Subtrochanteric stress fractures, though rare in low-risk premenopausal women, should be suspected in unexplained proximal thigh pain, as early MRI and timely conservative management can result in complete recovery without surgery.
Dr. Abhishek Singh, Department of Orthopaedics, Maharishi Markandeshwar Institute of Medical Sciences and Research, Ambala, Haryana, India. E-mail: avi2391994@gmail.com
Introduction: Subtrochanteric stress fractures are rare and often underdiagnosed due to their subtle clinical presentation and inconspicuous early radiological findings. While these fractures are frequently seen in elderly osteoporotic individuals or those on bisphosphonate therapy, they are uncommon in younger, premenopausal women without significant risk factors. This case highlights a rare instance of a non-displaced subtrochanteric stress fracture in a 45-year-old woman with osteopenia.
Case Report: A 45-year-old housewife presented with a progressively worsening, insidious pain in the anteromedial aspect of her left proximal thigh for the past month and a half. The pain, which worsened with activities, such as climbing stairs and squatting, was non-traumatic and unrelieved by rest. Initial radiographs showed no abnormalities, prompting a magnetic resonance imaging (MRI), which revealed a non-displaced subtrochanteric stress fracture with surrounding bone marrow edema. A DEXA scan confirmed osteopenia (T-score of −2.1 at the femoral neck), and laboratory tests were within normal limits.
Management and Outcome: Conservative management was initiated, including strict non-weight-bearing for 6–8 weeks, followed by partial weight-bearing, physiotherapy, and calcium and vitamin D supplementation. At 8 weeks, the patient reported significant pain relief and improved functional mobility. A follow-up MRI at 6 months demonstrated complete healing with no signs of delayed union or cortical disruption.
Conclusion: In this case, a non-displaced subtrochanteric stress fracture in a premenopausal woman without bisphosphonate use or antecedent trauma presented as unexplained proximal thigh pain with normal initial radiographs. MRI enabled early diagnosis, and conservative management with non-weight-bearing and metabolic optimization resulted in complete fracture healing without the need for surgical intervention.
Keywords: Subtrochanteric stress fracture, insufficiency fracture, magnetic resonance imaging, osteopenia, thigh pain, conservative management.
Stress fractures are classified broadly into fatigue fractures, which occur due to abnormal repetitive loading on normal bone, and insufficiency fractures, which arise from normal physiological stresses on weakened or osteoporotic bone [1]. Among these, stress fractures involving the femur are relatively rare and most commonly affect the neck of the femur or the shaft. Subtrochanteric stress fractures, located in the region just distal to the lesser trochanter, are particularly uncommon and often underdiagnosed due to their subtle clinical presentation and inconspicuous radiological findings during early stages [2]. These fractures are typically reported in elderly patients, especially postmenopausal women with osteoporosis, or those on long-term bisphosphonate therapy. Bisphosphonates, while beneficial in reducing fracture risk in osteoporotic patients, have been associated with the development of atypical femoral fractures, predominantly in the subtrochanteric region and femoral shaft [3]. In 2005, Goh et al. first reported the relationship between long-term alendronate therapy and low-energy subtrochanteric fractures [4]. Since then, multiple reports have confirmed this association, suggesting that prolonged suppression of bone turnover may result in microdamage accumulation and decreased bone remodeling, predisposing to stress fractures [5]. However, subtrochanteric stress fractures in younger, premenopausal individuals not on bisphosphonate therapy remain exceedingly rare. In such cases, insufficiency fractures may still occur in the setting of osteopenia, nutritional deficiencies, metabolic bone diseases, or repetitive microtrauma from occupational or lifestyle-related activities [6]. A recent study by Kim et al. described stress fractures of the subtrochanteric region in non-athletic, middle-aged women who had low bone mineral density but no history of anti-resorptive medication use, suggesting that even low-grade osteopenia may compromise bone integrity in specific anatomic regions subjected to high mechanical loading [7]. Clinically, these fractures may present with insidious onset of groin or thigh pain, often without any preceding trauma or acute event, making diagnosis difficult. Early radiographs are frequently negative, and the fracture may only become visible once cortical disruption or periosteal reaction becomes apparent after several weeks [8]. Magnetic resonance imaging (MRI) remains the most sensitive modality for early detection, showing marrow edema and a fracture line when X-rays are still normal [9]. This imaging sensitivity allows early diagnosis and conservative treatment before progression to a complete fracture. In this context, we report the case of a 45-year-old housewife with no history of trauma or bisphosphonate intake, who developed a non-displaced subtrochanteric stress fracture likely due to early-stage osteopenia, detected using MRI. This case emphasizes the need to maintain a high index of suspicion for such injuries, even in premenopausal women, and highlights the importance of MRI in evaluating unexplained thigh pain. To our knowledge, only a handful of such cases have been reported in the literature, and very few involving successful non-surgical management in this demographic.
