. Am J Emerg Med 2005;23:689-95. [Google Scholar] [PubMed]
- 9. Gardner MJ, Yacoubian S, Geller D, Suk M, Mintz D, Potter H, et al. The incidence of soft tissue injury in operative tibial plateau fractures: A magnetic resonance imaging analysis of 103 patients. J Orthop Trauma 2005;19:79-84. [Google Scholar] [PubMed]
- 10. Stannard JP, Lopez R, Volgas D. Soft tissue injury of the knee after tibial plateau fractures. J Knee Surg 2010;23:187-92. [Google Scholar] [PubMed]








