Irreducible periprosthetic hip dislocations may result from rare mechanical barriers such as muscular penetration of the femoral head and can be complicated by sciatic nerve involvement, requiring prompt surgical intervention.
Dr. Zachary Fuller, Department of Orthopedic Surgery, Rutgers New Jersey Medical School, Newark, NJ, USA. E-mail: zachary.fuller@rutgers.edu
Introduction: Periprosthetic dislocations remain a prevalent complication following total hip arthroplasty, with heightened risks in elderly patients and those with cognitive impairments. While most cases can be managed with closed reduction, irreducible dislocations are rare and may be due to unusual mechanical or soft-tissue impediments.
Case Report: This case report describes an 87-year-old woman with an irreducible prosthetic hip dislocation due to penetration of the femoral head through the gluteus medius musculature after a ground-level fall. After multiple failed closed reduction attempts, the patient developed a foot drop with sensory changes indicating a sciatic nerve palsy. Open reduction was then indicated, along with neurolysis of the sciatic nerve.
Conclusion: The case underscores the challenges of managing complex hip dislocations in older adults and highlights the importance of addressing mechanical and neurological factors during treatment.
Keywords: Periprosthetic hip dislocation, total hip arthroplasty, open reduction, sciatic nerve entrapment, irreducible, neurolysis.
Total hip arthroplasty (THA) is a highly effective surgical procedure commonly employed to alleviate pain and restore function in patients with advanced hip joint pathology [1,2,3]. Despite its success, complications such as prosthetic dislocations remain a significant concern, with reported rates ranging from 1% to 5% [4,5,6,7]. Factors contributing to dislocation include malpositioning of components, soft tissue laxity, surgical approach, and prosthetic design [4,5,6,7]. While many of these cases can be successfully treated with closed reduction techniques, irreducible dislocations are rare but challenging scenarios that may require advanced interventions. Irreducible dislocations often result from unusual causes, including dissociation of modular components, interposition of soft tissues, or entrapment of surrounding anatomical structures [8,9,10,11]. In addition, sciatic nerve complications, although rare, are critical to recognize given their potential to cause significant neurological deficits, including foot drop and sensory changes [12,13]. The author reports a case of an irreducible prosthetic hip dislocation due to femoral head/neck penetration through abductors with concomitant foot drop following closed reduction attempts.
An 87-year-old female with a medical history of dementia, hypertension, and hyperlipidemia underwent a left THA through a posterior approach in 2010. She presented to the emergency department following a ground-level fall, reporting severe left hip pain and an inability to bear weight. Imaging confirmed a left periprosthetic hip dislocation (Fig. 1).
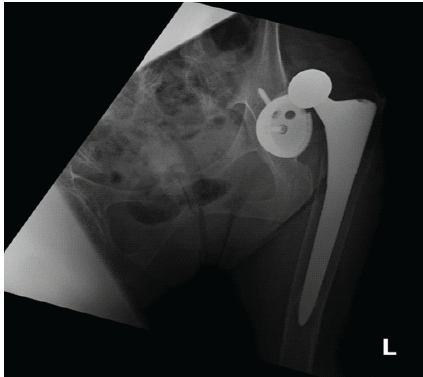
Figure 1: Pre-reduction X-ray of left hip.
Initial attempts at closed reduction with conscious sedation in the emergency department failed. A subsequent closed reduction attempt under general anesthesia in the operating room was also unsuccessful. Postoperatively, the patient developed numbness on the dorsum of her left foot and was unable to dorsiflex, raising concerns for sciatic nerve involvement.
Given the failed reductions and the development of neurological deficits, the decision was made to proceed with an open reduction. During the procedure, it was found that the femoral head had penetrated through the gluteus medius muscle, impeding reduction (Fig. 2). In addition, the sciatic nerve was abutting the posterior acetabulum and was entrapped in scar tissue (Fig. 3).

Figure 2: Clinical photograph during open reduction with the head violating the abductors.

Figure 3: Clinical photograph during open reduction showing scarred sciatic nerve abutment against the posterior margin of the cup.