A 45-year-old female, housewife by occupation, presented to the Orthopaedic outpatient department at MMIMSR, Mullana, with a chief complaint of pain in the anteromedial aspect of the left proximal thigh for the past 1½ months. The pain was insidious in onset, non-radiating, and gradually progressive. Initially, it was relieved with rest, but later became persistent and interfered with her daily household activities, particularly while climbing stairs, squatting, and rising from a seated position. She denied any history of fall, trauma, overexertion, or vigorous physical activity before the onset of symptoms. There were no systemic comorbidities, such as diabetes, thyroid dysfunction, or chronic steroid intake. Her menstrual history was regular, and she had not yet attained menopause. She reported no history of osteoporotic fractures, bisphosphonate or corticosteroid use, or any metabolic bone disorders. There was no family history of osteoporosis, malignancy, or other skeletal diseases. Her diet was vegetarian with suboptimal calcium intake, and she had no history of tobacco or alcohol consumption. Her routine as a housewife involved moderate physical activity, including frequent squatting and kneeling. On clinical examination, she walked with an antalgic gait, favoring the left lower limb. No visible swelling, deformity, or skin discoloration was noted. Localized tenderness was elicited over the anteromedial aspect of the proximal femur, just distal to the lesser trochanter. There was no warmth or erythema. Movements of the left hip were painful, particularly flexion and internal rotation. Limb lengths were equal, and distal neurovascular status was intact. Initial anteroposterior and lateral radiographs of the pelvis and left femur showed no abnormalities—no cortical discontinuity, periosteal reaction, or signs of bone pathology. However, due to the persistence of symptoms and worsening pain on activity, a pelvic MRI was ordered. MRI revealed a hypointense linear signal in the subtrochanteric region on T1-weighted images, along with hyperintense bone marrow edema in short tau inversion recovery and T2-weighted sequences (Fig. 1 and 2). A transverse fracture line was noted along the medial cortex, without displacement—consistent with an incomplete insufficiency stress fracture. There was no associated soft tissue mass or cortical thickening.
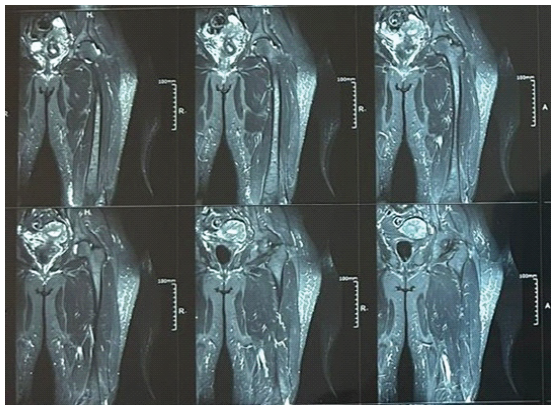
Figure 1: Magnetic resonance imaging of the left thigh showing focal cortical and periosteal thickening along the anteromedial aspect of the upper part of the femur.
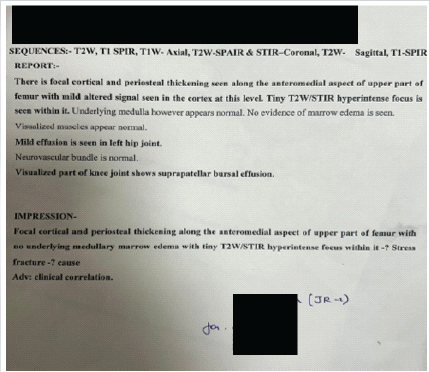
Figure 2: Magnetic resonance imaging (MRI) report of the above MRI.
A Dual-energy X-ray absorptiometry (DEXA) scan revealed osteopenia, with a T-score of −2.1 at the femoral neck and −1.9 at the lumbar spine (L1–L4). Serum calcium, phosphate, vitamin D3, parathyroid hormone, and renal function tests were within normal limits. Serum alkaline phosphatase was mildly elevated (168 U/L), suggesting active bone remodeling.