Neurolysis was performed to release the sciatic nerve, and the femoral head was carefully disengaged from the muscle. The acetabular and femoral prosthetic components were assessed and deemed to be stable and thus were left in position. The femoral head size was increased from +4 to +8 (32 mm head) to enhance stability (Figs. 4 and 5).
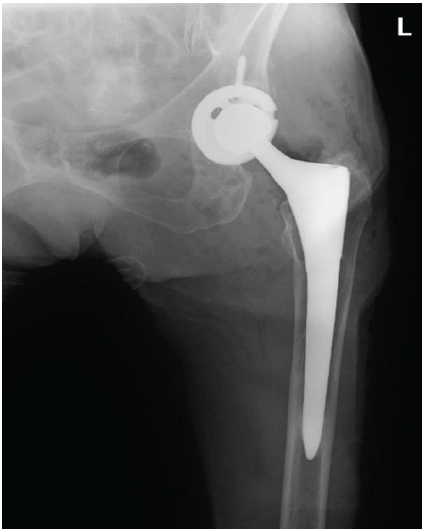
Figure 4: Post-reduction X-ray of left hip.
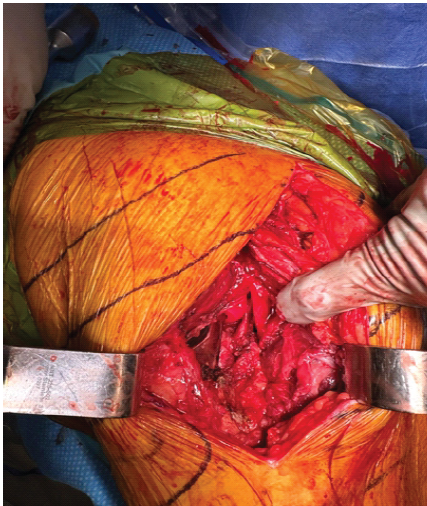
Figure 5: Clinical photograph during open reduction of tension-free sciatic nerve status post-neurolysis.
Postoperatively, the patient showed partial improvement in foot sensation, though dorsiflexion remained weak. She was discharged to a subacute rehabilitation facility on post-operative day 3. At the 2-week follow-up, she continued to exhibit incomplete recovery of motor and sensory function.
On post-operative day 22, during a physical therapy session, the patient experienced a repeat left hip dislocation, confirmed by imaging. This dislocation was successfully reduced through a closed procedure without complications.
At her 3-month post-operative visit, she remained well located, had regained dorsiflexion of her foot, and was ambulatory without assistive devices.
This case illustrates several critical challenges in managing periprosthetic dislocations. The perforation of the femoral head through the gluteus medius is a rare mechanical impediment to reduction but should be suspected when numerous attempts have failed. In addition, sciatic nerve entrapment, likely due to scarring, compounded the difficulty in achieving a closed reduction and provided additional challenges in the post-operative period. Irreducible dislocations, though rare, present unique clinical difficulties. Previous literature states failed closed reductions could be due to entrapment of the iliopsoas tendon, interposition of the joint capsule, cement fragments, or other third-body elements [4,8,9,10,11]. Non-concentric reductions during attempts at closed reduction should alert the surgeon to the possibility of such interpositions necessitating open reductions. In addition, sciatic nerve complications – though with a prevalence of <0.1% – can occur, further complicating management [14]. Due to the proximity of the sciatic nerve to the posterior hip structures places it at risk of tension or compression injury during reduction maneuvers [13,14]. Cases of sciatic nerve entrapment around the femoral stem following closed reduction have been documented but are very limited in the literature [12,13,14,15,16,17]. When sciatic nerve palsy occurs post-reduction, immediate surgical exploration and neurolysis may be warranted to prevent permanent motor deficits [12]. This underscores the importance of limiting forceful reduction attempts and performing neurovascular assessments following manipulative efforts. It is recommended to monitor partial and secondary nerve injuries with an initial observation period of four to 6 months, as spontaneous recovery occurs in 70–100% of cases [14].
This case emphasizes the importance of considering mechanical, muscular, and neurological factors in periprosthetic dislocations. Surgical intervention must address not only the reduction of the prosthesis but also the surrounding soft tissue and nerve involvement. Further studies are needed to explore optimal strategies for preventing recurrent dislocations and improving neurological outcomes in this high-risk population.
In elderly patients with failed closed reductions after hip arthroplasty, consider open reduction to address both mechanical interposition and potential sciatic nerve entrapment to prevent long-term deficits.
References
- 1. Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 2018;100:1455-60. [Google Scholar] [PubMed]
- 2. Nuelle DG, Mann K. Minimal incision protocols for anesthesia, pain management, and physical therapy with standard incisions in hip and knee arthroplasties: The effect on early outcomes. J Arthroplasty 2007;22:20-5. [Google Scholar] [PubMed]
- 3. Stowers MD, Manuopangai L, Hill AG, Gray JR, Coleman B, Munro JT. Enhanced recovery after surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J Surg 2016;86:475-9. [Google Scholar] [PubMed]
- 4. Dawson-Amoah K, Raszewski J, Duplantier N, Waddell BS. Dislocation of the hip: A review of types, causes, and treatment. Ochsner J 2018;18:242-52. [Google Scholar] [PubMed]
- 5. Khan M, Della Valle CJ, Jacofsky DJ, Meneghini RM, Haddad FS. Early postoperative complications after total hip arthroplasty: Current strategies for prevention and treatment. Instr Course Lect 2015;64:337-46. [Google Scholar] [PubMed]
- 6. Brooks PJ. Dislocation following total hip replacement. Bone Joint J 2013;95-B:67-9. [Google Scholar] [PubMed]
- 7. D’Angelo F, Murena L, Zatti G, Cherubino P. The unstable total hip replacement. Indian J Orthop 2008;42:252-9. [Google Scholar] [PubMed]
- 8. Lim HF, Jain S, Haughton B, Veysi V, Shaw D. Irreducible dislocated total hip replacement due to intra-articular incarceration of bone cement: A case report. Int J Surg Case Rep 2014;5:1018-20. [Google Scholar] [PubMed]
- 9. Grigoris P, Grecula MJ, Amstutz HC. Dislocation of a total hip arthroplasty caused by iliopsoas tendon displacement. Clin Orthop Relat Res 1994;306:132-5. [Google Scholar] [PubMed]
- 10. Murphy EP, Fenelon C, Russell S, Condon F. Cause of irreducible dislocation of a re-revision THR. BMJ Case Rep 2018;2018:r-223072. [Google Scholar] [PubMed]
- 11. Pai VS. A rare cause of irreducible dislocation of a total hip prosthesis. J Arthroplasty 2003;18:208-10. [Google Scholar] [PubMed]
- 12. Cheung ZB, Patel AV, DeBellis N, Unis DB, Benitez CL. Sciatic nerve entanglement around a femoral prosthesis during closed reduction of a dislocated total hip prosthesis: The role of metal-suppression MRI. JBJS Case Connect 2018;8:e3. [Google Scholar] [PubMed]
- 13. Maeder B, Goetti P, Mahlouly J, Mustaki L, Buchegger T, Guyen O. Entrapment of the sciatic nerve over the femoral neck stem after closed reduction of a dislocated total hip arthroplasty. J Am Acad Orthop Surg Glob Res Rev 2019;3:e081. [Google Scholar] [PubMed]
- 14. Leversedge FJ, Gelberman RH, Clohisy JC. Entrapment of the sciatic nerve by the femoral neck following closed reduction of a hip prosthesis: A case report. J Bone Joint Surg Am 2002;84:1210-3. [Google Scholar] [PubMed]
- 15. van der Merwe JM. Sciatic nerve palsy after total hip arthroplasty. JBJS J Orthop Physician Assistants 2023;11:e23.00002. [Google Scholar] [PubMed]
- 16. Ng J, Marson BA, Broodryk A. Foot drop following closed reduction of a total hip replacement. BMJ Case Rep 2016;2016:bcr2016215010. [Google Scholar] [PubMed]
- 17. Stockley I, Bickerstaff D. Sciatic palsy following reduction of a dislocated prosthesis: brief report. J Bone Joint Surg Br 1988;70:329-30. [Google Scholar] [PubMed]