Given the stable nature of the fracture, absence of displacement, and good functional status, a conservative treatment approach was adopted. The patient was advised to maintain strict non-weight-bearing for 6–8 weeks, followed by partial weight-bearing ambulation with crutches. She was also prescribed calcium and vitamin D supplementation and advised on physiotherapy, activity modification, and nutritional optimization. At the 8-week follow-up, the patient reported significant improvement in pain and functional mobility. By 12 weeks, she had achieved pain-free full weight-bearing ambulation. At the 6-month follow-up, an MRI was repeated, which showed complete resolution of marrow edema and full consolidation at the fracture site, with no evidence of cortical disruption or delayed union [Fig. 3 and 4].
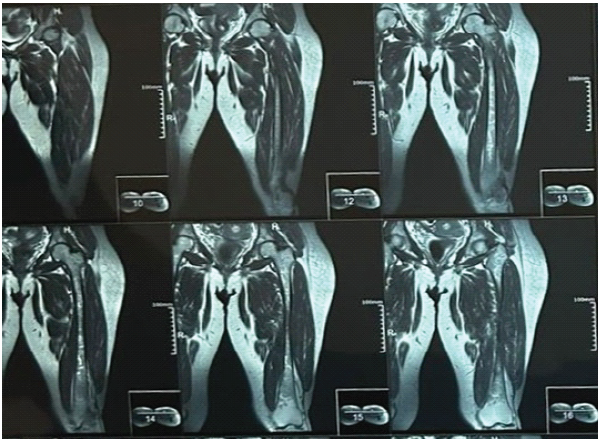
Figure 3: Magnetic resonance imaging done after 6 months of the treatment showing no changes in the upper part of the femur.
Figure 4: Magnetic resonance imaging report of the left thigh done after 6 months of the treatment.
This case underscores the effectiveness of early MRI in the diagnosis and successful conservative management of subtrochanteric stress fractures in low-risk, premenopausal women.
Stress fractures of the subtrochanteric femur are uncommon, particularly in patients without overt risk factors. Insufficiency fractures arise from normal physiological stress applied to bone weakened by conditions, such as osteoporosis or osteopenia, and are frequently observed in elderly women. While the prevalence of insufficiency fractures among women over 50 is notable, subtrochanteric locations remain rare, often under-recognized due to their subtle initial presentation [10]. Indeed, stress fractures in the proximal femur are among the least common, making prompt diagnosis especially challenging. “Bisphosphonate-associated insufficiency fractures” have gained attention in the literature, with long-term antiresorptive therapy implicated in atypical transverse subtrochanteric fractures. Goh et al. documented 13 cases, nine of whom were on alendronate, highlighting prodromal pain, lateral cortical beaking, and simple transverse fracture morphology as hallmark features of bisphosphonate-related fractures [4]. Similarly, Odvina et al. described severely suppressed bone turnover leading to microdamage accumulation and compromised fracture repair in long-term bisphosphonate users [3]. These fracture patterns differ from typical osteoporotic ones, which tend to be comminuted and involve trabecular bone. However, insufficiency fractures may also occur in the absence of bisphosphonate therapy. In patients with osteopenia, nutritional deficiencies, or hormonal imbalance, particularly middle-aged women, normal loading across the subtrochanteric cortex may result in microfractures and stress reactions [11]. In our case, the patient had mild osteopenia (T‑score −2.1) without any pharmacological predisposition, yet developed a non-displaced subtrochanteric fracture. This suggests that even low-grade bone mineral loss under repetitive household activity may precipitate such injuries. Early radiographs are often unremarkable in insufficiency fractures, with clear cortical changes or periosteal reaction visible only after a delay of weeks. In contrast, MRI is highly sensitive, detecting marrow edema in over 90% of fracture sites, and visualizing fracture lines not apparent on X-ray. As reported by Goh et al., MRI facilitated diagnosis before displacement occurred, allowing conservative management. Our case mirrors this pattern: Initial X-ray was equivocal, but MRI demonstrated a transverse fracture line and surrounding edema – criteria consistent with an incomplete stress fracture [4,12]. Management of a non-displaced insufficiency fracture depends on stability, displacement risk, and patient activity level. Many reports support non-operative treatment with protected weight-bearing, calcium and vitamin D supplementation, and observation, especially when the fracture is incomplete and stable [13]. Surgical fixation is reserved for displaced fractures or those occurring in patients with multiple risk factors. In patients on bisphosphonates, some authors recommend discontinuation of therapy and consider anabolic agents, such as teriparatide to aid healing and prevent progression [14]. Although our patient was not on antiresorptive therapy, she followed a similar conservative protocol—partial weight-bearing, bone nutrition optimization—and successfully healed without surgical intervention. This case is notable for presentation in a premenopausal, non-athletic, relatively healthy woman, without bisphosphonate therapy, yet with osteopenia-induced insufficiency fracture. Such presentations remain uncommon and may lead to delayed diagnosis or misdiagnosis as musculotendinous thigh pain. Our report supports the growing view that exclusion of pathology with MRI in atypical thigh pain is warranted – even in non-osteoporotic demographics – if clinical suspicion exists. Early imaging allowed timely management, pain resolution, and fracture consolidation without surgical risks.
In this case, a 45-year-old premenopausal woman without any history of trauma or bisphosphonate use presented with insidious, activity-related proximal thigh pain. Initial radiographs were unremarkable, making early diagnosis challenging. MRI played a crucial role by revealing a non-displaced subtrochanteric stress fracture with surrounding marrow edema, allowing timely intervention. Conservative management – including strict non-weight-bearing initially, gradual progression to partial weight-bearing, physiotherapy, and calcium and vitamin D supplementation – led to complete fracture healing and full restoration of function within six months, without the need for surgical intervention. This case demonstrates that even in low-risk, premenopausal individuals with mild osteopenia, subtrochanteric stress fractures can occur, and early recognition with MRI followed by carefully supervised conservative treatment can result in successful outcomes.
Limitations
This single-case report cannot be generalized to other premenopausal women. Objective assessment of mechanical load or biomechanics was not performed, and follow-up was limited to six months, so long-term outcomes remain unknown. The absence of a comparative treatment arm and detailed metabolic or genetic evaluation further limits conclusions about causative factors and optimal management.
Subtrochanteric stress fractures can occur even in premenopausal women without major risk factors, such as trauma or bisphosphonate use. Persistent, unexplained proximal thigh pain warrants early MRI evaluation when radiographs are normal. Timely diagnosis and conservative management can result in complete healing and avoid unnecessary surgical intervention.
References
- 1. Daffner RH, Pavlov H. Stress fractures: Current concepts. AJR Am J Roentgenol 1992;159:245-52. [Google Scholar] [PubMed]
- 2. Hulkko A, Orava S. Stress fractures in athletes. Int J Sports Med 1987;8:221-6. [Google Scholar] [PubMed]
- 3. Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: A potential complication of alendronate therapy. J Clin Endocrinol Metab 2005;90:1294-301. [Google Scholar] [PubMed]
- 4. Goh SK, Yang KY, Koh JS, Wong MK, Chua SY, Chua DT, et al. Subtrochanteric insufficiency fractures in patients on alendronate therapy: A caution. J Bone Joint Surg Br 2007;89:349-53. [Google Scholar] [PubMed]
- 5. Lenart BA, Lorich DG, Lane JM. Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med 2008;358:1304-6. [Google Scholar] [PubMed]
- 6. Neviaser AS, Lane JM, Lenart BA, Edobor-Osula F, Lorich DG. Low-energy femoral shaft fractures associated with alendronate use. J Orthop Trauma 2008;22:346-50. [Google Scholar] [PubMed]
- 7. Kim TY, Lee YK, Lee Y, Jang S, Lee HJ, Cho HM, et al. Low-energy subtrochanteric and diaphyseal femoral fractures in patients without bisphosphonate exposure: A report of three cases. Bone Joint J 2015;97-B:510-4. [Google Scholar] [PubMed]
- 8. Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med 1995;23:472-81. [Google Scholar] [PubMed]
- 9. Gaeta M, Minutoli F, Scribano E, Ascenti G, Vinci S, Bruschetta D, et al. CT and MR imaging findings in athletes with early tibial stress injuries: Comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology 2005;235:553-61. [Google Scholar] [PubMed]
- 10. Bush LA, Chew FS. Subtrochanteric femoral insufficiency fracture in woman on bisphosphonate therapy for glucocorticoid-induced osteoporosis. Radiol Case Rep 2009;4:232. [Google Scholar] [PubMed]
- 11. Chew FS, Bui-Mansfield LT. Subtrochanteric femoral stress fracture in a young adult: CT and MRI correlation. AJR Am J Roentgenol 2003;180:1515-7. [Google Scholar] [PubMed]
- 12. Shin WC, Lee SM, Lee JH, Suh KT. Spontaneous insufficiency fracture of the femur in a middle-aged patient without bisphosphonate use. Clin Orthop Surg 2012;4:251-4. [Google Scholar] [PubMed]
- 13. Vannabouathong C, Schemitsch EH. Subtrochanteric femur fractures: Review of fixation and outcomes. Orthop Clin North Am 2015;46:85-97. [Google Scholar] [PubMed]
- 14. Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med 2011;364:1728-37. [Google Scholar] [PubMed]